Last Updated on November 26, 2025 by Bilal Hasdemir

Prostate cancer is one of the most common cancers in men, with more than 200,000 new cases diagnosed annually in the U.S. When a man gets this diagnosis, he must decide between removing the prostate or using radiation therapy. This choice depends on the cancer’s stage, how aggressive it is, and the man’s overall health.
We will look at the pros and cons of prostatectomy vs radiation, two main ways to treat prostate cancer. Knowing about these prostate cancer treatment options is key to making a good choice.
Key Takeaways
- Prostate cancer treatment options include surgical removal of the prostate and radiation therapy.
- The choice between prostatectomy and radiation depends on the cancer’s stage and aggressiveness.
- Each treatment option has its benefits and risks.
- Understanding these options is key to making an informed decision.
- Patient health and preferences play a big role in choosing a treatment.
Understanding Prostate Cancer and Treatment Options
Prostate cancer is a complex condition that needs a deep understanding. It’s important to know its types, stages, and treatment options. Recognizing the factors that influence treatment choices is key.
Types and Stages of Prostate Cancer
Prostate cancer can be classified into different types. The most common type is adenocarcinoma, which starts in the glandular cells of the prostate. Knowing the stage of prostate cancer is also vital. It helps determine how far the disease has spread.
The stages range from localized prostate cancer to advanced prostate cancer. The TNM system is used to stage prostate cancer. It looks at the tumor size (T), lymph node involvement (N), and metastasis (M). This helps doctors choose the best treatment.
Overview of Available Treatment Approaches
There are many ways to treat prostate cancer, from active surveillance to surgery and radiation therapy. The right treatment depends on the cancer’s stage and aggressiveness. It also depends on the patient’s health and what they prefer.
- Surgery: Radical prostatectomy removes the prostate gland. It can be done through open, laparoscopic, or robotic-assisted surgery.
- Radiation Therapy: This uses high-energy rays to kill cancer cells. It can be external or internal.
- Active Surveillance: For low-risk prostate cancer, active surveillance is used. It involves regular PSA tests, biopsies, and digital rectal exams. Treatment is delayed until the cancer shows signs of growing.
Knowing about these treatment options is important for making informed decisions. By considering the cancer type, stage, and patient’s situation, doctors can suggest the best treatment plan.
Prostatectomy vs Radiation: The Two Main Treatment Approaches
Radical prostatectomy and radiation therapy are the top treatments for prostate cancer. It’s important for patients to know about these options to make the best choice for their care.
What is Radical Prostatectomy?
Radical prostatectomy is a surgery to remove the prostate gland. It’s a main treatment for prostate cancer, mainly for those with early-stage disease. The surgery can be done in different ways, like open, laparoscopic, or robotic-assisted methods.
Key aspects of radical prostatectomy include:
- Removal of the prostate gland and seminal vesicles
- Preservation of surrounding nerves when possible
- Varying recovery times based on surgical technique
What is Radiation Therapy for Prostate Cancer?
Radiation therapy is another effective treatment for prostate cancer. It uses high-energy rays to kill cancer cells. There are two main types: external beam radiation therapy (EBRT) and brachytherapy.
| Type of Radiation Therapy | Description |
| External Beam Radiation Therapy (EBRT) | Delivers radiation from outside the body, targeting the prostate gland |
| Brachytherapy | Involves placing radioactive seeds directly into the prostate |
Both radical prostatectomy and radiation therapy have their benefits and possible side effects. The choice between them depends on several factors. These include the cancer’s stage and aggressiveness, the patient’s health, and personal preferences.
Radical Prostatectomy: Procedure and Techniques

Radical prostatectomy is a major surgery for prostate cancer. It uses different surgical techniques. The choice depends on the patient’s health, cancer stage, and the surgeon’s skills.
Open Radical Prostatectomy
Open radical prostatectomy is a traditional method. It removes the prostate through a single incision in the abdomen or perineum. This method gives direct access to the prostate gland.
Benefits: The surgeon has more control, and it’s widely available. Risks: A larger incision can lead to longer recovery times and more visible scarring.
Laparoscopic Prostatectomy
Laparoscopic prostatectomy makes several small incisions. Surgical instruments and a camera are inserted to remove the prostate. This method causes less tissue damage.
Advantages: It results in less blood loss, smaller scars, and quicker recovery. Challenges: It requires advanced laparoscopic skills and may have a longer learning curve.
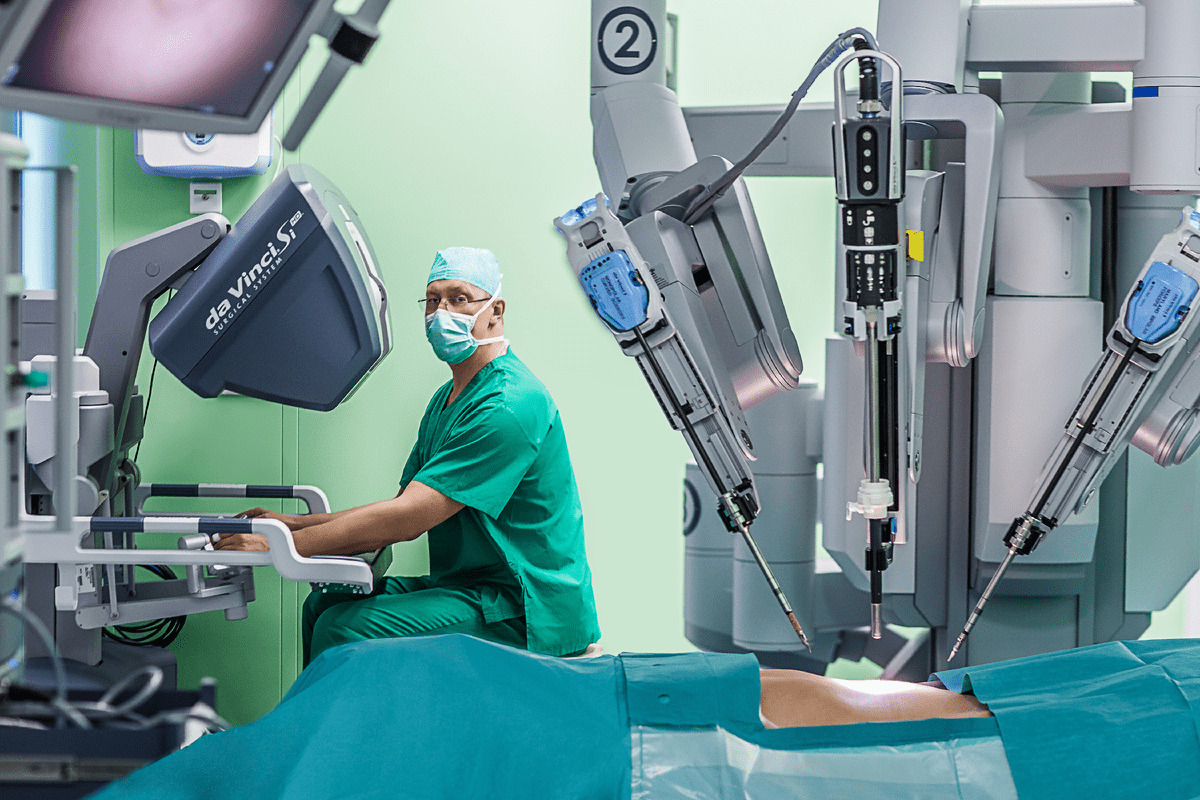
Robotic-Assisted Prostatectomy
Robotic-assisted prostatectomy is an advanced laparoscopic surgery. It uses a robotic system to enhance the surgeon’s capabilities. It offers high-definition 3D vision and precise instrumentation.
Benefits: It provides enhanced precision, flexibility, and control. It may result in less blood loss and faster recovery. Limitations: It has a high initial investment for the robotic system and requires specialized training.
Each technique has its own advantages and drawbacks. The choice depends on the patient’s situation and the surgeon’s expertise.
Radiation Therapy Options for Prostate Cancer
Radiation therapy is a key treatment for prostate cancer. It uses different methods to target cancer cells while saving healthy tissue. This approach helps in fighting cancer effectively.
External Beam Radiation Therapy (EBRT)
External Beam Radiation Therapy (EBRT) is a non-invasive method. It uses beams from a machine outside the body to kill cancer cells. EBRT is highly effective and can be adjusted to fit the tumor’s shape and size.
There are several types of EBRT, including:
- 3D Conformal Radiation Therapy, which precisely targets the prostate.
- Intensity-Modulated Radiation Therapy (IMRT), allowing for varying intensities of radiation.
- Stereotactic Body Radiation Therapy (SBRT), delivering high doses in fewer sessions.
Brachytherapy (Seed Implants)
Brachytherapy involves placing small radioactive seeds in or near the prostate gland. This method delivers high doses of radiation directly to the tumor. It helps in saving healthy tissues.
Brachytherapy can be used alone or in combination with EBRT, depending on the cancer’s stage and aggressiveness. It requires careful planning for optimal seed placement.
Combination Approaches
For some patients, a mix of EBRT and brachytherapy is recommended. This is often the case for those with intermediate or high-risk prostate cancer.
Combining these techniques can improve cancer control rates. It also helps in managing side effects.
Radiation therapy, whether through EBRT, brachytherapy, or a combination, is a versatile and effective treatment for prostate cancer. The choice depends on the cancer’s stage and grade, the patient’s health, and personal preferences.
Effectiveness and Success Rates
When looking at treatments for prostate cancer, knowing how well prostatectomy and radiation therapy work is key. Both treatments have been studied a lot. Their success rates give important insights for patients and doctors.
Cancer Control Rates for Prostatectomy
Radical prostatectomy is very good at controlling cancer, mainly for those with cancer that’s only in the prostate. Studies show that 80% to 90% of patients stay cancer-free for 5 years. This depends on the cancer’s stage and how aggressive it is.
A study found that after 10 years, about 75% of patients with high-risk cancer stayed cancer-free after surgery. This shows surgery is effective in fighting prostate cancer.
Cancer Control Rates for Radiation Therapy
Radiation therapy, like external beam radiation therapy (EBRT) and brachytherapy, also has good cancer control rates. How well it works depends on the dose, cancer stage, and patient health.
A study showed that 5-year cancer-free survival rates for EBRT were similar to surgery, at 80% to 90%. Brachytherapy, alone or with EBRT, works well for low- to intermediate-risk cancer patients.
| Treatment | 5-Year Biochemical Recurrence-Free Survival | 10-Year Biochemical Recurrence-Free Survival |
| Radical Prostatectomy | 80-90% | 75% |
| External Beam Radiation Therapy (EBRT) | 80-90% | 70-80% |
| Brachytherapy | 85-95% | 75-85% |
The table shows both prostatectomy and radiation therapy have high cancer control rates. Rates vary based on the treatment and patient specifics.
“Choosing between prostatectomy and radiation therapy depends on many factors. These include the cancer’s stage and aggressiveness, and the patient’s health and preferences.”
Expert Opinion
We suggest patients talk to their doctors about these factors. This helps decide the best treatment plan.
Side Effects and Complications of Prostatectomy
Prostatectomy is a treatment for prostate cancer but comes with side effects. It’s important for patients to know about these to make the best choice for their care.
Short-term Complications
Right after a prostatectomy, patients might face infections, bleeding, or reactions to anesthesia. These issues are usually handled with good medical care. We keep a close eye on patients to catch any signs of these problems early.
Common short-term complications:
- Infection
- Bleeding or hematoma
- Anesthesia-related complications
- Clot formation
Urinary Incontinence
Urinary incontinence can be a long-term issue after prostatectomy. How likely and severe it is can depend on the surgery method and the patient’s health.
Factors influencing urinary incontinence:
| Factor | Description | Impact on Incontinence |
| Surgical Technique | Method used for prostatectomy (open, laparoscopic, robotic) | Robotic techniques may reduce risk |
| Patient Age | Age of the patient at the time of surgery | Younger patients may recover faster |
| Pre-existing Conditions | Presence of conditions like diabetes or heart disease | May increase the risk of complications |
Erectile Dysfunction
Erectile dysfunction (ED) is a common side effect of prostatectomy. The risk depends on the patient’s age, nerve damage during surgery, and their sexual health before surgery.
Strategies to mitigate erectile dysfunction:
- Nerve-sparing surgical techniques
- Preoperative counseling
- Postoperative rehabilitation programs
Dealing with prostatectomy side effects can be tough. Our healthcare team is here to offer full support. We aim to help manage these issues and improve our patients’ lives.
Side Effects and Complications of Radiation Therapy
It’s important for prostate cancer patients to know about radiation therapy’s side effects. This treatment can help fight cancer but also has downsides that affect daily life.
Acute Side Effects
Acute side effects happen right away or soon after treatment starts. These can include feeling very tired, needing to pee a lot, and irritation in the bladder and rectum. We keep a close eye on patients to help manage these issues.
Common acute side effects are:
- Fatigue
- Urinary frequency or urgency
- Diarrhea or rectal discomfort
Urinary and Bowel Problems
Radiation therapy can cause long-term issues with urination and bowel movements. These problems might include not being able to control urine, needing to pee a lot, and irritation or bleeding in the bowel. We’ll talk about ways to lessen these effects and improve your life quality.
Management strategies for these problems include:
- Pelvic floor exercises
- Dietary adjustments
- Medications to manage symptoms
Sexual Function Impact
Radiation therapy can also affect sexual function, possibly causing erectile dysfunction. We take this serious issue seriously and will discuss treatment options and support.
Treatments for erectile dysfunction might include:
- Medications
- Penile implants
- Counseling and support
Knowing about radiation therapy’s side effects helps prostate cancer patients make better choices. We’re here to offer full care and support during treatment.
Recovery and Quality of Life Considerations
Choosing between prostatectomy and radiation therapy involves thinking about recovery and quality of life. It’s important to understand how each treatment affects daily life.
Recovery Timeline After Prostatectomy
The time it takes to recover from a prostatectomy varies. It depends on the surgery method and the patient’s health. Most patients can get back to normal in a few weeks.
Here’s what you might experience during recovery:
- Immediate post-surgery (1-2 weeks): Rest and recovery at home, with possible discomfort and fatigue.
- Short-term recovery (2-6 weeks): Gradual return to light activities, with possible urinary incontinence and erectile dysfunction.
- Long-term recovery (3-6 months): Continued improvement in urinary and sexual function, with most patients returning to their normal activities.
| Recovery Stage | Timeline | Expected Outcomes |
| Immediate Post-Surgery | 1-2 weeks | Rest, possible discomfort, and fatigue |
| Short-Term Recovery | 2-6 weeks | Return to light activities, possible urinary incontinence and erectile dysfunction |
| Long-Term Recovery | 3-6 months | Improvement in urinary and sexual function, return to normal activities |
Recovery Experience With Radiation Therapy
Radiation therapy recovery is different from surgery because it’s non-invasive. Patients usually face fewer immediate side effects.
But, radiation therapy can cause side effects that affect quality of life. These include:
- Fatigue
- Urinary issues, such as frequency or urgency
- Bowel problems, such as diarrhea or rectal discomfort
- Sexual dysfunction
It’s key for patients to talk to their healthcare provider about their recovery and side effects. This helps make an informed treatment choice.
Long-term Outcomes and Survival Rates
When it comes to treating prostate cancer, treatments like prostatectomy and radiation therapy are often compared. It’s important for patients and doctors to know about long-term survival rates. This knowledge helps in making the right treatment choices.
5-Year, 10-Year, and 15-Year Survival Comparisons
Research has looked into how well prostatectomy and radiation therapy work over time. A detailed analysis of many studies gives us a clear picture of survival rates at different times.
| Treatment | 5-Year Survival Rate | 10-Year Survival Rate | 15-Year Survival Rate |
| Prostatectomy | 95-100% | 85-95% | 75-85% |
| Radiation Therapy | 90-100% | 80-90% | 70-80% |
These numbers show that both treatments are very effective. But, the success rate can change based on the cancer’s stage and how aggressive it is.
Risk of Cancer Recurrence
The chance of cancer coming back is a key factor in judging treatment success. Studies show that prostatectomy and radiation therapy have different rates of recurrence. This depends on the cancer’s initial stage and the patient’s health.
Recurrence Rates: Some studies suggest prostatectomy might lower recurrence rates, mainly for early-stage cancer. But, radiation therapy, often used with hormone therapy, can also keep recurrence rates low.
Knowing these long-term results helps patients choose the best treatment. It’s about weighing the benefits and risks of each option.
Factors That Influence Treatment Decision
Choosing between surgery and radiation for prostate cancer depends on many things. Several important factors are considered when picking the best treatment.
Age and Overall Health
A patient’s age and health are key in deciding between surgery and radiation. Older patients or those with serious health problems might prefer radiation. It’s less invasive and could have fewer side effects than surgery. Younger patients with fewer health issues might choose surgery. It can offer a more complete treatment for prostate cancer.
Cancer Stage and Aggressiveness
The cancer’s stage and how aggressive it is also matter a lot. For localized, low-risk prostate cancer, treatments like active surveillance might be suggested. But, for high-risk or advanced prostate cancer, treatments like surgery or a mix of radiation and hormone therapy are often better.
Personal Preferences and Lifestyle
What a patient prefers and their lifestyle also affect the choice. Some might choose based on avoiding certain side effects. For example, someone worried about losing sexual function might pick radiation or a nerve-sparing surgery. How a patient’s lifestyle and support system are also important in making this decision.
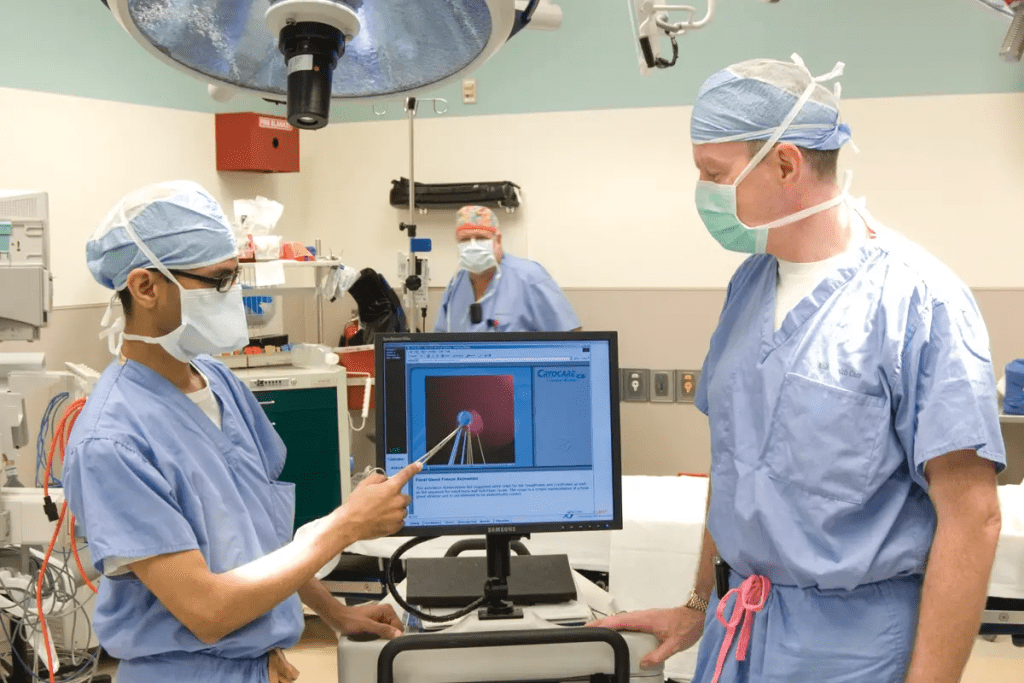
Doctor Recommendations
Doctors’ advice is also very important. Urologists and radiation oncologists give advice based on the latest research and their experience. It’s important for patients to talk with their doctors about their options. This way, they can understand why certain treatments are recommended and how they fit with the patient’s health and wishes.
In summary, choosing a treatment for prostate cancer involves looking at many factors. By understanding these, patients can make choices that are right for them.
- Age and overall health of the patient
- Stage and aggressiveness of the prostate cancer
- Personal preferences and lifestyle considerations
- Recommendations from healthcare professionals
Newer Treatment Approaches and Advances
New technologies and methods are giving hope to those with prostate cancer. Medical research is moving fast, leading to new treatments. These aim to better outcomes and lessen side effects.
Focal Therapy Options
Focal therapy is a big change in prostate cancer treatment. It targets the tumor directly, leaving healthy tissue alone. This could mean fewer side effects than older treatments.
Some focal therapy options include:
- High-Intensity Focused Ultrasound (HIFU): A non-invasive method using ultrasound to kill cancer cells.
- Cryotherapy: Freezing cancer cells to death.
- Nanoknife Irreversible Electroporation: A minimally invasive method that kills cells with electrical pulses.
These therapies are for early-stage prostate cancer. They’re often tested in clinical trials or as part of a treatment plan.
Emerging Technologies and Techniques
Other new technologies and methods are being looked into for prostate cancer treatment. These include:
- Advanced Imaging Techniques: Like MRI and PET scans, for better diagnosis and staging.
- Robotic Surgery: Improved robotic surgery for more precise and quicker recovery.
- Immunotherapy: Using the immune system to fight cancer, with vaccines and checkpoint inhibitors.
- Precision Medicine: Tailoring treatment to the individual based on genetic profiles and other factors.
These new technologies and methods could lead to better treatment results and quality of life for prostate cancer patients.
As research keeps moving forward, it’s key for patients to talk to their doctors. This way, they can find the best treatment plan for their situation.
How to Make Your Decision: A Framework
Choosing a treatment for prostate cancer can be tough. But with the right approach, patients can feel more in control. We aim to guide you through this tough time, helping you make a well-informed choice.
When looking at prostate removal or radiation therapy, knowing all about your options is key. You need to understand the possible side effects and what results you might see. This knowledge empowers you to decide what’s best for your health.
Questions to Ask Your Doctor
It’s vital to ask the right questions when talking to your doctor about treatment. Here are some important ones to think about:
- What are the benefits and risks of each treatment?
- How might the treatment affect my daily life?
- What are the chances of cancer coming back with each option?
- Are there newer or alternative treatments I should look into?
By asking these questions, you’ll get a better grasp of your options. This helps you make a choice that’s right for you.
Seeking Second Opinions
Getting a second opinion can offer new insights and boost your confidence in your choice. Remember, getting a second opinion is a common and valuable step in making a decision.
When you’re looking for a second opinion, here’s what to do:
- Find a specialist with a lot of experience in prostate cancer.
- Share all your medical records and test results.
- Ask questions and talk about any worries you have with the second doctor.
By using this framework, you can make a better choice about your prostate cancer treatment, whether it’s prostate removal or radiation therapy. We’re here to support you every step of the way.
Conclusion
Choosing between prostatectomy and radiation therapy for prostate cancer is a big decision. It depends on the cancer’s stage and how aggressive it is. Also, the patient’s health plays a big role.
Looking at both treatments shows their good and bad sides. Knowing the differences helps patients make a better choice.
The right treatment for prostate cancer is one that fits the patient’s needs. Factors like age, health, cancer stage, and personal wishes are important. This helps patients make informed choices about their care.
Success in treatment comes from looking at all options and talking to a healthcare provider. Patients and their teams can find the best plan together.
FAQ
What are the main treatment options for prostate cancer?
The main treatments for prostate cancer are surgery and radiation. Surgery removes the prostate. Radiation uses rays to kill cancer cells.
What is the difference between open, laparoscopic, and robotic-assisted prostatectomy?
Open surgery uses one big cut. Laparoscopic surgery has small cuts and a camera. Robotic-assisted surgery uses a robot for better control.
What are the possible side effects of radical prostatectomy?
Side effects include trouble peeing and erectile issues. You might also face bleeding and infection right after surgery.
What are the different types of radiation therapy used to treat prostate cancer?
There’s external beam radiation and brachytherapy (seed implants). Some use both for better results.
What are the possible side effects of radiation therapy for prostate cancer?
Side effects include urinary and bowel issues. It can also affect your sex life.
How do I decide between prostatectomy and radiation therapy for prostate cancer?
Your choice depends on the cancer’s stage and your health. Age and personal preferences also play a role.
What are the long-term survival rates for prostatectomy and radiation therapy?
Both treatments have high survival rates. The 5, 10, and 15-year survival rates are similar.
What is the risk of cancer recurrence after prostatectomy and radiation therapy?
The risk of cancer coming back varies. It depends on the cancer’s stage and how well the treatment worked.
Are there newer treatment approaches available for prostate cancer?
Yes, there are newer options like focal therapy. Targeted radionuclide therapy is also emerging.
How can I make an informed decision about my prostate cancer treatment?
Ask your doctor questions and seek second opinions. Think about your situation and what you prefer.
What are the benefits of seeking a second opinion for prostate cancer treatment?
A second opinion can give you more information. It helps you make a better choice for your treatment.
How do I choose the best treatment for my prostate cancer?
Consider your cancer’s stage, your health, and what you prefer. Talk to your healthcare provider about these factors.
Reference
- American Urological Association. (2022). Clinically Localized Prostate Cancer: AUA/ASTRO Guideline.