Did you know over 200,000 men are diagnosed with prostate cancer each year in the United States? A prostate biopsy is key in finding this cancer early. It helps doctors start treatment right away.
Getting a biopsy can seem scary. But knowing about it helps. It’s a test that takes tissue from the prostate gland. Then, doctors check for cancer cells.
Learning about how a prostate biopsy is done helps patients get ready. It also helps them make smart choices about their health.
Key Takeaways
- A prostate biopsy is a test to find prostate cancer.
- The test takes tissue from the prostate gland.
- Knowing about the biopsy helps patients make good choices.
- Early detection leads to better treatment and outcomes.
- A prostate biopsy is vital for diagnosing prostate cancer.
Understanding Prostate Biopsy: What Is It?

Definition of Prostate Biopsy

A prostate biopsy removes tissue from the prostate gland. This tissue is then checked under a microscope for cancer or other issues. It’s a vital step in finding prostate cancer and other problems.
“The biopsy is a critical diagnostic tool that helps in identifying the presence and severity of prostate cancer,” says a renowned urologist. This statement highlights the biopsy’s role in prostate cancer diagnosis.
Types of Prostate Biopsies
There are different prostate biopsy methods:
- Transrectal Biopsy: This is the most common, where the needle goes through the rectum.
- Transperineal Biopsy: Here, the needle goes through the area between the scrotum and anus.
- MR-guided Biopsy: This uses MRI images to guide the needle to the right spot.
Why Is a Prostate Biopsy Performed?
A prostate biopsy is done for several reasons, mainly to find or rule out prostate cancer. It’s often suggested when:
- PSA (Prostate-Specific Antigen) levels are high.
- Abnormalities are found during a digital rectal exam (DRE).
- Previous biopsies showed precancerous cells or other issues.
Understanding why a prostate biopsy is needed can ease worries and prepare patients for the process.
The Risks Associated with Prostate Biopsy
Prostate biopsy is usually safe, but it can have risks and complications. We will look at these risks to help patients know what to expect.
Common Complications
Common issues with prostate biopsy include bleeding, infection, and trouble with urination. Bleeding can happen during or after the procedure. It might even lead to serious problems. Infection is another risk, which can be treated with antibiotics but needs quick medical care if symptoms don’t go away.
- Bleeding or hematoma
- Infection or sepsis
- Temporary urinary difficulties or retention
- Pain or discomfort during or after the procedure
Rare but Serious Risks
There are serious but rare risks with prostate biopsy. These include severe infection, major bleeding needing hospital care, and damage to nearby areas. It’s important for patients to talk to their doctor about these risks to understand the chances and effects.
|
Rare but Serious Risks |
Description |
|---|---|
|
Severe Infection |
Can lead to sepsis, a life-threatening condition if not promptly treated. |
|
Significant Bleeding |
May require hospitalization or further medical intervention. |
|
Damage to Surrounding Structures |
Potential injury to nearby organs or tissues during the biopsy. |
Psychological Impact of Biopsy Results
The emotional impact of biopsy results is significant. Patients waiting for results often feel anxious. The news can deeply affect their mental health. It’s key to have support from healthcare providers, family, and friends during this time.
Getting a diagnosis after a prostate biopsy can be tough. We stress the need for a support system and clear communication with healthcare providers. This helps address any worries or fears patients might have.
Alternatives to Prostate Biopsy
Not everyone needs a traditional prostate biopsy. There are other ways to check for prostate health. Some doctors might suggest watching health signs closely instead.
Active Surveillance
Active surveillance is for men with low-risk prostate cancer. It means watching the cancer closely with tests and exams.
This approach can avoid the risks of biopsy and treatments. But, it needs a lot of trust in the monitoring process.
MRI-guided Biopsy
MRI-guided biopsy uses MRI scans to guide the biopsy. It helps find cancer more accurately. This reduces the chance of missing important cancer cells.
With MRI guidance, doctors can better see where and how big the cancer is. This helps plan better treatments.
Other Diagnostic Tests
There are other tests that can help check prostate health without a biopsy. These include:
- PSA testing: Checks the prostate-specific antigen in the blood.
- PCA3 test: Looks for PCA3, a gene linked to prostate cancer, in urine.
- 4Kscore test: Uses four biomarkers to predict aggressive prostate cancer risk.
|
Diagnostic Test |
Description |
Benefits |
|---|---|---|
|
Active Surveillance |
Monitoring PSA levels and other indicators for low-risk prostate cancer |
Avoids or delays biopsy complications |
|
MRI-guided Biopsy |
Combines MRI imaging with biopsy for accurate targeting |
Improves detection of significant cancers |
|
PSA Testing |
Measures prostate-specific antigen levels in the blood |
Non-invasive, early detection |
These options give patients and doctors choices for prostate health. Knowing the pros and cons helps make better decisions about care.
Understanding PSA Levels and Their Role
PSA testing is a simple blood test that checks the prostate-specific antigen in your blood. This test gives insights into your prostate health. Prostate-specific antigen, or PSA, is a protein made by the prostate gland. Elevated levels of PSA can mean prostate cancer, but also other non-cancerous conditions.
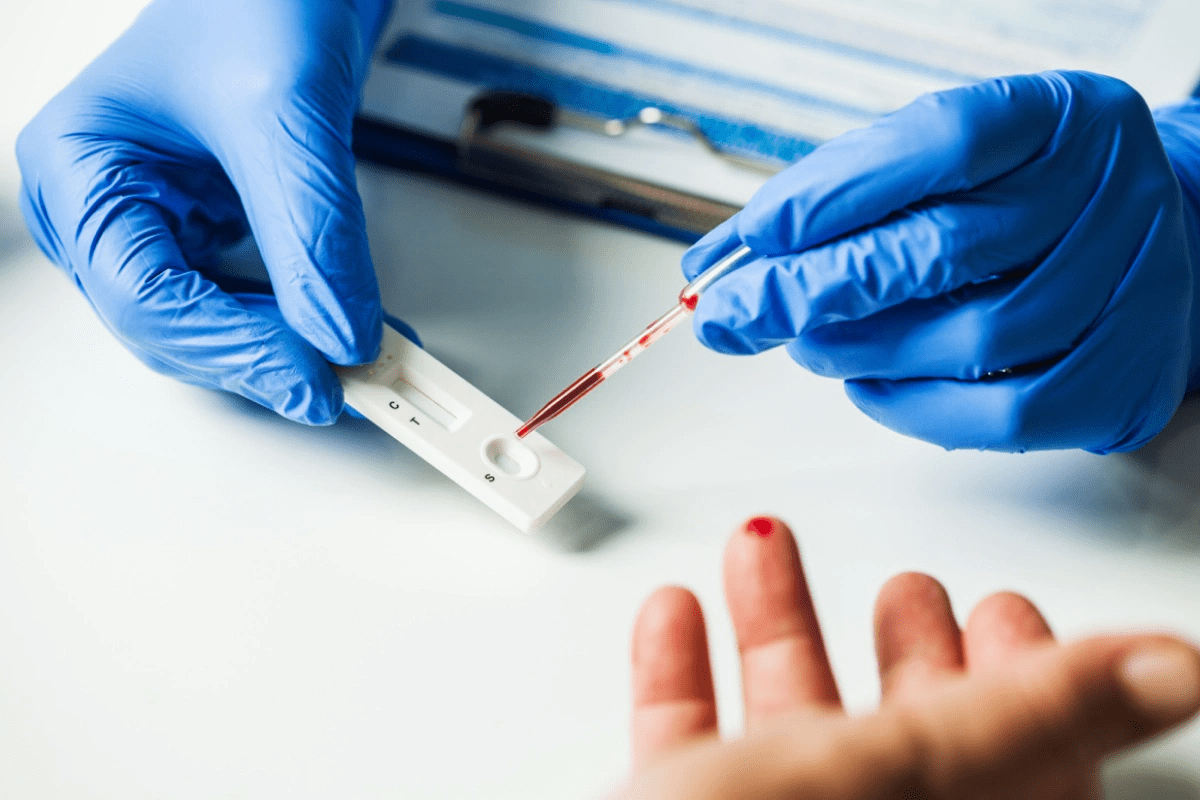
What Is PSA Testing?
PSA testing measures the PSA level in your blood. It’s a key tool for screening prostate cancer and keeping an eye on prostate health. The test is easy and just involves a blood sample, which is then checked in a lab.
PSA is made by both cancerous and non-cancerous cells in the prostate. A normal PSA level is okay, but high levels can mean trouble. Knowing about PSA levels is key for accurate diagnosis and treatment.
How PSA Levels Influence Decisions
PSA test results can shape decisions about more tests, like a biopsy. High PSA levels might lead a doctor to suggest a biopsy to check for cancer. Low PSA levels can be reassuring, but regular checks are needed.
PSA levels also help check if treatments for prostate cancer are working. A drop in PSA levels after treatment is a good sign.
Limitations of PSA Testing
PSA testing is helpful but has its limits. False positives can cause worry and extra tests. Also, some men with prostate cancer might have normal PSA levels. This shows we need a full approach to prostate health.
Some things, like not ejaculating for 30 days before a test, can affect PSA levels. Not ejaculating before a test can help avoid false readings. Knowing this can help men get ready for PSA tests and understand their results better.
Evaluating the Need for a Biopsy
To decide if a prostate biopsy is needed, it’s important to look at a patient’s symptoms and medical history. The choice to get a biopsy depends on many things. These include the patient’s health, symptoms, and results from tests like PSA (Prostate-Specific Antigen) testing.
Symptoms that Indicate a Biopsy
Some symptoms might mean a prostate biopsy is needed. These include:
- Difficulty urinating or painful urination
- Blood in the urine or semen
- Painful ejaculation
- Frequent urination, often at night
A urologist will look at these symptoms and the patient’s health. They will decide if a biopsy is needed. For example, they might check if symptoms affect the patient’s life and if they point to a serious issue, like how a urologist examines your ejaculation to check for abnormalities.
Factors Influencing the Decision
Many things can affect the decision to do a prostate biopsy. These include:
|
Factor |
Description |
Impact on Decision |
|---|---|---|
|
PSA Levels |
Elevated PSA levels can indicate prostate issues. |
High PSA levels may necessitate a biopsy. |
|
Family History |
A family history of prostate cancer. |
Increases the likelihood of recommending a biopsy. |
|
Age |
Risk of prostate cancer increases with age. |
Older men are more likely to be recommended for a biopsy. |
Consultation with Healthcare Providers
Talking to healthcare providers is key when thinking about a biopsy. Patients should share their symptoms, medical history, and any worries about the biopsy. Providers will use this info to decide if a biopsy is right.
It’s vital for patients and providers to talk openly. This way, all important factors are considered when deciding on a prostate biopsy.
Patient Experiences: Real-Life Stories
Every person’s journey through prostate biopsy is unique. The outcomes can vary a lot. We’ve collected stories from patients who have gone through this procedure. These stories show the different experiences and how the results affect their lives.
Positive Outcomes
For some, prostate biopsy leads to early cancer detection and treatment. John’s story is one example: “I was diagnosed with prostate cancer after my biopsy. Thanks to early detection, I was able to undergo treatment and recover successfully.”
These positive stories highlight the role of prostate biopsy in prostate health. Some patients find the procedure minimal discomfort. Others see it as a key part of their cancer treatment.
|
Patient Profile |
Biopsy Experience |
Outcome |
|---|---|---|
|
Age 55, family history of prostate cancer |
Minimal discomfort, quick recovery |
Negative for cancer |
|
Age 62, elevated PSA levels |
Some discomfort, managed with pain relief |
Positive for cancer, underwent treatment |
|
Age 50, abnormal DRE |
Minimal pain, returned to normal activities quickly |
Negative for cancer, continued surveillance |
Negative Outcomes
Not all experiences with prostate biopsy are positive. Some men face complications like infection or perineum lump. One patient said, “After my biopsy, I experienced significant pain and discomfort, which took several weeks to resolve.”
While these negative outcomes are rare, they are concerning. It’s vital to talk about risks and complications with healthcare providers. This ensures informed decisions.
Psychological Repercussions of Results
The psychological impact of prostate biopsy results can be big. Patients may feel anxious, fearful, or relieved, depending on their diagnosis and treatment plan.
We know how important emotional support is for patients. By sharing real-life stories, we aim to create a sense of community. This helps those going through this challenging time.
The Financial Implications of Prostate Biopsy
Understanding the financial side of prostate biopsy is key for making good choices. The cost of a prostate biopsy can be a big worry for patients. It’s important to think about these costs when deciding if a biopsy is needed.
Average Costs in the U.S.
The cost of a prostate biopsy in the U.S. can vary a lot. This depends on where you are, who your healthcare provider is, and your insurance. On average, it can cost between $1,000 to $3,000 or more for an outpatient procedure. This includes the biopsy, pathology fees, and other related costs.
Insurance Coverage Considerations
Insurance coverage is a big factor in how much you’ll pay for a prostate biopsy. Most insurance plans cover the cost of necessary biopsies. But, how much they cover can differ. It’s a good idea to check your insurance policy to know what you might have to pay.
Cost-Effectiveness of Alternatives
There are other tests, like MRI-guided biopsy, that might be cheaper for some patients. These options could mean you don’t need a more invasive procedure and save money. But, how cost-effective they are depends on your situation and insurance.
We suggest talking to your healthcare provider about your financial worries and insurance. This way, you can make the best choice for your care.
Timing and Frequency of Biopsies
Prostate biopsy guidelines suggest specific timing and frequency based on risk factors and medical history. It’s key for patients and healthcare providers to understand these guidelines. This helps in making informed decisions about prostate health.
Recommended Guidelines
The American Urological Association (AUA) and other groups offer guidelines for prostate biopsies. These guidelines look at PSA levels, digital rectal exams, family history, and past biopsy results.
Men with a high-risk profile, like a family history of prostate cancer, may need more frequent biopsies. On the other hand, those with a low-risk profile might have biopsies less often.
Recommended Biopsy Frequency Based on Risk Profile
|
Risk Profile |
Recommended Biopsy Frequency |
|---|---|
|
Low Risk |
Every 2-3 years |
|
Intermediate Risk |
Every 1-2 years |
|
High Risk |
Every 6-12 months |
When to Consider Repeat Biopsies
Repeat biopsies are needed when a patient’s condition changes or previous results are unclear. For example, if a patient’s PSA level keeps rising after a negative biopsy, another biopsy might be necessary.
Men with HGPIN or ASAP in the past may also need repeat biopsies. This is to watch for any signs of cancer.
Monitoring Post-Biopsy Conditions
After a prostate biopsy, patients are watched for complications like infection or bleeding. Healthcare providers also check PSA levels and perform DREs to see if prostate health has changed.
It’s important for patients to follow their post-biopsy instructions closely. They should tell their healthcare provider about any symptoms that worry them. This ensures quick action if complications arise.
Future of Prostate Biopsy Techniques
The world of prostate biopsy is about to change a lot. New technologies and methods are coming. It’s important to know about these changes for better prostate cancer diagnosis.
Innovations in Biopsy Techniques
New biopsy methods are making the process better and less painful. Robotic-assisted biopsies and fusion biopsy techniques are getting more popular. They help find cancer spots more accurately and with less discomfort.
Artificial intelligence (AI) and machine learning (ML) are also helping. AI can spot cancer cells that humans might miss. This could lead to catching cancer earlier.
Research in Less Invasive Methods
Scientists are working on making biopsies easier and more accurate. They’re looking into liquid biopsies, which check blood or urine for cancer signs. This could mean fewer surgeries for patients.
Imaging technologies like MRI and ultrasound are also key. They help doctors see the prostate better. This makes biopsies more precise.
Role of Technology in Diagnosis
Technology is becoming more important in finding prostate cancer. Advanced imaging techniques and diagnostic software are making biopsies better. Telemedicine is also helping, making it easier to see specialists online.
As tech keeps getting better, so will prostate biopsy methods. This will lead to better care and more tailored treatment for patients.
Addressing Myths and Misconceptions
Many myths and misconceptions surround prostate biopsy. These can cause unnecessary worry and confusion. We aim to clear up these myths and share the truth about prostate biopsy.
Common Misunderstandings About Biopsies
One big myth is that prostate biopsies are very painful. While some discomfort is possible, most men find it only mildly painful. Effective pain management strategies help reduce this discomfort.
Another myth is that biopsy results are often unclear or wrong. But, thanks to better biopsy techniques and pathology, results are now much more accurate.
Scientific Evidence vs. Perceptions
Scientific evidence is key to understanding prostate biopsy. Research shows that prostate biopsy is a safe procedure with a low risk of serious problems. Yet, many people think it’s riskier than it is.
“The safety and efficacy of prostate biopsy have been well-documented in medical literature, yet misconceptions persist.”
It’s important to compare what science says with what people think. By knowing the truth, patients can make better choices about their health.
|
Myth |
Fact |
|---|---|
|
Prostate biopsy is very painful. |
Most men experience mild discomfort; effective pain management is available. |
|
Biopsy results are often inaccurate. |
Advances in biopsy techniques have improved result accuracy. |
How Media Influences Public Opinion
The media greatly influences what people think about prostate biopsy. Sensationalized stories can spread myths, while fair reporting can educate. It’s vital to provide accurate, unbiased information.
We need to think about how media affects what patients believe. By sharing the truth, we can help patients make informed health choices.
Support Resources for Patients
Patients going through prostate biopsy can find help from many places. These resources make the journey easier. They offer more than just the procedure itself.
Guidance from Healthcare Providers
Getting help from healthcare providers is key. They address concerns and guide patients personally. Our team is here to offer care that is both caring and knowledgeable.
Connecting through Online Communities
Online forums are great for sharing stories and asking questions. They connect patients with others who have gone through the same thing.
Empowering through Education
Learning about your condition and treatment is empowering. We give patients access to reliable information. This helps them understand their situation better.
With these resources, patients feel more in control and supported. They are better equipped to face their prostate biopsy journey.
FAQ
What is a prostate biopsy?
A prostate biopsy is a procedure where doctors take a tissue sample from the prostate gland. This is done to check for prostate cancer or other issues.
What are the different types of prostate biopsies?
There are several types of prostate biopsies. These include transrectal and transperineal biopsies. Each has its own way of doing things and benefits.
Why is a prostate biopsy performed?
A prostate biopsy is done to find prostate cancer. It helps figure out how serious the cancer is. It also helps decide on treatment.
What are the possible risks and complications of prostate biopsy?
There are risks like bleeding and infection. There can also be temporary problems with urination.
What are the alternatives to traditional prostate biopsy?
Alternatives include active surveillance and MRI-guided biopsy. Other tests can also help watch prostate health without a biopsy right away.
How does PSA testing relate to prostate biopsy?
PSA testing checks prostate health. High PSA levels might mean a biopsy is needed to check for cancer.
What factors influence the decision to have a prostate biopsy?
Decisions are based on symptoms, health, PSA levels, and talking to doctors.
What are the financial implications of prostate biopsy?
The cost of a prostate biopsy varies. Insurance can affect how much you pay out of pocket.
How often should prostate biopsies be repeated?
How often depends on health, PSA levels, and past biopsy results.
What are the future directions in prostate biopsy techniques?
New technology and methods are making biopsies more precise and less invasive.
How can patients cope with the psychological impact of biopsy results?
Support from doctors, online groups, and educational materials can help with the emotional side of biopsy results.
What are the benefits of not ejaculating for 30 days?
Some studies suggest not ejaculating for 30 days might affect PSA levels. But more research is needed to understand this.
How does a urologist examine ejaculation?
A urologist might check ejaculation as part of a full check-up of prostate and urinary health.
What is anal intraepithelial neoplasia?
Anal intraepithelial neoplasia is abnormal cell growth in the anal canal. It can be a sign of anal cancer.
What is the role of a rectal tube in a prostate biopsy procedure?
A rectal tube or ultrasound probe helps guide the needle during a transrectal biopsy into the prostate gland.
How is a prostate biopsy performed?
The procedure uses a needle to take tissue samples from the prostate gland. It’s often guided by ultrasound or MRI.
What are semen pills, and are they related to prostate health?
Semen pills are supplements for male fertility or sexual function. But their effect on prostate health is not clear.
Where is PSA located?
PSA (Prostate-Specific Antigen) is a protein made by the prostate gland. Its levels can be checked in the blood.
What is a perineum lump, and could it be related to prostate issues?
A perineum lump could be due to infections or cysts. A healthcare provider can evaluate it.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36865012/