Last Updated on November 26, 2025 by Bilal Hasdemir

When you’re diagnosed with prostate cancer, you worry about the pain it might bring. Some specialists note that prostate cancer impacts patients emotionally and mentally, highlighting the need to address these feelings.
Knowing how much pain prostate cancer can cause is key to managing it well. We’ll look at the disease’s stages and how they affect pain levels. This will give you a better understanding of what patients go through.
Key Takeaways
- Understanding the level of pain associated with prostate cancer is key to managing it.
- The disease’s stages affect pain levels differently.
- Prostate cancer symptoms can really hurt a patient’s quality of life.
- It’s vital to address the emotional and mental impact of prostate cancer.
- Managing prostate cancer pain well needs a complete approach.
Understanding Prostate Cancer and Pain
Prostate cancer and pain are closely linked, but many don’t understand this well. Pain isn’t always caused by the cancer itself. It can also come from treatment or other factors.
The Relationship Between Cancer and Pain
Cancer pain, like that from prostate cancer, can come from different sources. The tumor can press on nerves, bones, or organs, causing pain. Treatments like surgery, chemotherapy, or radiation can also lead to pain.
It’s important to know these causes for good prostate cancer pain management. Pain is different for everyone. It depends on the cancer stage, overall health, and how well someone can handle pain. Finding the right pain management is key to improving life for prostate cancer patients.
Misconceptions About Prostate Cancer Pain
There are many wrong ideas about prostate cancer pain. One is that pain is always part of having cancer. But, not everyone with cancer feels pain, even in the early stages.
Another wrong idea is that pain always comes from the tumor. But, pain can also come from treatments or other health problems. Knowing this helps us find better prostate cancer pain relief options for each person.
Also, prostate pain causes can be different for everyone. Some pain comes from the cancer itself, while others come from treatment or other health issues. By clearing up these wrong ideas, we can offer better support and care for those with prostate cancer.
Early-Stage Prostate Cancer and Pain Levels
Localized prostate cancer might not always hurt. But knowing about possible discomfort is key. We’ll look into the pain linked with early-stage prostate cancer. This helps both patients and doctors make better choices.
Is Localized Prostate Cancer Painful?
Early-stage prostate cancer often doesn’t hurt much. The cancer stays in the prostate gland, and symptoms might be small or none. Yet, some men could feel pain or discomfort because of the tumor or other reasons.
It’s important to tell apart common discomfort and real pain. Discomfort might be from urinary problems or other issues. But real pain is sharp, stabbing, or aching and lasts.
Common Discomfort vs. Actual Pain
Knowing the difference between common discomfort and real pain is key. Discomfort might feel like pressure or mild pain in the pelvic area. It could be from many things, not just prostate cancer. But real pain is worse and lasts longer, affecting daily life a lot.
Men with early-stage prostate cancer might feel some discomfort. But how much pain they feel can really vary. Things like where the tumor is, how big it is, and the person’s health play a big role.
By understanding these details, patients can talk better with their doctors. This leads to better management and treatment plans.
Advanced and Metastatic Prostate Cancer Pain

Patients with advanced prostate cancer often face more pain. This pain is hard to manage. It happens when the cancer grows and affects different parts of the body.
Why Advanced Prostate Cancer Causes Pain
Advanced prostate cancer causes pain because the tumor grows. It affects tissues and organs around it. This can lead to discomfort and pain.
The pain can also come from metastasis. This is when cancer spreads to other parts of the body. It can go to bones, lymph nodes, or other organs. The pain pattern depends on where and how much it spreads.
Metastatic Prostate Cancer Pain Patterns
Metastatic prostate cancer pain patterns change based on where the cancer spreads. Often, it spreads to bones, causing bone pain.
Bone pain is a big worry for those with metastatic prostate cancer. It can feel like a dull ache or sharp pain. It usually happens in the back, hips, or ribs. The pain can get worse if not treated right.
To understand metastatic prostate cancer pain better, let’s look at common pain patterns:
| Site of Metastasis | Pain Characteristics |
| Bones | Dull ache or sharp pain, often in the back, hips, or ribs |
| Lymph Nodes | Discomfort or pain in the groin, pelvis, or abdomen |
| Other Organs | Varies depending on the organ involved; can include abdominal pain, neurological symptoms, etc. |
Knowing these pain patterns is key to managing pain well. Healthcare providers can tailor treatments to match the pain’s cause. This improves patient outcomes and quality of life.
Prostate Cancer Pain Symptoms by Location
Prostate cancer pain can show up in different parts of the body. It’s important to know where it can happen. As the cancer grows, it can cause pain in many areas, making life harder for those affected.
Pelvic Pain
Pelvic pain is common in men with prostate cancer. It can feel like a dull ache or sharp pains in the pelvic area. The pain might stay the same or get worse with sitting or bowel movements.
Pelvic pain from prostate cancer happens when the tumor presses on nerves and tissues. Men with ongoing pelvic pain should see their doctor for a check-up.
Back Pain
Back pain is also linked to prostate cancer, often when it spreads to the spine bones. This pain can feel like a dull ache or sharp pain in the lower back, sometimes going to the legs.
It’s important to tell if back pain is from prostate cancer or other reasons like muscle strain or degenerative disc disease. Men with new or getting worse back pain should tell their healthcare team.
Bone Pain
Bone pain happens when prostate cancer spreads to bones. Common places include the spine, pelvis, and ribs. The pain is often severe, feeling like a deep ache or tenderness in the bones.
“Bone pain from prostate cancer can significantly impact a man’s quality of life, making it essential to manage effectively with the help of healthcare professionals.”
Abdominal Pain
Abdominal pain from prostate cancer is less common but can happen. It’s often due to cancer in lymph nodes in the abdomen or other issues. This pain can feel like a dull ache or cramping in the stomach area.
Men with abdominal pain should get medical help to find out the cause and treatment.
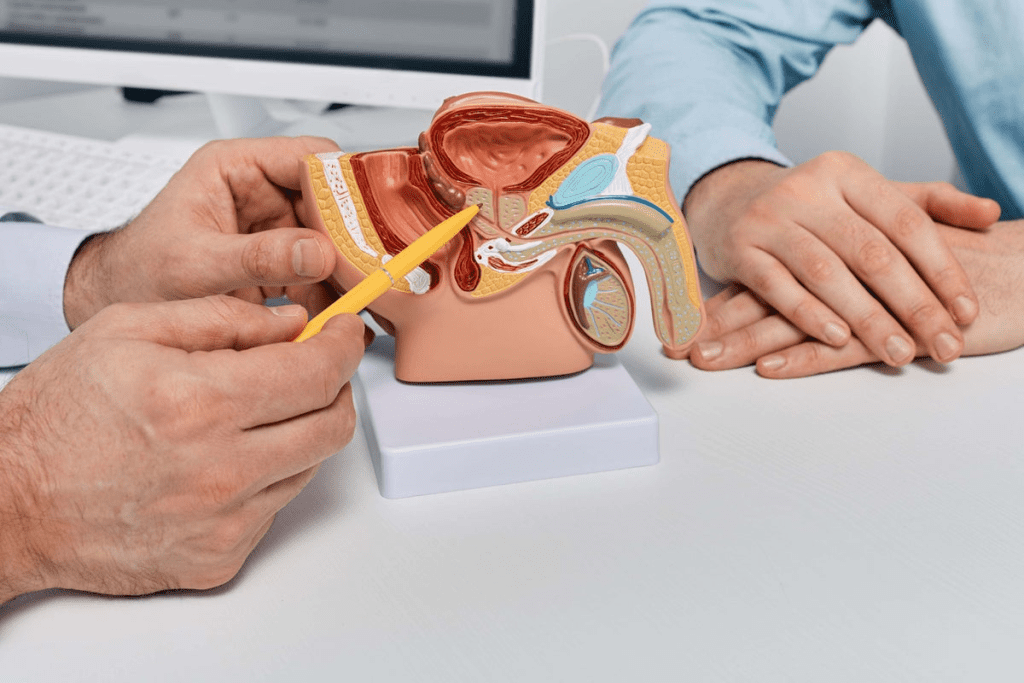
Pain During Urination and Other Urinary Symptoms
Prostate cancer can really mess with your urinary health. It can cause pain when you pee. As the cancer grows, it can make your urinary system uncomfortable and lead to other problems.
Causes of Painful Urination in Prostate Cancer
There are a few reasons why prostate cancer patients might feel pain when they pee. The tumor can block the urine flow, causing irritation and pain in the urethra. Treatments like radiation or surgery can also cause urinary symptoms.
Common causes include:
- Tumor obstruction
- Inflammation or infection
- Treatment side effects
Distinguishing Prostate Cancer from Other Urinary Conditions
It’s important to tell the difference between prostate cancer symptoms and symptoms from other conditions. UTIs and BPH can also make peeing painful. But, if you see blood in your pee or lose a lot of weight, it might be prostate cancer.
| Symptom | Prostate Cancer | UTI/BPH |
| Painful Urination | Possible, if tumor is blocking | Common |
| Blood in Urine | Possible | Rare, unless infection is bad |
| Frequency/Urgency | Common | Very Common |
Knowing the differences is key to getting the right treatment. If you’re having urinary problems, see a doctor to figure out why.
Nerve Pain Associated with Prostate Cancer
It’s important to know why and how nerve pain happens in prostate cancer patients. This pain comes from nerve damage caused by the cancer. It’s called neuropathic pain.
How Prostate Cancer Affects Nerves
Prostate cancer can harm nerves around the prostate gland. As it grows, it can invade these nerves, causing pain. This pain can also come from treatments like surgery or radiation.
Nerve damage from prostate cancer can cause pain, numbness, or tingling. How much damage happens depends on the cancer’s stage and where it is.
Recognizing Neuropathic Pain Symptoms
Neuropathic pain from prostate cancer can show up in many ways. Common signs include:
- Sharp, shooting, or burning pain
- Numbness or tingling sensations
- Chronic pain that lasts a long time
- Pain that gets worse with light touch or cold
Spotting these signs is key to diagnosing neuropathic pain. Doctors use patient history, physical checks, and tests to find the cause of nerve pain.
| Symptom | Description |
| Sharp, shooting pain | Sudden, intense pain that may spread along the nerve |
| Numbness or tingling | Abnormal feelings from nerve damage |
| Chronic pain | Long-lasting pain that affects daily life |
Managing neuropathic pain needs a team effort. This includes medicine, physical therapy, and sometimes special procedures. Knowing the causes and signs of nerve pain helps patients and doctors create a good pain plan.
Prostate Cancer Pain at Night
Prostate cancer pain can be tough at night, making it hard to sleep well. Many things can make pain worse at night. Knowing what these are can help manage the pain.
Why Pain Often Worsens at Night
There are several reasons why prostate cancer pain gets worse at night. The body’s natural rhythm can affect how we feel pain. Also, without daytime distractions, we notice pain more at night. Plus, lying down can put extra pressure on painful areas, making it hurt more.
Strategies for Better Sleep Despite Pain
To manage prostate cancer pain at night, we need a few strategies. Here are some ways to improve sleep:
- Using a comfortable mattress and pillows to support the body
- Maintaining a consistent sleep schedule
- Engaging in relaxation techniques, such as deep breathing or meditation, before bedtime
- Avoiding stimulating activities and electronic screens before sleep
It’s also important to work with healthcare providers to manage pain. They can help adjust medication or find other ways to improve sleep.
| Strategy | Description | Benefits |
| Comfortable Sleeping Environment | Using a supportive mattress and pillows | Reduces pressure on painful areas |
| Relaxation Techniques | Deep breathing, meditation, or gentle stretches before bed | Helps in reducing stress and promoting relaxation |
| Consistent Sleep Schedule | Going to bed and waking up at the same time daily | Improves overall sleep quality |
By using these strategies and working with healthcare providers, patients can manage their pain at night. This can lead to better sleep and a better quality of life.
Factors Affecting Prostate Cancer Pain Levels
Prostate cancer pain varies from person to person. This is because many factors can influence how pain is felt. Understanding these factors is key to managing pain effectively.
Several elements affect the pain levels in prostate cancer patients. These include the cancer’s stage and grade, how much pain a person can handle, and any other health issues they might have.
Cancer Stage and Grade
The stage and grade of prostate cancer greatly impact pain levels. Advanced cancer often causes more pain because it spreads to other parts of the body. Dr. Smith, a renowned oncologist, notes that this spread can lead to more pain in bones and other areas.
A higher grade of cancer means the tumor is more aggressive. This can also lead to more pain. It’s important for doctors to understand this relationship to manage pain well.
Individual Pain Tolerance
How much pain a person can handle varies a lot. Age, health, and mental state can all play a role. A study on pain management found that pain tolerance is very personal and can be influenced by many things.
It’s important to understand and assess each person’s pain tolerance. This helps tailor pain management plans to fit their needs.
Comorbid Conditions
Having other health issues can also affect pain levels. Conditions like diabetes, arthritis, or heart disease can make pain harder to manage. Research shows that these conditions can greatly impact a person’s quality of life and pain.
It’s vital to manage these conditions well to help with prostate cancer pain. Doctors need to look at the patient’s overall health when planning treatment.
“The interplay between prostate cancer, comorbid conditions, and individual pain tolerance creates a complex pain experience that requires a multifaceted management approach.”
” Expert in Palliative Care
Prostate Cancer Pain Management
Managing pain well is key to a better life for prostate cancer patients. It’s not just about the physical pain. It also includes emotional and psychological aspects.
Medical Pain Management
Medical pain management is a big part of treating prostate cancer pain. It uses medicines to help with pain. Non-opioid analgesics like acetaminophen and NSAIDs work for mild to moderate pain.
For more severe pain, opioid medications might be used. But, they are chosen carefully because of possible side effects.
Adjuvant medications, used for other health issues, can also help with pain. For example, some antidepressants and anticonvulsants can treat neuropathic pain.
Interventional Procedures
When medicines alone don’t work, interventional procedures might be needed. These include nerve blocks, where a local anesthetic or steroid is injected around a nerve. This blocks pain signals.
Other procedures might use neuromodulation techniques, like spinal cord stimulation. These are done by pain management specialists and can offer a lot of relief.
Complementary and Alternative Methods
There are also other ways to manage prostate cancer pain. Acupuncture, massage therapy, and cognitive-behavioral therapy can help. They can make pain better and improve overall well-being.
It’s important for patients to talk to their healthcare provider about these options. This way, they can find the best pain management plan.
Prostate Cancer Pain Medications
Managing prostate cancer pain is key to improving life quality for patients. Many medications help ease this pain. The right choice depends on the pain’s severity and type.
Non-Opioid Analgesics
Non-opioid analgesics are often the first choice for prostate cancer pain. These include over-the-counter drugs like acetaminophen and NSAIDs like ibuprofen. Acetaminophen works for mild to moderate pain. NSAIDs reduce inflammation and ease pain.
“Non-opioid analgesics are a cornerstone in pain management,” says Dr. Smith, a pain management specialist. “They are effective for many patients and have a relatively favorable side effect profile when used appropriately.”
Opioid Medications
For severe pain, opioid medications are used. These are strong pain relievers for moderate to severe pain. But, they can lead to dependency and have side effects like constipation and drowsiness.
Opioid medications should be used carefully and under a healthcare provider’s guidance. “The goal is to use the lowest effective dose for the shortest duration necessary,” emphasizes Dr. Johnson, an oncologist.
Adjuvant Medications
Adjuvant medications are not mainly pain relievers but can help with certain pains. For example, anticonvulsants and certain antidepressants can manage nerve pain from prostate cancer.
- Anticonvulsants like gabapentin can help with neuropathic pain.
- Antidepressants such as amitriptyline may be used for nerve pain.
- Corticosteroids can reduce inflammation and swelling.
Managing Medication Side Effects
While medications offer relief, they can also have side effects. It’s important to manage these to keep the patient’s quality of life good. Common side effects include nausea, constipation, and drowsiness.
To lessen these effects, patients can:
- Stay hydrated to help reduce the risk of constipation.
- Take medications with food to minimize stomach upset.
- Adjust dosages or timing under the guidance of a healthcare provider.
Effective pain management is not just about the right medication. It’s also about a complete approach to reduce side effects and increase patient comfort.
Radiation and Other Treatments for Prostate Cancer Pain
Radiation therapy and other treatments are key in managing prostate cancer pain. They help improve life quality for patients. It’s important to know how they work.
Radiation Therapy for Pain Relief
Radiation therapy is a common treatment for prostate cancer. It helps by shrinking tumors that cause pain.
There are two main types: external beam radiation therapy (EBRT) and brachytherapy. EBRT uses radiation from outside the body. Brachytherapy places radioactive material inside the prostate.
Benefits of Radiation Therapy:
- Reduces tumor size and pain
- Works for different cancer stages
- Offers non-invasive or minimally invasive options
| Type of Radiation Therapy | Description | Benefits |
| External Beam Radiation Therapy (EBRT) | Radiation delivered from outside the body | Non-invasive, effective for localized tumors |
| Brachytherapy | Radioactive material placed directly into the prostate | Highly targeted, minimizes damage to surrounding tissues |
Hormone Therapy and Pain
Hormone therapy, or androgen deprivation therapy (ADT), is another option. It lowers male hormones that help cancer grow.
Dr. Smith says, “Hormone therapy can manage prostate cancer pain by shrinking tumors and slowing disease growth.”
It can be used alone or with other treatments like radiation.
Key Considerations:
- Works for advanced or metastatic prostate cancer
- May have side effects
- Needs regular monitoring
Surgical Interventions for Pain
Surgery can also help with prostate cancer pain. It’s used when other treatments don’t work or are not possible.
Palliative surgery aims to ease symptoms and improve life quality, not cure cancer.
As we learn more about prostate cancer, a mix of treatments is often best for pain management.
End-Stage Prostate Cancer Pain
The final stages of prostate cancer can bring tough pain symptoms. These symptoms need careful attention. As the disease gets worse, the pain can change, needing a detailed pain management plan.
Pain Characteristics in Terminal Stages
In the end stages of prostate cancer, pain can get worse and more complex. It might come from the tumor growing, bone metastases, or other factors. Knowing the pain’s characteristics is key for managing it well.
Common pain characteristics include:
- Persistent pain in the pelvic area
- Radiating pain to the lower back or legs
- Sharp or stabbing pain due to nerve involvement
- Aching or discomfort in the bones
Palliative Care Approaches
Palliative care is vital for managing pain and improving life quality in end-stage prostate cancer patients. It uses a team approach to meet physical, emotional, and social needs.
| Palliative Care Measures | Description |
| Pain Medication | Use of analgesics to control pain effectively |
| Radiation Therapy | Targeted radiation to reduce tumor size and alleviate pain |
| Nerve Blocks | Procedures to interrupt pain signals to the brain |
Palliative care is more than just pain management. It also offers emotional and psychological support to patients and their families.
Supporting Patients and Families
Supporting patients and their families is a key part of care in the end stages of prostate cancer. It includes emotional support, counseling, and resources to help them deal with challenges.
We know how important a supportive care network is. It can include:
- Counseling services for patients and families
- Support groups to share experiences and coping strategies
- Resources for practical assistance, such as home care
By taking a full approach to pain management and support, we can enhance the quality of life for patients with end-stage prostate cancer and their loved ones.
Living with Prostate Cancer Pain
Prostate cancer pain is more than just physical. It also affects your emotions and mind. To manage it well, you need to tackle both the pain and its emotional side.
Psychological Impact of Chronic Pain
Chronic pain from prostate cancer can cause a lot of emotional stress. It can make you feel anxious and depressed. It also affects your mood, sleep, and life quality.
Managing the psychological impact is key. This includes:
- Counseling or therapy to deal with pain’s emotional side
- Mind-body techniques like meditation and deep breathing
- Support groups to share experiences and find support
One patient said, “Joining a support group was a turning point for me. It showed me I’m not alone in this journey.”
“The emotional toll of prostate cancer pain can be just as debilitating as the physical pain itself.”
Maintaining Function Despite Pain
It’s important to stay active despite prostate cancer pain. Regular exercise, adjusted to your ability, can help reduce pain and improve your mood.
Gentle exercises like yoga or short walks are good. It’s also key to keep in touch with your healthcare team to adjust your treatment as needed.
| Activity | Benefits |
| Yoga | Improves flexibility and reduces stress |
| Short walks | Enhances circulation and boosts mood |
Support Resources for Patients
There are many support resources for those with prostate cancer pain. These include:
- Online forums and support groups
- Counseling services for cancer patients
- Educational materials on pain management
Using these resources can help you cope better with prostate cancer pain. We suggest exploring these options and talking about them with your healthcare team.
When to Seek Medical Attention for Prostate Pain
Knowing when to see a doctor for prostate pain is key. Prostate cancer pain can change in intensity and type. It’s important to notice these changes to know when to get help.
Warning Signs That Require Immediate Care
Some symptoms of prostate pain need quick medical help. These include:
- Severe or getting worse pain that doesn’t get better with over-the-counter meds
- Pain with other signs like trouble peeing, blood in pee or semen, or fever
- Sudden, severe pain
- Pain spreading to the lower back, belly, or legs
If you see any of these signs, call your doctor right away. Quick action can greatly improve treatment and your life quality.
Communicating Effectively About Pain with Healthcare Providers
Talking well with your healthcare team is key for managing prostate pain. Here are some tips for the best care:
- Describe where, how bad, and what your pain feels like
- Keep a pain journal to track changes and patterns
- Share all meds and supplements you’re taking
- Tell your team about any worries or fears about your pain or treatment
Being open and detailed helps your healthcare team make better decisions for you. This teamwork can lead to better pain management plans that fit your needs.
Conclusion: Navigating the Journey of Prostate Cancer Pain
Dealing with prostate cancer pain is a unique and complex path. It’s important to understand the different types of pain to manage it well and improve life quality.
Managing this pain needs a full approach. This includes medical treatments, procedures, and other therapies. We’ve looked at how pain changes from early stages to more serious cases.
Patients should team up with their doctors to create a pain plan that fits them. This way, they can handle their pain better and keep living well.
Good pain care is vital for those with prostate cancer. We urge patients to talk openly with their doctors about their pain. This helps them get the support they need.
FAQ
What are the common pain symptoms associated with prostate cancer?
Prostate cancer can cause different types of pain. This includes pelvic pain, back pain, bone pain, and abdominal pain. These pains can come from the cancer itself or from treatments.
Is prostate cancer painful in the early stages?
Early prostate cancer might not always hurt. Some men might feel a bit uncomfortable, but real pain is rare in early stages.
Why does prostate cancer cause pain at night?
Nighttime pain from prostate cancer can be due to several reasons. These include less distraction, changes in how you sit, and hormonal changes. Using pain management and relaxation techniques can help sleep better.
What are the pain management options for prostate cancer?
There are many ways to manage prostate cancer pain. This includes medical treatments, interventional procedures, and alternative methods. Doctors might use non-opioid and opioid medications, along with other drugs, to help manage pain.
How does metastatic prostate cancer cause pain?
Metastatic prostate cancer can spread to bones, nerves, and other tissues. This can cause different types of pain, like bone pain and nerve pain.
What is the role of palliative care in end-stage prostate cancer?
Palliative care focuses on easing pain and symptoms in end-stage prostate cancer. Teams of palliative care professionals support patients and their families during this time.
How can I manage prostate cancer pain during urination?
Painful urination can be due to tumors or treatment side effects. It’s important to tell your doctor about these symptoms. They can help figure out the best treatment.
What are the warning signs that require immediate medical attention for prostate pain?
Severe pain, trouble urinating, or other concerning symptoms need immediate medical help. It’s key to talk openly with your doctor about your pain.
How can I maintain function despite prostate cancer pain?
To keep functioning with pain, use pain management strategies and make lifestyle changes. Work with your doctor to create a plan that helps you manage pain and live well.
What support resources are available for patients living with prostate cancer pain?
There are many resources, like counseling and support groups, to help with chronic pain’s mental impact. Doctors can guide you to these resources and help you access them.
Reference
- Cornford, P., et al. (2021). EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. European Urology, 79(2), 243-262. https://pubmed.ncbi.nlm.nih.gov/33696335/