Last Updated on November 26, 2025 by Bilal Hasdemir
Prostate exam guidelines have changed a lot in recent years, shaping how doctors screen for prostate cancer. The American Cancer Society and other medical groups have updated their recommendations, creating both discussion and confusion among patients and healthcare providers.
In the past, routine prostate exams were recommended for men over 50. However, the new prostate exam guidelines are more personalized. They now focus on individual risk factors, weighing the benefits and potential risks of screening.
These updated prostate exam guidelines reflect our growing understanding of prostate cancer. They help ensure that each man receives care that fits his unique health needs while avoiding unnecessary procedures.
Key Takeaways
- The American Cancer Society has updated its prostate screening recommendations.
- Modern guidelines emphasize individualized screening based on risk factors.
- The approach to prostate exams has become more nuanced.
- Understanding the benefits and harms of screening is key.
- Men over 50 should talk to their doctor about screening options.
The Evolution of Prostate Cancer Screening
Prostate exams were once key in cancer screening, but now guidelines have changed. The way we detect prostate cancer has changed a lot over the years. This is thanks to new medical tech and better understanding of the disease.
Historical Approach to Prostate Examinations
In the past, prostate examinations were common for men over a certain age. The main method was the digital rectal exam (DRE). This is when a doctor manually checks the prostate gland for any issues.
The DRE was simple and gave quick results. But, it’s not perfect for finding cancer early.
The Traditional Digital Rectal Exam (DRE) Procedure
The DRE involves a doctor putting a gloved finger in the patient’s rectum. This lets them feel the prostate gland. They check its size, shape, and texture for any signs of cancer.
But, the DRE has its downsides. It depends a lot on the doctor’s skill. It’s not always good at finding prostate cancer early.
When Prostate Exams Were Standard Practice
Prostate exams were once seen as essential for men’s health, as they got older. The idea was that finding cancer early could lead to better treatment and outcomes.
But, as more research came out, guidelines started to change. Now, screening is more tailored to each person’s risk and what they want.
Understanding the Decline in Routine Prostate Exams
A big change has happened in how doctors screen for prostate cancer. This change affects how often prostate exams are done. It’s due to new data, changes in medical views, and what patients want.
Statistical Trends in Prostate Examination Frequency
Studies have shown a big drop in prostate exams done each year. Data from the American Urological Association shows a big drop in digital rectal exams (DREs) for screening in certain age groups. This is because new guidelines suggest a more careful approach to screening.
The trend isn’t the same for everyone. It changes based on age, ethnicity, and where you live. For example, older men are more likely to get screened because they’re at higher risk. Younger men might not get screened unless they have a family history of prostate cancer.
Medical Community’s Shifting Perspective
The way doctors view prostate cancer screening has changed a lot. Evidence-based medicine means they now screen more carefully. They focus on men at higher risk and avoid unnecessary tests for those at lower risk. Groups like the American Cancer Society and the U.S. Preventive Services Task Force have updated their guidelines to reflect this.
This change is because doctors now understand the limits and risks of routine exams. They want to make sure men know the pros and cons of screening before they get a prostate exam.
Patient Preferences and Compliance Issues
What patients want is a big reason for fewer prostate exams. Many men don’t like DREs because they’re uncomfortable or worried about their accuracy. Patient education and shared decision-making are key. They help make sure screening matches what each patient values and prefers.
There are also issues with following guidelines because they can be complex. Men might get confused about when to get screened. This confusion can lead to fewer exams being done.
The Science Behind the Change in Screening Approaches
Prostate cancer screening methods have changed a lot due to new research. Studies have shown that old ways of screening aren’t as good as we thought. This has led to new guidelines and advice for doctors and patients.
Research Findings on Digital Rectal Exam Limitations
Digital Rectal Exams (DREs) have been key in finding prostate cancer for years. But, research has found big problems with this method. DREs often miss cancer and depend too much on the doctor doing the exam. They’re not as good at finding cancer as other tests.
Limitations of DRE:
- High rate of false negatives
- Operator-dependent
- Lower sensitivity and specificity compared to other methods
Evidence-Based Medicine and Screening Protocols
Using evidence-based medicine has changed how we screen for prostate cancer. Now, we focus on methods that have been proven to work. These changes come from careful studies and trials, making sure screening is safe and effective.
The U.S. Preventive Services Task Force (USPSTF) has played a key role in updating prostate cancer screening guidelines. They look at all the evidence to make sure screening helps more than it harms.
Risk-Benefit Analysis of Routine Prostate Exams
Understanding the risks and benefits of prostate exams is important. Finding cancer early is good, but we must also think about the downsides. For some men, regular exams might not be needed, as they’re at lower risk.
| Risk Category | Recommended Screening | Rationale |
| Low Risk | Less frequent or no screening | Lower risk of prostate cancer; possible overdiagnosis |
| High Risk | Regular screening | Higher risk of prostate cancer; early detection benefits outweigh risks |
In summary, the science behind changing prostate cancer screening is complex. It involves looking at old methods, adopting new evidence-based approaches, and weighing risks and benefits. These factors have led to new guidelines for screening prostate cancer.
PSA Testing: The Primary Alternative to Digital Rectal Exams
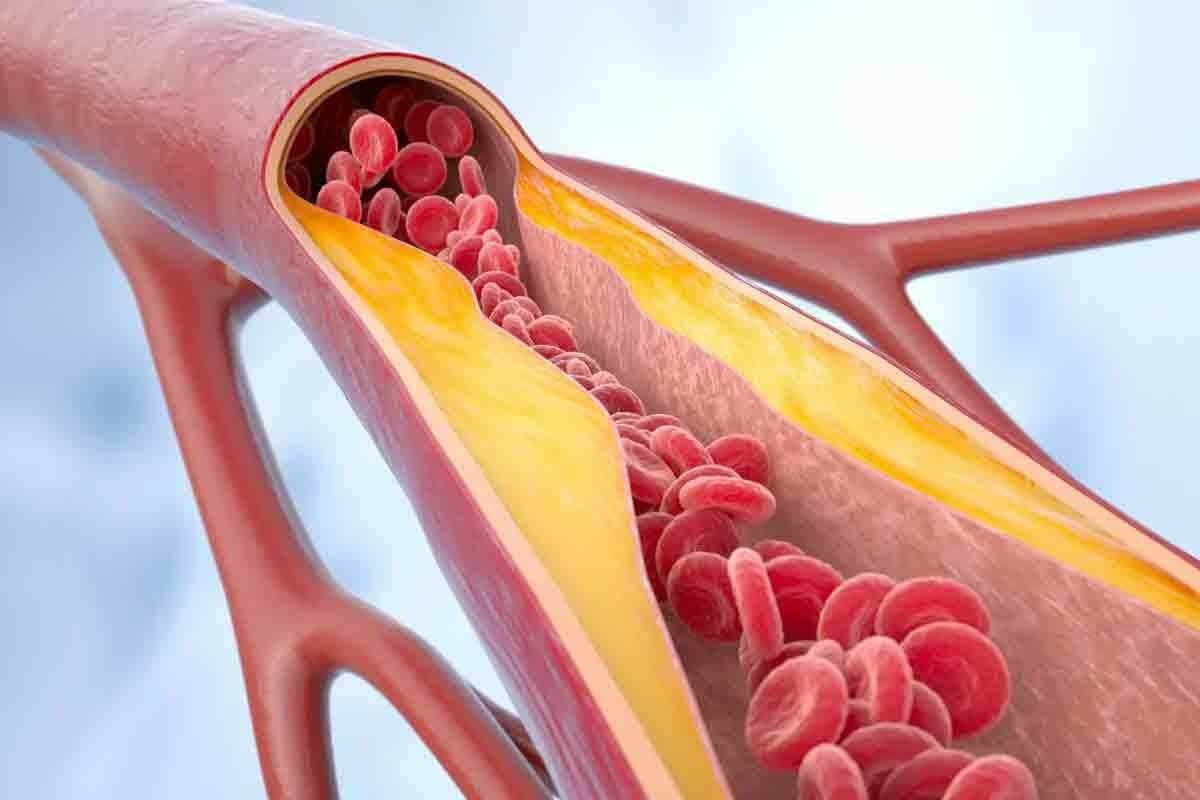
Recently, PSA testing has become a key method for prostate cancer screening. This change is because of the issues with traditional prostate exams.
How PSA Testing Works
PSA testing is a blood test that checks for a protein made by the prostate gland. High levels might mean cancer, but they can also show other issues like infections or BPH.
Key aspects of PSA testing include:
- It’s a simple blood test, making it less invasive than a digital rectal exam.
- Various factors, including age, race, and certain medical conditions can influence PSA levels.
- The test results require careful interpretation by a healthcare professional.
Advantages of Blood Tests Over Physical Examinations
PSA testing is less invasive and can be less uncomfortable than digital rectal exams. It also gives quantitative results that can be tracked over time. This helps in monitoring prostate health more precisely.
“The use of PSA testing has revolutionized the early detection of prostate cancer, making it more sensitive and less invasive than digital rectal exams.”
An Urologist
Limitations and Controversies of PSA Testing
PSA testing has its drawbacks. One big issue is the risk of overdiagnosis and overtreatment of prostate cancer. Some men might get treated for slow-growing tumors that wouldn’t have caused harm.
| Limitation | Description |
| False Positives | Elevated PSA levels not due to cancer, leading to unnecessary anxiety and further testing. |
| Overdiagnosis | Detection of cancers that are not life-threatening, potentially leading to overtreatment. |
| Lack of Specificity | PSA levels can be elevated due to non-cancerous conditions. |
Interpreting PSA Results
Understanding PSA test results is complex. It involves looking at the patient’s age, PSA velocity, and other health conditions. A healthcare provider can guide the next steps based on these factors.
It’s important to know the details of PSA testing for informed prostate cancer screening decisions. While it’s a good alternative, its limitations and controversies need to be considered.
Current Prostate Exam Guidelines from Major Medical Organizations
Major medical groups have updated their prostate exam guidelines. These changes reflect new research and clinical practices. They are key to understanding today’s prostate cancer screening standards.
American Cancer Society Recommendations
The American Cancer Society (ACS) says men should talk to their doctor about prostate cancer screening. This should start at age 50 for those at average risk. For those at higher risk, the talk should begin earlier.
For men with a family history of prostate cancer, this is at age 45. For men with multiple first-degree relatives diagnosed, it’s at age 40.
The ACS stresses the importance of making informed decisions. This includes considering personal preferences, values, and life expectancy.
American Urological Association Guidelines
The American Urological Association (AUA) advises against routine PSA screening for men aged 70 or older. It also advises against it for men with a life expectancy of less than 10 to 15 years. For men aged 55 to 69, the AUA suggests discussing PSA screening.
“The decision to undergo PSA screening should be individualized, taking into account a man’s risk factors, life expectancy, and personal values.”
U.S. Preventive Services Task Force Position
The U.S. Preventive Services Task Force (USPSTF) has updated its stance. It suggests men aged 55 to 69 should discuss PSA screening with their doctor. For men outside this age range, the USPSTF advises against PSA-based screening.
Differences in International Guidelines
International guidelines differ, with some countries not recommending routine prostate cancer screening. For example, the UK’s National Health Service (NHS) does not have a national screening program. Instead, it relies on informed decision-making between men and their healthcare providers.
The variety in guidelines shows the complexity of prostate cancer screening. It highlights the need for personalized approaches. As research evolves, these guidelines will likely change, refining prostate cancer screening recommendations.
The Overdiagnosis Problem: Why Less Screening Can Sometimes Be Better
Overdiagnosis in prostate cancer screening is a big issue in medicine. It means finding cancers that won’t cause symptoms or death. This can lead to treatments that aren’t needed, causing harm.
Understanding Overdiagnosis in Prostate Cancer
Overdiagnosis happens when tests find cancers that aren’t dangerous. The use of Prostate-Specific Antigen (PSA) tests has increased cancer diagnoses. Early detection is good, but it also means more overdiagnosis.
The consequences of overdiagnosis are significant. Men may get treatments that don’t help, causing harm without any benefit.
Psychological Impact of False Positives
False positives from prostate cancer tests can really affect men. They feel anxious and worried, even if no cancer is found. This worry can lower their quality of life.
Unnecessary Treatments and Their Consequences
Overdiagnosis can lead to treatments that cause problems. These include urinary issues, erectile dysfunction, and bowel problems. These side effects can greatly affect a man’s life, showing the need to think about screening risks and benefits.
| Treatment | Potential Side Effects |
| Surgery (Prostatectomy) | Urinary incontinence, erectile dysfunction |
| Radiation Therapy | Bowel problems, erectile dysfunction |
| Hormone Therapy | Hot flashes, weight gain, fatigue |
The Concept of Watchful Waiting
Watchful waiting is a strategy for men with prostate cancer. It’s for those with low-risk disease or are older. It means watching the cancer without treating it right away, only stepping in if symptoms appear or the cancer grows.
Watchful waiting is not the same as active surveillance. Active surveillance means regular tests and biopsies to watch the cancer. Watchful waiting focuses on managing symptoms and improving quality of life.
Modern Alternatives to Traditional Prostate Exams
The way we find prostate cancer is changing. New methods are being used to make screening better and more comfortable. These changes come from advances in medical research.
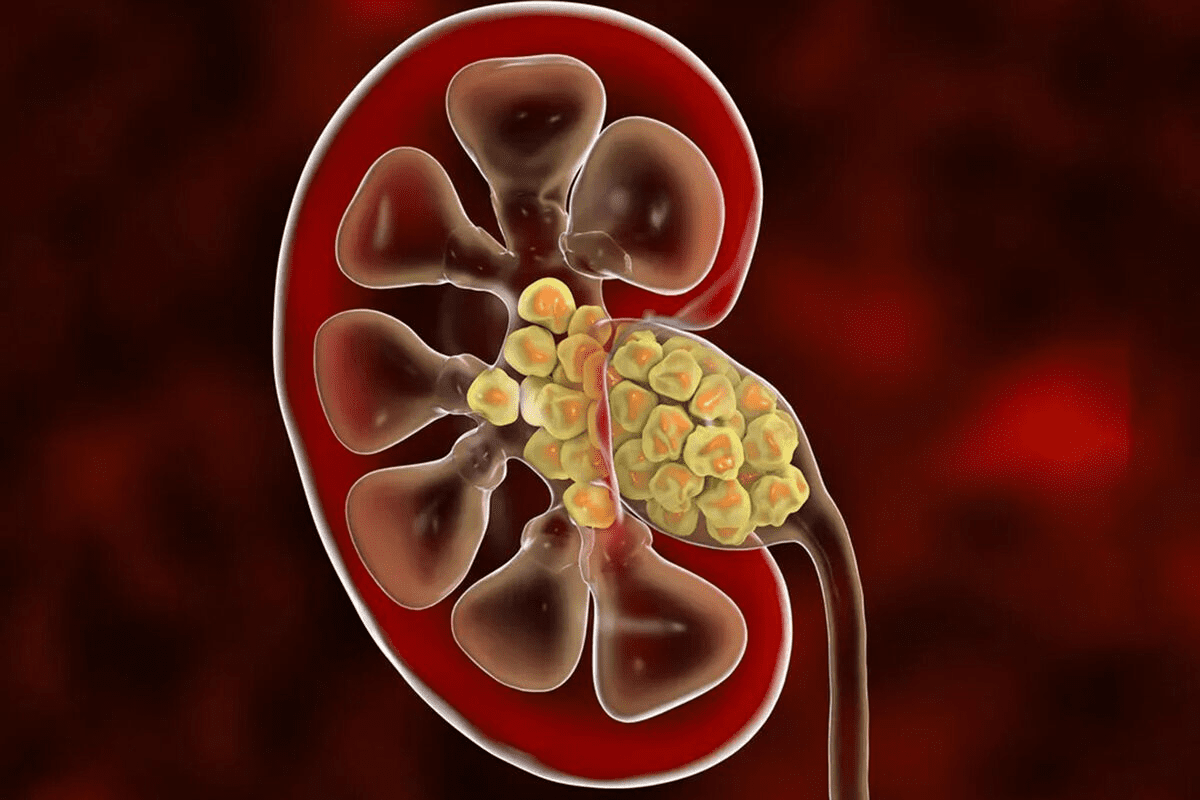
Advanced Imaging Techniques
New imaging tools like MRI and ultrasound are key in finding prostate cancer. They give clear pictures of the prostate gland. This helps doctors make more accurate diagnoses.
MRI (Magnetic Resonance Imaging) is a big help in finding prostate cancer. It shows detailed images that help spot tumors and guide biopsies. Research shows MRI can find important prostate cancer better.
- MRI-guided biopsy makes prostate cancer diagnosis more accurate.
- Multiparametric MRI uses different techniques for a full view of the prostate.
Biomarker Testing Beyond PSA
New biomarkers are being looked at to improve prostate cancer screening. These include PCA3 and TMPRSS2-ERG. They might help find prostate cancer better than just PSA testing.
PCA3 is a gene found more in prostate cancer cells. Testing for PCA3 can tell if a man with high PSA levels might have cancer.
- Biomarker tests can cut down on unnecessary biopsies.
- Using several biomarkers together might make diagnosis even better.
Genetic Testing for Prostate Cancer Risk
Genetic testing is key in figuring out prostate cancer risk. Genes like BRCA1 and BRCA2 are linked to higher risk.
Genetic counseling is advised for men with a family history of prostate cancer. It helps find who might need closer screening.
Emerging Technologies in Prostate Cancer Detection
New technologies are changing prostate cancer detection. These include AI for medical images and new biomarkers for early detection.
“The use of AI in medical imaging is changing how we find prostate cancer. AI can spot tumors that humans might miss.”
A Prostate Cancer Researcher
These new technologies will likely be big in the future of prostate cancer screening and diagnosis.
When Digital Rectal Exams Are Stil Necessary and Recommended
Digital rectal exams are key for prostate health, mainly for those at high risk or showing symptoms. Even though routine exams are less common, they’re needed in some cases. Knowing when to have one can help both patients and doctors make better choices for prostate care.
High-Risk Patient Profiles
Men with a family history of prostate cancer, African Americans, and those with BRCA1 and BRCA2 mutations are at high risk. For them, digital rectal exams are part of a detailed screening plan. Early detection is key for these groups, as it can greatly improve treatment results.
Symptomatic Cases Requiring Physical Examination
Those with symptoms like trouble urinating, painful pee, or blood in pee or semen might need a digital rectal exam. These signs suggest prostate problems that need checking. The exam helps doctors check the prostate’s size, feel, and any oddities.
Complementary Use with Other Screening Methods
Digital rectal exams are often paired with PSA tests and MRI scans. This mix gives a deeper look at prostate health. “Using different screening methods together can improve detection and tailor treatments to each patient.”
Follow-up Examinations After Abnormal Results
Patients with odd PSA test results or other screening issues might need follow-up exams. These exams track prostate changes and decide if more tests or treatment are needed. Regular check-ups are vital for good prostate care.
“The role of digital rectal exams in prostate cancer screening is evolving, but they remain an essential tool in certain clinical contexts.”
” A Urologist
The Effectiveness Debate: Comparing Traditional Exams to Modern Methods
Healthcare experts are debating the effectiveness of traditional prostate exams versus modern screening methods. New technologies are emerging, and it’s important to compare them to traditional methods. We need to look at their accuracy, cost, and how they affect patient outcomes.
Sensitivity and Specificity Comparisons
When we compare traditional digital rectal exams (DRE) to modern tests like PSA testing and MRI scans, sensitivity and specificity are key. Traditional DRE is less sensitive than PSA testing for catching early-stage prostate cancer. But, DRE can provide useful information when combined with other tests.
A study in the Journal of Urology found that using DRE and PSA testing together can increase detection rates by 26% compared to PSA testing alone. MRI scans also show high sensitivity in detecting significant prostate cancer.
“The use of MRI in prostate cancer diagnosis has revolutionized our ability to detect and stage the disease accurately.” – An Urologist
Cost-Effectiveness Analysis
The cost-effectiveness of different screening methods is a big part of the debate. Modern imaging techniques like MRI are very accurate but also very expensive. A study in the Journal of Clinical Oncology found that PSA screening is more cost-effective than DRE for detecting prostate cancer.
| Screening Method | Cost | Sensitivity | Specificity |
| DRE | Low | Moderate | High |
| PSA Testing | Moderate | High | Moderate |
| MRI | High | Very High | High |
Patient Outcomes Research
The true measure of a screening method’s effectiveness is its impact on patient outcomes. Research shows that early detection through screening can improve survival rates for prostate cancer patients. A study in the New England Journal of Medicine found that regular screening can lower the risk of prostate cancer mortality.
Quality of Life Considerations
Quality of life is also a key factor in the effectiveness debate. Screening methods that lead to overdiagnosis and overtreatment can harm a patient’s quality of life. Modern methods aim to find a balance between early detection and avoiding unnecessary treatments.
Age-Specific Prostate Exam Guidelines and Recommendations
Age is key in setting prostate exam guidelines. Different ages have different screening needs. The risk of prostate cancer changes as men get older.
Guidelines for Men in Their 40s
Men in their 40s face a personalized screening approach. Those with a family history of prostate cancer or other risk factors might start screening early. The American Cancer Society advises starting the talk about screening at 50 for average-risk men. But, those at higher risk should discuss it sooner.
Recommendations for Men in Their 50s and 60s
Men in their 50s and 60s with average risk should get screened regularly. The exact frequency depends on initial results and health. Those at higher risk might need more frequent or earlier tests.
Screening Frequency Based on Age and Risk
| Age Group | Average Risk Screening Frequency | Higher Risk Screening Frequency |
| 40-49 | No routine screening | Discuss with provider; potentially every 2-3 years |
| 50-69 | Every 2-4 years | Every 1-2 years |
| 70+ | Discuss cessation with provider | Individualized based on health status |
Screening Considerations for Men Over 70
Men over 70 should consider their health and life expectancy for screening. Those with a short life expectancy might not benefit from screening.
Risk Factors That Modify Age Recommendations
Some risk factors can change when to start screening. These include family history, ethnicity, and genetics. Men with these factors might need to start screening earlier.
It’s vital for men to talk to their healthcare provider about their risk factors and screening options. This helps determine the best screening schedule for them.
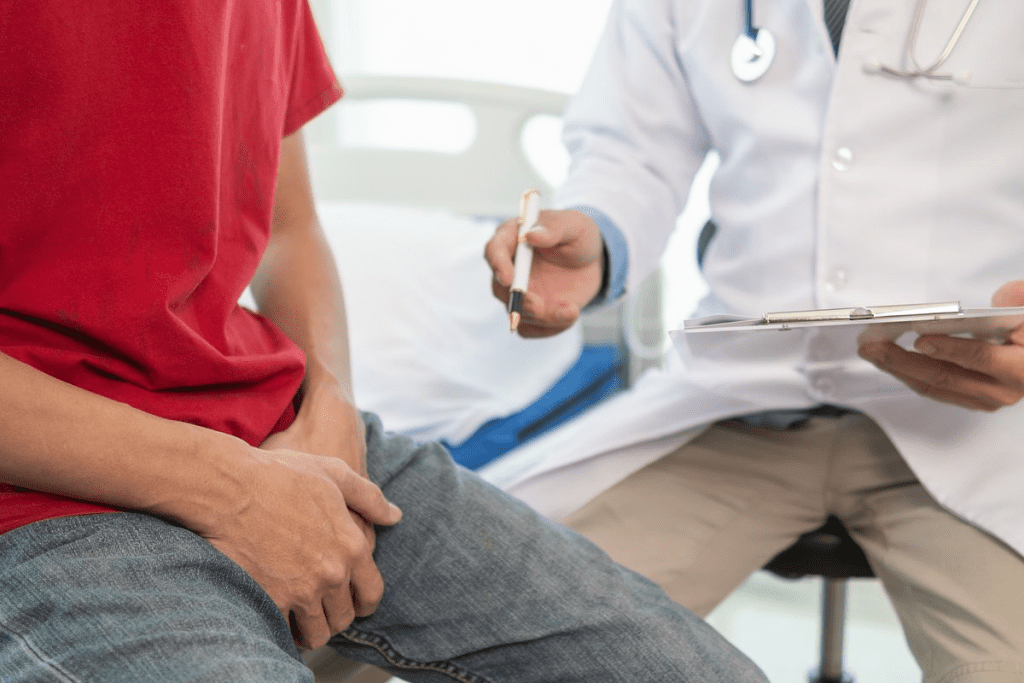
The Role of Primary Care Physicians vs. Specialists in Prostate Health
It’s key to know the roles of primary care doctors and specialists for good prostate health. Prostate care is a team effort. Each healthcare provider has a special role in finding, treating, and managing the condition.
When to See a Urologist
Primary care doctors are usually the first stop for prostate concerns. But, if you have issues like high PSA levels or trouble urinating, you should see a urologist. Urologists are experts in urinary and reproductive system issues, making them essential for prostate care.
Coordinating Care Between Providers
It’s important for primary care doctors and specialists to work together. They share patient info, test results, and treatment plans. This teamwork ensures a complete care plan for prostate health.
Communication Strategies for Patients
Patients must talk openly with their doctors. This means asking questions, sharing symptoms, and understanding treatment choices. Being informed and involved in your care helps you follow recommended steps.
Shared Decision-Making in Prostate Screening
Shared decision-making is when patients and doctors talk about screening and treatment options.
“Shared decision-making respects the patient’s autonomy and preferences, leading to more personalized and appropriate care.”
This is very important in prostate health. Decisions about screening and treatment can greatly affect a patient’s life quality.
Common Myths and Misconceptions About Prostate Exams
Many men have wrong ideas about prostate exams. These ideas come from bad information or not understanding. This section will clear up common myths and misconceptions about prostate exams.
Debunking Prostate Exam Myths
One big myth is that only older men need prostate exams. But, guidelines say men with a family history or other risk factors might need to start earlier. The need and how often for prostate exams really depend on your risk factors, like age, family history, and ethnicity.
Another myth is that prostate exams hurt. While some might feel a bit uncomfortable, it’s not usually painful. Knowing what to expect can help reduce worry.
Understanding the True Purpose of Different Screening Methods
There are different screening methods for a reason. For example, the PSA test checks the prostate-specific antigen in your blood. A digital rectal exam (DRE) lets doctors feel the prostate gland. Both tests give important info that, together, help find prostate problems early.
No test is perfect. But, using PSA testing and DRE together can help find problems sooner. It’s key to talk about the good and bad with your doctor.
Cultural and Social Barriers to Prostate Health Discussions
Cultural and social issues can stop men from talking about prostate health. Shyness and fear of bad news can keep them from getting medical help. Making a safe and supportive place can help men talk about their health and get the tests they need.
Addressing Fear and Embarrassment
Doctors are key in helping men feel at ease. They offer supportive care and clear explanations about the tests and why they’re good. Men should feel free to ask questions and share their worries. This helps make talking about prostate health normal.
By tackling these myths and misconceptions, men can make better health choices. This leads to better prostate health for everyone.
Conclusion: The Future of Prostate Cancer Screening
The world of prostate cancer screening is changing fast. New medical tech and a better understanding of the disease are leading the way. We’ve seen how often traditional prostate exams are now done less, thanks to better tools.
New tools like advanced imaging and biomarker tests are making a big difference. They’re more accurate and less invasive. This means we can find and treat prostate cancer better.
The future of screening will mix new tools with smart, targeted approaches. This aims to catch cancer early without causing too much harm. It’s all about finding the right balance.
As we learn more, doctors and patients will work together more closely. This means making care plans that fit each person’s needs. Keeping up with the latest in prostate cancer screening is key for everyone involved.
FAQ
Why are prostate exams less common now?
Prostate exams are less common today because of new guidelines and screening methods. The medical field now looks at each person’s risk differently. This change aims to avoid overdiagnosis and overtreatment.
Do doctors stil do prostate exams?
Yes, doctors do perform prostate exams, like digital rectal exams (DRE), in some cases. They use them for high-risk patients, those with symptoms, and as a tool with other tests. But, DREs are not as routine as they once were.
What is the difference between a digital rectal exam and a PSA test?
A digital rectal exam is a physical check where a doctor feels the prostate. A PSA test, on the other hand, is a blood test for prostate-specific antigen. Today, PSA tests are the main way to screen for prostate cancer, with DRE used in specific cases.
Why did doctors stop doing routine prostate checks?
Doctors stopped routine checks because of the limits and debates around DREs. There’s also the problem of overdiagnosis and overtreatment. Now, they recommend a more personalized approach to screening.
What are the current prostate cancer screening methods?
Today, screening includes PSA tests, digital rectal exams, and advanced imaging like MRI and ultrasound. New tests, like biomarkers and genetic testing, are also being explored.
Are PSA tests replacing prostate exams?
PSA tests are now the main screening tool for prostate cancer. But, they don’t replace prostate exams entirely. Both have their own strengths and weaknesses, and are sometimes used together.
How accurate are prostate exams?
The accuracy of prostate exams, like DREs, is debated. While DRE can find some issues, it’s not as accurate as PSA tests or advanced imaging.
When is a prostate exam stil necessary?
Prostate exams are needed in certain situations. This includes high-risk patients, those with symptoms, and follow-ups after abnormal results. They’re also used with other screening methods.
What are the alternatives to digital rectal exams?
Alternatives to DREs include PSA tests, advanced imaging, biomarker testing, and genetic testing. These new technologies are changing how we screen for prostate cancer.
What are the age-specific guidelines for prostate exams?
Guidelines for prostate exams vary by age. Men are usually advised to talk about screening in their 40s or 50s. Recommendations can change based on individual risk and health, even for men over 70.
Who should see a urologist for prostate health?
Men with high-risk profiles, abnormal results, or symptoms should see a urologist. Primary care doctors also play a key role in guiding care and discussing prostate health.
What are some common myths about prostate exams?
Myths about prostate exams include thinking they’re always painful or the only way to find cancer. Education helps clear these myths and encourages men to talk about their prostate health.
References
- American Cancer Society. (2024). Prostate Cancer Screening Guidelines. https://www.cancer.org/health-care-professionals/american-cancer-society-prevention-early-detection-guidelines/prostate-cancer-screening-guidelines.html