Last Updated on November 26, 2025 by Bilal Hasdemir
Being told you have cancer is a big change, and it’s important to have your loved ones with you. A prostate biopsy is a key step in finding out more about your condition. It can be hard both physically and emotionally. Many patients wonder about the prostate biopsy necessity and whether it’s truly required.
Medical procedures like biopsies can make you feel unsure and scared, but understanding their purpose can ease those worries. We will look into why a prostate biopsy is important, what happens during it, and what patients can expect. Knowing this helps you make confident, informed choices about your health.
Key Takeaways
- Understanding the role of a prostate biopsy in diagnosis.
- The importance of having support during the diagnosis process.
- Exploring the necessity and implications of undergoing a biopsy.
- What to expect during and after the procedure.
- The significance of informed decision-making in healthcare.
Understanding Prostate Biopsy
It’s key for patients to know about prostate biopsy if they might have prostate cancer. A prostate biopsy takes tissue from the prostate gland for tests.
What is a prostate biopsy?
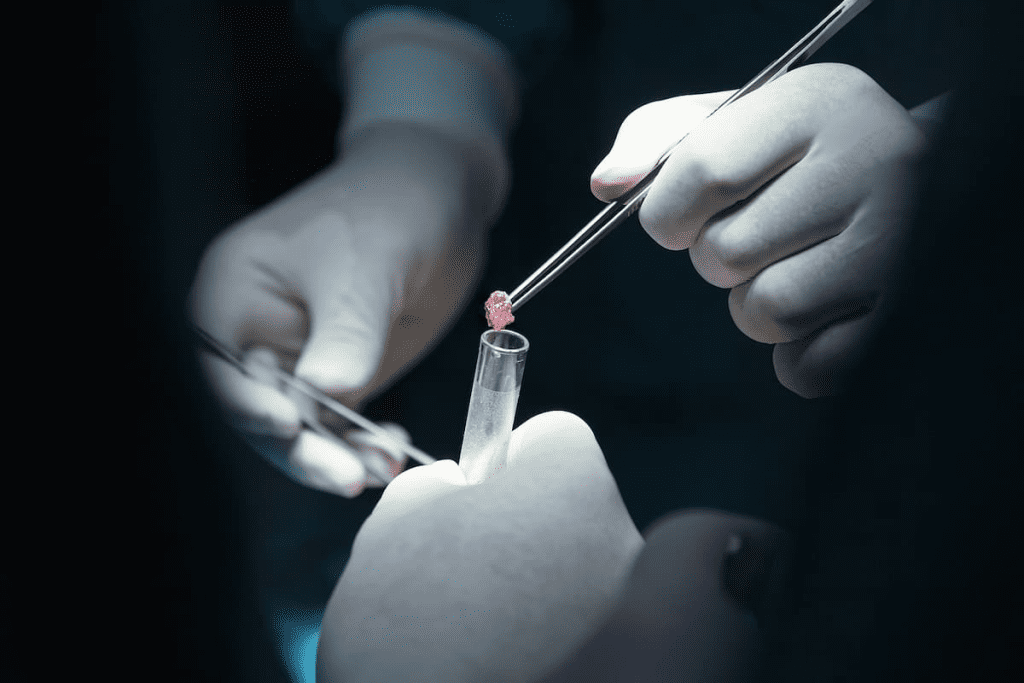
A prostate biopsy checks for cancer in the prostate. A urologist uses a special tool to take tissue samples. These are then looked at under a microscope for cancer cells. Doctors usually do a biopsy after other tests show possible problems. For example, Kevin Webber, a 49-year-old dad, was diagnosed with stage 4 prostate cancer. This shows how important accurate tests like biopsies are.
Types of prostate biopsies
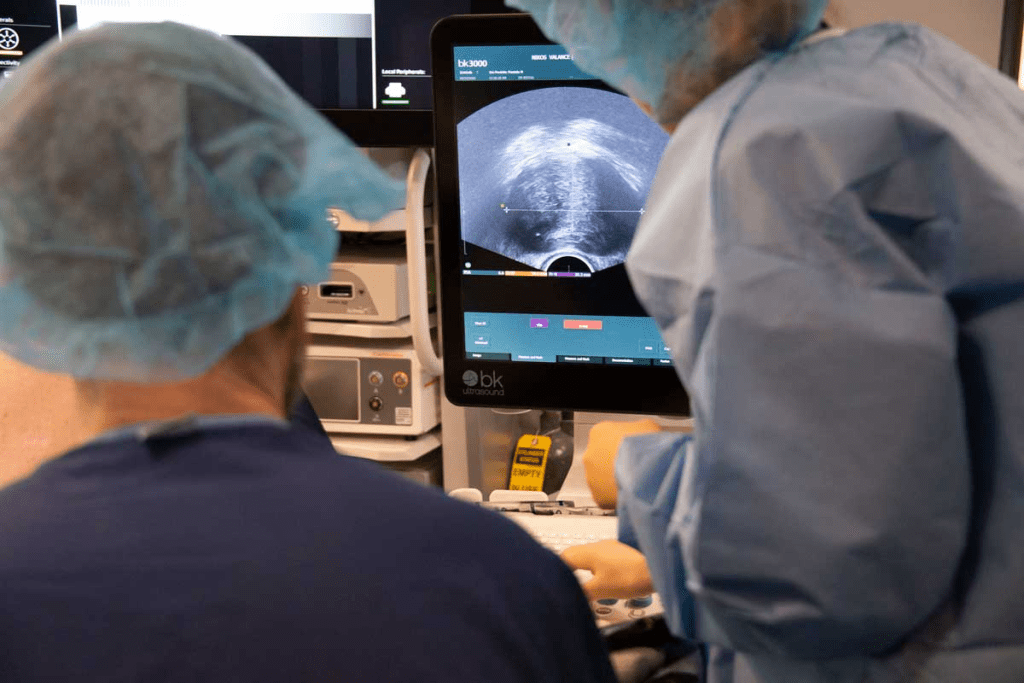
There are different types of prostate biopsies. The most common is the transrectal ultrasound-guided biopsy (TRUS). This uses an ultrasound probe in the rectum to guide the needle. The transperineal biopsy is another type. It uses a needle through the perineum, between the scrotum and anus. This method is less common but useful in some cases. There are also advanced methods like MRI-ultrasound fusion biopsy. It uses MRI images with ultrasound to find specific areas in the prostate. This can make the biopsy more accurate by focusing on the most suspicious spots.
The Purpose of Prostate Biopsies
Prostate biopsies are key in finding and managing prostate cancer. They help doctors understand the disease’s nature. This is more than just a test; it’s a vital step.
Diagnosing Prostate Cancer
The main goal of a prostate biopsy is to find prostate cancer. Doctors look at prostate tissue to see if cancer is there. A survivor said, “The biopsy was a turning point for me. It gave me a clear diagnosis that helped shape my treatment.”
“The diagnosis of prostate cancer through biopsy is a critical step that allows for timely and appropriate treatment,”
It shows how important it is to get a correct diagnosis.
Determining Cancer Aggressiveness
Biopsies also show how aggressive the cancer is. This is important because it tells doctors how fast the cancer might grow. Knowing how aggressive the cancer is helps choose the right treatment.
Guiding Treatment Decisions
The results of a biopsy are key for deciding treatment. Knowing the cancer’s presence and how aggressive it is helps doctors pick the best treatment. This way, care is tailored to each patient’s needs. We consider many factors, like the patient’s health and what they prefer. In short, prostate biopsies are vital for finding prostate cancer, figuring out how aggressive it is, and deciding on treatment. This approach ensures patients get the best care possible.
When Doctors Recommend a Prostate Biopsy
Doctors suggest a prostate biopsy for several reasons. These reasons show a possible risk of prostate cancer. They help find who might need a biopsy to get early care.
Elevated PSA Levels
High Prostate-Specific Antigen (PSA) levels often lead to a biopsy. PSA is a protein from the prostate gland. High levels might mean cancer, but not always. We look at PSA levels with other factors. These include age, health, and past PSA tests. A big change in PSA levels is more worrying than a single high reading. We also check how fast PSA levels are changing.
Abnormal Digital Rectal Exam (DRE)
An abnormal digital rectal exam (DRE) might also lead to a biopsy. A DRE checks the prostate for lumps or irregularities. Not all findings are cancer, but they can be a sign. An abnormal DRE, with high PSA levels, makes a biopsy more likely. It helps find the cause of the abnormality.
Previous Suspicious Findings
Previous tests or biopsies with suspicious cells or lesions might need a biopsy. This is true if the suspicious area has changed or if previous biopsies showed HGPIN or ASAP.
Family History Considerations
A family history of prostate cancer is a big risk factor. Men with a first-degree relative (father or brother) with prostate cancer are at higher risk. This risk grows with more affected relatives. We think about family history when deciding on a biopsy. This is true for men with other risk factors. By looking at these factors, we decide if a prostate biopsy is needed. It’s a choice that weighs early detection against the biopsy’s risks and discomforts.
Prostate Biopsy Necessity: When Is It Truly Required?
To know when a prostate biopsy is needed, we look at current practices and guidelines. The decision depends on several factors. These include clinical guidelines, risk assessment, and age and life expectancy.
Clinical Guidelines for Biopsy Necessity
Clinical guidelines are key in deciding if a prostate biopsy is needed. They are based on research and aim to standardize diagnosis. The American Urological Association and the European Association of Urology advise on when a biopsy is necessary. These guidelines help doctors find patients at high risk of prostate cancer who should get a biopsy. PSA levels are a big part of these guidelines. High PSA levels might mean cancer, but they can also mean other issues. Doctors look at many things, like age, family history, and past biopsy results, to understand PSA levels.
Risk Stratification Approaches
Risk stratification is important in deciding on a prostate biopsy. It involves looking at different risk factors. These include age, family history, ethnicity, and past PSA test results. By looking at these factors, doctors can figure out who would really benefit from a biopsy.
- Age: Older men are at a higher risk of prostate cancer.
- Family History: Men with a family history of prostate cancer are considered higher risk.
- Ethnicity: Certain ethnic groups have a higher incidence of prostate cancer.
Age and Life Expectancy Considerations
Age and life expectancy are big factors in deciding on a prostate biopsy. For older men or those with a short life expectancy, the risks of a biopsy might outweigh the benefits. The goal is to avoid unnecessary procedures in men who may not benefit from treatment due to their age or health status. For example, men who are expected to live a long time might benefit from early cancer detection and treatment. On the other hand, men with serious health issues or a short life expectancy might not benefit from a biopsy. The risks might be too high compared to the benefits.
Official Guidelines for Prostate Biopsy
Official guidelines are key in guiding prostate biopsy and cancer detection. These are made by top medical groups to standardize care. They help ensure patients get the right diagnosis and treatment.
American Urological Association Recommendations
The American Urological Association (AUA) sets guidelines for when a prostate biopsy is needed. These are based on the latest research and clinical evidence. They consider PSA levels, digital rectal exam findings, and patient risk factors. According to the AUA, a biopsy is recommended for men with high PSA levels or abnormal digital rectal exam results. The guidelines also look at the patient’s health, life expectancy, and personal preferences.
European Association of Urology Guidelines
The European Association of Urology (EAU) also has guidelines on prostate cancer diagnosis, including biopsy recommendations. The EAU guidelines stress the importance of risk stratification in deciding on a biopsy. These guidelines suggest that the decision to perform a biopsy should be based on PSA levels, PSA density, digital rectal exam findings, and other risk factors. This includes family history and ethnicity.
NCCN Guidelines for Prostate Cancer Early Detection
The National Cancer Network (NCCN) provides detailed guidelines for early prostate cancer detection. These guidelines include recommendations for prostate biopsy based on risk assessment.The NCCN guidelines categorize patients into different risk groups. This is based on PSA levels, Gleason score (if previous biopsy), and other clinical factors. The guidelines recommend biopsy for men at higher risk of prostate cancer. To show the differences and similarities between these guidelines, we have summarized the key recommendations in the table below:
| Guideline | PSA Threshold for Biopsy | Risk Factors Considered | Biopsy Recommendation |
| AUA | Elevated PSA | PSA level, DRE, patient health | Recommended for high-risk patients |
| EAU | PSA density, elevated PSA | PSA density, DRE, family history, ethnicity | Based on risk stratification |
| NCCN | Varies by risk group | PSA level, Gleason score, other clinical factors | Recommended for higher risk groups |
By following these official guidelines, healthcare providers can make informed decisions about when to recommend a prostate biopsy. This ensures patients receive appropriate care based on the latest clinical evidence.
The PSA Test and Its Limitations
The Prostate-Specific Antigen (PSA) test is key in checking prostate health. But, its limits are often talked about by doctors. We use the PSA test to first check for prostate cancer. It’s important to know what it can and can’t do.
Understanding PSA Levels
PSA levels are measured in nanograms per milliliter (ng/mL) of blood. A PSA level below 4 ng/mL is usually normal. But, levels above 4 might show prostate problems, like cancer. Yet, a high PSA doesn’t always mean cancer; it can also show non-cancerous issues. PSA levels can change for many reasons. For example, PSA levels can go up after some medical tests or if the prostate gets bigger. This shows we need to look at PSA test results carefully.
Factors That Affect PSA Readings
Many things can change PSA readings, making it not perfect for diagnosing alone. These include:
- Age: PSA levels go up as we get older.
- Prostate size: A bigger prostate can raise PSA levels.
- Prostatitis: Inflammation of the prostate can also raise PSA.
- Recent prostate procedures or exams: Some tests can temporarily raise PSA levels.
- Ejaculation: Ejaculating recently can slightly raise PSA levels.
Knowing these factors helps us understand PSA test results better. It’s not just the number; it’s how we see that number.
PSA Test vs. Biopsy: What Each Reveals
The PSA test and biopsy are used in different ways to find prostate cancer. The PSA test gives a first look at prostate health. But, a biopsy directly looks at prostate tissue to confirm cancer. A biopsy can tell us if cancer is there and how aggressive it is. This info is key for choosing treatment. The PSA test, on the other hand, helps figure out who needs more tests. In short, the PSA test is useful for prostate cancer screening, but we must understand its limits. By knowing what affects PSA levels and using it with other tests like biopsy, we can better care for our prostate health.
Prostate Biopsy Accuracy and Detection Rates
Prostate biopsies are key in finding cancer. They help doctors diagnose and treat prostate cancer. How well they work is very important.
Standard Biopsy Detection Rates
Standard biopsies take random samples from the prostate. This method is common but not perfect. It can miss cancers, mainly small ones or those in hard-to-reach spots. The success of standard biopsies depends on several things. For example, taking more samples can help find cancer. But, it also raises the risk of complications.
Targeted Biopsy Accuracy
Targeted biopsies use imaging to focus on suspicious areas. This method is better at finding important cancers. They work well because they target likely cancer spots. This is great for people who have had negative biopsies but are worried about cancer.
False Negatives and Sampling Errors
Even with better biopsies, false negatives and errors can happen. A false negative means a biopsy misses cancer that’s there. Errors can be due to many things. For example, if the sample is not big enough or if the tumor is in a hard spot. Knowing these issues helps both patients and doctors understand biopsy results better.
| Biopsy Type | Detection Rate | Advantages | Limitations |
| Standard Biopsy | Variable | Widely used, established technique | May miss significant cancers |
| Targeted Biopsy | Higher for significant cancers | Improved detection of clinically significant cancers | Requires advanced imaging |
Knowing the good and bad of different biopsies helps patients make better choices about their health.
The Problem of False Positives and Overdiagnosis
Prostate cancer screening saves lives but faces challenges like false positives and overdiagnosis. It’s key to grasp these issues to improve patient care and outcomes.
Understanding False Positive Results
False positives happen when tests show prostate cancer when it’s not there. This can be due to many reasons, like PSA levels from non-cancerous conditions. Knowing why false positives occur helps us lessen their effect on patients.
Receiving a false positive can start a chain of unnecessary tests, causing worry and stress. We must think about the chance of false positives when we look at screening results to avoid too much intervention.
Overdiagnosis Concerns
Overdiagnosis means finding prostate cancer that won’t cause symptoms or death. This is a big issue with screening, leading to treatments that might not be needed. Finding the right cancers to treat is a big challenge. Overdiagnosis can harm patients with treatments they don’t need. We must find a balance between early detection and avoiding overdiagnosis for the best care.
Psychological Impact of False Positives
The mental toll of false positives is real. Patients often feel anxious and stressed, impacting their life quality. It’s vital to think about the mental effects of screening results and support those affected. Healthcare providers play a big role in easing the mental burden of false positives. By explaining things clearly and supporting patients, we can help them deal with these challenges.
MRI Before Biopsy: A Game-Changer?
Multiparametric MRI is becoming a key tool in prostate cancer diagnosis before biopsy. It uses several MRI sequences to give a detailed view of the prostate gland.
The Role of Multiparametric MRI
Multiparametric MRI is vital in spotting serious prostate cancer. It combines different MRI types, like T2-weighted and diffusion-weighted imaging. This helps doctors find and understand prostate lesions better.
- Improved Detection: Multiparametric MRI boosts finding serious prostate cancer.
- Better Characterization: It helps figure out how aggressive prostate cancer is.
- Risk Stratification: This imaging helps sort out risks, guiding treatment choices.
MRI vs. Biopsy: Complementary Approaches
MRI and biopsy work together in prostate cancer diagnosis. While biopsy is the main way to diagnose, MRI offers extra insights before it.
Key Benefits of MRI Before Biopsy:
- It spots cancerous areas for focused biopsies.
- It aids in planning treatments based on risk.
- It might cut down on unnecessary biopsies.
MRI-Guided Targeted Biopsies
MRI-guided targeted biopsies are a big step forward in prostate cancer diagnosis. They let urologists take precise samples from specific MRI-identified spots. The precision of MRI-guided targeted biopsies can lead to better cancer detection. It also means spotting fewer low-risk cancers, which could lower overtreatment.
Advanced Biopsy Technologies
Advanced biopsy technologies are changing how we find prostate cancer. They aim to get better at spotting cancer, cut down on unneeded tests, and help patients more. Let’s look at some new methods that are making a big difference in prostate biopsy.
MRI-Ultrasound Fusion Biopsy
MRI-ultrasound fusion biopsy is a big step forward in finding prostate cancer. It mixes MRI’s detailed pictures with ultrasound’s live view. This way, doctors can better find and take samples from cancer spots. Studies show it helps find important prostate cancer better.
Transperineal vs. Transrectal Approaches
For a long time, doctors used a transrectal biopsy, going through the rectum. But, the transperineal method, going through the perineum, is becoming more popular. It might be safer and get to more of the prostate.
- Transrectal Approach: Traditional method, higher risk of infection.
- Transperineal Approach: Lower infection risk, potentially more accurate.
Saturation Biopsy Techniques
Saturation biopsy takes many samples from the prostate. It’s great for people with high PSA levels or other cancer signs, even if past biopsies were negative. It can be done in two ways. Taking more samples helps doctors find cancer if it’s there.
“Saturation biopsy techniques have become an essential tool in the diagnosis of prostate cancer, even when initial biopsies are negative.”
As we keep improving biopsy tech, it’s key to understand each method’s good and bad sides. This helps us give the best diagnosis and treatment plan to patients.
Alternatives to Immediate Biopsy
If a prostate biopsy isn’t needed right away, there are other options. These choices can give important info or help watch the condition closely.
Active Surveillance Protocols
Active surveillance is for men with low-risk prostate cancer. It lets them avoid or delay treatment’s side effects. They get regular check-ups to watch for cancer growth.
“Active surveillance is great for men with low-risk prostate cancer,” – A top urologist. “It keeps their quality of life high while watching the cancer.” This includes regular PSA tests, exams, and imaging studies.
Biomarker Tests
Biomarker tests are another choice instead of a biopsy. They look at genetic or molecular markers in blood or urine. This gives more info on cancer risk, helping make better choices.
- The Prostate Health Index (phi) combines three PSA tests for better cancer detection.
- The 4Kscore test looks at four kallikrein markers in blood to predict aggressive cancer.
- The PCA3 test checks a specific gene in urine to assess cancer risk.
Repeat PSA Testing
Repeat PSA testing is a simple way to watch prostate health. It tracks PSA level changes. Doctors can see trends that might mean a biopsy is needed. PSA testing alone isn’t enough. It’s part of a bigger plan. PSA velocity, or how fast PSA levels change, is key to understanding prostate health. Exploring these options helps patients and doctors decide on a biopsy. This ensures the choice fits the patient’s health and wishes.
Risks and Complications of Prostate Biopsies
Patients need to know about the risks and complications of prostate biopsies. The procedure is usually safe, but there are possible side effects to be aware of.
Infection Risks
One major risk is infection. The biopsy involves a needle through the rectum into the prostate. This can introduce bacteria into the urinary tract or prostate gland. To lower this risk, we often give antibiotics before and after the procedure. Even with these precautions, some patients might get infections. These can range from mild urinary tract infections to severe prostatitis.
Bleeding Complications
Bleeding is another risk. It can show up as blood in semen, urine, or stool. Most bleeding is minor and goes away in a few days. But sometimes, bleeding can be more serious and need medical help. We take steps to reduce bleeding risks. Patients with bleeding disorders or on anticoagulant medications are at higher risk.
Pain and Discomfort
While many men feel little discomfort during the procedure, some may feel pain or discomfort. We use local anesthesia and sedation to help with pain. After the procedure, some men might feel pain or discomfort in the prostate area. This usually goes away in a few days.
Long-term Side Effects
Long-term side effects are rare but can include discomfort, erectile dysfunction, or urinary issues. Research is ongoing to understand and reduce these risks.
| Complication | Frequency | Typical Management |
| Infection | 1-5% | Antibiotics |
| Bleeding | 2-10% | Observation, sometimes hospitalization |
| Pain/Discomfort | Variable | Pain management medications |
| Long-term side effects | Rare | Varies depending on the effect |
Knowing about these risks and complications helps patients make informed decisions about prostate biopsies. We work closely with our patients to assess their risk factors and provide the best care.
The Biopsy Procedure: What to Expect
Getting a prostate biopsy can feel scary, but knowing what happens can help. We’ll walk you through what to expect, from getting ready to feeling better afterward. This way, you’ll know what to expect every step of the way.
Preparation for a Prostate Biopsy
Before the biopsy, you’ll do some prep work. This might include:
- Stopping certain medications that could interfere with the procedure, such as blood thinners
- Undergoing a bowel preparation to cleanse your rectum
- Receiving antibiotics to minimize the risk of infection
It’s very important to follow your doctor’s instructions carefully. This helps make sure the procedure goes well and keeps risks low.
During the Procedure
A prostate biopsy takes small tissue samples from your prostate gland. It’s usually done with:
- Transrectal ultrasound-guided biopsy, where a probe is inserted into your rectum
- Local anesthesia to reduce discomfort
The whole thing usually takes 15 to 30 minutes. You might feel some pressure or discomfort during the biopsy, but it’s usually not painful.
Recovery and Aftercare
After the biopsy, you might feel some side effects, such as:
- Bleeding or blood in your semen, urine, or stool
- Pain or discomfort in the rectum or lower abdomen
| Common Side Effects | Duration | Action |
| Bleeding | A few days to a week | Contact your doctor if heavy or persistent |
| Pain/Discomfort | A few days | Use pain relievers as directed by your doctor |
Most men can get back to normal in a day or two. It’s very important to follow your doctor’s aftercare instructions. This helps you recover smoothly.
Shared Decision Making: Discussing Biopsy with Your Doctor
Deciding on a prostate biopsy is a big step. It’s important to talk it over with your doctor. This way, you can make a choice that feels right for you. You’ll discuss if the biopsy is needed, learn about the procedure, and think about your own risks and preferences.
Questions to Ask Your Urologist
When you talk to your urologist about a prostate biopsy, ask the right questions. This helps you understand the reasons and what might happen next. Some key questions are:
- What are the reasons for recommending a biopsy?
- What are the possible risks and complications of the procedure?
- How will the biopsy results affect my treatment choices?
- Are there other tests that could give similar information?
These questions help you grasp the doctor’s advice and what to expect. This way, you can make a choice that feels right for you.
Weighing Personal Risk Factors
Your personal risks are important when deciding on a biopsy. Things like family history, age, and past PSA test results matter. Talk these over with your doctor to see how they affect your choice.
| Risk Factor | Description | Impact on Decision |
| Family History | Having a first-degree relative diagnosed with prostate cancer | Increases the risk; may necessitate earlier or more frequent screening |
| Age | Risk increases with age, specially after 50 | Older men may be more likely to benefit from biopsy if other risk factors are present |
| Previous PSA Results | Elevated or rising PSA levels over time | May indicate a need for biopsy to assess cancer risk |
Incorporating Your Preferences and Values
Your personal preferences and values are key in making this decision. Think about how you feel about uncertainty, how a diagnosis might change your life, and what treatment you might prefer if cancer is found. For example, some men might choose active surveillance for low-risk cancer. Others might prefer more aggressive treatment. Talking about these choices with your doctor helps make sure the decision fits your overall well-being.
Conclusion
Deciding if a prostate biopsy is needed is a big choice. It depends on PSA levels, digital rectal exam results, and overall health. We’ve looked at the different types of biopsies, MRI’s role, and the guidelines urologists use. A prostate biopsy isn’t right for everyone. The decision should consider individual risk factors, medical history, and personal choices. Talking to a healthcare provider helps men make informed decisions about their prostate health. The main goal of a prostate biopsy is to find cancer early. This makes treatment easier. By understanding what a biopsy can and can’t do, men can take charge of their health. They can work with their healthcare team to create a plan that’s right for them.
FAQ
What is a prostate biopsy, and why is it necessary?
A prostate biopsy takes tissue samples from the prostate gland. It helps diagnose prostate cancer and decide on treatment.
How accurate is a prostate biopsy?
The accuracy of a prostate biopsy varies. It depends on the type of biopsy and the doctor’s skill. Standard biopsies detect cancer in 40% to 80% of cases. Targeted biopsies are more accurate.
What are the risks and complications associated with prostate biopsies?
Prostate biopsies can cause infection, bleeding, and pain. They may also lead to long-term issues like urinary incontinence or erectile dysfunction.
What are the alternatives to immediate prostate biopsy?
Alternatives include active surveillance, biomarker tests, and repeat PSA testing. These options are for patients with low-risk cancer or uncertain diagnoses.
How does MRI compare to biopsy in prostate cancer diagnosis?
MRI can spot suspicious areas before a biopsy. It guides targeted biopsies or complements them. MRI-ultrasound fusion biopsy is a cutting-edge method for precise sampling.
What are the official guidelines for prostate biopsy?
Guidelines come from the American Urological Association and the European Association of Urology. The NCCN also offers recommendations for early detection.
How do I prepare for a prostate biopsy?
Preparation includes stopping certain medications and bowel preparation. You’ll also get antibiotics to reduce infection risk. Your doctor will give you specific instructions.
What happens during a prostate biopsy procedure?
A healthcare provider uses a needle to take tissue samples from the prostate. The procedure is done under local anesthesia to reduce discomfort.
What are the signs that I may need a repeat prostate biopsy?
You might need a repeat biopsy if your PSA levels keep rising. Or if previous results were unclear. Your doctor may also suggest it if they suspect cancer despite a negative biopsy.
How do I discuss prostate biopsy with my doctor?
Discuss the need for a biopsy, risks, and benefits with your urologist. Consider your personal risk factors and preferences. This helps make informed decisions.
What is the role of PSA testing in prostate cancer diagnosis?
PSA testing detects elevated levels that may indicate cancer. But, a biopsy is often needed to confirm the diagnosis.
Can a prostate biopsy detect cancer aggressiveness?
Yes, a biopsy can determine cancer aggressiveness. It analyzes tissue samples for cancer cells and their characteristics.
Are there different types of prostate biopsies?
Yes, there are different types. Standard, targeted, and MRI-ultrasound fusion biopsies each have their own benefits and uses.
References
- American Urological Association. (2009). Early Detection of Prostate Cancer: AUA Guideline. https://www.auanet.org/guidelines-and-quality/guidelines/early-detection-of-prostate-cancer-guidelines