Benign Prostatic Hyperplasia (BPH) is a common condition in men. It affects the prostate gland, causing it to grow. This growth can lead to problems with urination. What is the prostatic hypertrophy pathophysiology? This guide explains the complex biological changes that lead to BPH (enlarged prostate).
The exact cause of BPH is not fully understood. But, it is believed to be related to hormonal changes and aging. These changes can cause the prostate to grow, leading to BPH.
Understanding the pathophysiology of BPH is important. It helps doctors diagnose and treat the condition. By knowing how BPH works, doctors can find the best treatment options for each patient.
Key Takeaways:
- Benign Prostatic Hyperplasia (BPH) is a common condition in men.
- The exact cause of BPH is not fully understood, but hormonal changes and aging are believed to play a role.
- Understanding the pathophysiology of BPH is important for diagnosis and treatment.
- Doctors can find the best treatment options for each patient by knowing how BPH works.
Overview of Benign Prostatic Hyperplasia
Benign Prostatic Hyperplasia (BPH) is when the prostate gland gets bigger. This can cause problems like needing to pee a lot, feeling urgent, and having a weak stream. It’s a common issue that men face as they get older.
By the time men reach 60, about half will have BPH. Knowing what causes it, its symptoms, and how to treat it is key to managing it well.
Anatomical and Histological Changes in BPH
Benign Prostatic Hyperplasia (BPH) makes the prostate gland grow bigger. This growth blocks urine flow. Knowing how BPH changes the prostate is key for treating it.
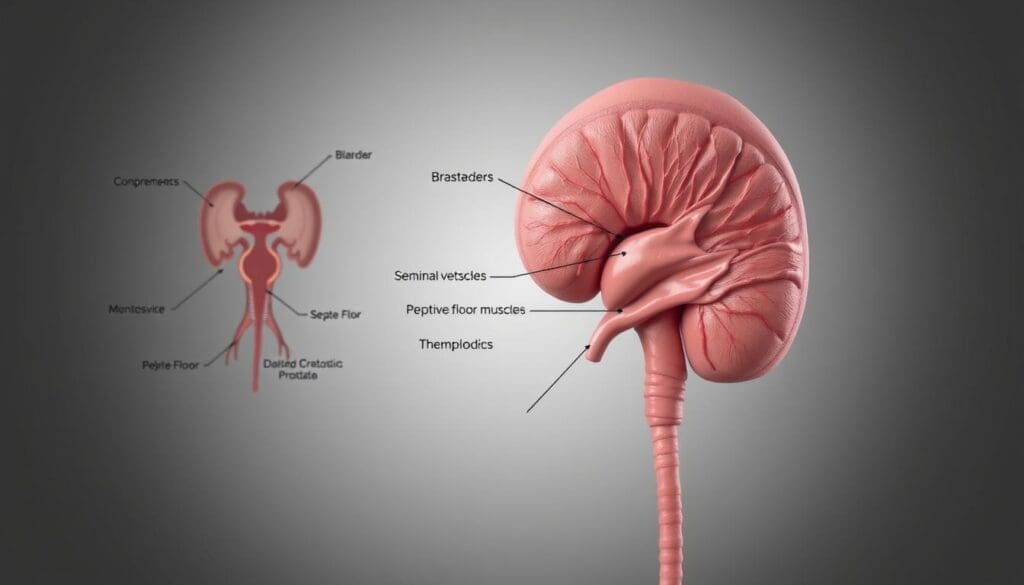
Normal Prostate Anatomy
The prostate gland is small, like a walnut. It sits between the bladder and the penis. It wraps around the urethra, which carries urine out of the body.
Histological Changes
In BPH, the prostate gets bigger because more cells grow. This makes the urethra narrow and blocks urine flow. The changes include nodules and more glandular and stromal cells.
The growth of the prostate in BPH puts pressure on the urethra. This leads to symptoms like trouble urinating.
Prostatic Hypertrophy Pathophysiology: Core Mechanisms
Benign Prostatic Hyperplasia (BPH) is a condition where the prostate gland gets bigger. This leads to symptoms like trouble urinating. There are two main parts to BPH’s cause: the gland itself getting bigger and the muscles in the prostate tightening.
Hormonal Influences on BPH Development

Hormonal Influences on Benign Prostatic Hyperplasia
BPH is when the prostate gland gets bigger. Hormones, like testosterone and dihydrotestosterone (DHT), are key players. They help the prostate grow.
Testosterone turns into DHT with the help of an enzyme called 5-alpha-reductase. DHT is stronger and makes the prostate bigger. Knowing how androgens affect BPH helps doctors find better treatments.
There are medicines that stop DHT from being made. These medicines help shrink the prostate and ease symptoms. This makes life better for people with BPH.
Genetic Factors and Hereditary Predisposition
Studies have found that genetics are a big part of Benign Prostatic Hyperplasia (BPH). Family history and genetic predisposition help us understand BPH better.
Genetic changes, like those in androgen metabolism, increase BPH risk. The androgen receptor gene is key, with certain variations affecting BPH severity and progression.
Grasping BPH’s genetic side is vital for better prevention and treatment. More research is needed to uncover how genes and environment interact in BPH.
Cellular and Molecular Basis of BPH
Benign Prostatic Hyperplasia (BPH) is a complex condition. It involves the enlargement of the prostate gland. This enlargement is due to the interaction between epithelial and stromal cells. The androgen receptor plays a key role in this process.
The development of BPH involves changes in gene expression. It also involves alterations in cellular signaling pathways. Understanding these mechanisms is essential for diagnosing and treating BPH.
Inflammatory Processes in BPH Progression

Inflammatory Processes in BPH
The growth of Benign Prostatic Hyperplasia (BPH) is tied to inflammation. Chronic inflammation makes the prostate gland grow bigger.
Role of Cytokines
Cytokines like IL-6 and TNF-alpha are key in BPH’s inflammation. They bring immune cells to the prostate, causing inflammation and damage.
Impact on BPH Progression
Chronic inflammation in BPH makes the disease worse. Knowing how this happens helps in finding better treatments.
Management Strategies
Targeting inflammation could lead to new BPH treatments. Lowering inflammation might slow or stop the disease’s growth. This could improve symptoms and life quality for patients.
Oxidative Stress and Antioxidant Mechanisms
Oxidative stress is a major player in Benign Prostatic Hyperplasia (BPH). It happens when the body can’t keep up with the damage caused by reactive oxygen species (ROS). This imbalance can lead to BPH getting worse.
Peroxiredoxin 3 (Prdx3) is an antioxidant enzyme that fights off this damage. It helps protect cells from harm. Knowing how oxidative stress affects BPH is key to finding better treatments.
Dysregulated Autophagy and Metabolic Alterations
Autophagy is key for keeping cells healthy. It helps remove damaged parts. But, in Benign Prostatic Hyperplasia (BPH), autophagy goes wrong. This leads to a buildup of damaged cells, causing BPH to grow.
Changes in how cells use glucose and lipids also play a big part in BPH. It’s important to understand how autophagy, metabolic changes, and BPH are connected. This knowledge can help us find better treatments.
The link between autophagy and BPH is complex. It affects how cells grow and multiply. More research is needed to fully understand this connection. This will help us find new ways to treat BPH.
Understanding BPH and Its Impact on Men’s Health
Benign prostatic hyperplasia (BPH) is a common condition in men, affecting nearly 50% of those over 50. It’s a non-cancerous enlargement of the prostate gland, which can lead to urinary issues and discomfort. Understanding the pathophysiology of enlarged prostate and how it impacts men’s health is essential for effective management and treatment.
What is BPH?
BPH, or benign prostatic hyperplasia, is a condition where the prostate gland grows larger, often causing urinary problems. This growth can lead to symptoms such as frequent urination, weak urine flow, and difficulty starting urination. These symptoms can significantly affect a man’s quality of life, making it important to address them promptly.
Causes and Risk Factors
The exact cause of BPH is not fully understood, but several factors contribute to its development. Age, genetics, and hormonal changes are key risk factors. As men age, the risk of developing BPH increases, making it a common condition in older men. Understanding these risk factors can help in early detection and management of BPH.
Signs and Symptoms
The symptoms of BPH can vary from mild to severe and include:
- Frequent urination
- Weak urine flow
- Difficulty starting urination
- Urinary urgency
- Urinary incontinence
Recognizing these symptoms early can help in managing BPH effectively and improving overall men’s health.
Diagnosis and Treatment Options
Diagnosing BPH typically involves a combination of physical examination, medical history, and diagnostic tests such as a digital rectal exam (DRE) and prostate-specific antigen (PSA) blood test. Treatment options range from lifestyle changes to medication and, in severe cases, surgery. Effective bph management is critical to alleviate symptoms and improve quality of life.
FAQ
Q: What is Benign Prostatic Hyperplasia (BPH)?
BPH is a non-cancerous growth of the prostate gland. It causes urinary symptoms in men, mainly as they get older.
Q: What are the symptoms of BPH?
BPH symptoms include weak or interrupted urine flow. Men may also urinate more often, wake up at night to use the bathroom, and have trouble starting or stopping urination.
Q: What causes BPH?
BPH is caused by hormonal changes, genetics, and age. These factors lead to the prostate gland growing larger.
Q: How is BPH diagnosed?
Doctors diagnose BPH through medical history, physical exams, and tests. These include a digital rectal exam, PSA test, and urodynamic studies.
Q: What are the treatment options for BPH?
Treatments for BPH include watchful waiting, medications, and surgery. Medications like alpha-blockers and 5-alpha-reductase inhibitors are used. Surgery, such as TURP, is also an option.
Q: How does BPH affect quality of life?
BPH can greatly affect a man’s quality of life. It causes urinary symptoms that disrupt daily activities, sleep, and overall well-being.
Q: Can BPH be prevented?
While preventing BPH is not guaranteed, a healthy lifestyle can help. Eating well and exercising regularly may reduce the risk.
Q: Is BPH a sign of prostate cancer?
No, BPH is not a sign of prostate cancer. It is a non-cancerous condition, but it can increase the risk of prostate problems.
Q: How is BPH related to hormonal changes?
BPH is linked to hormonal changes, like the conversion of testosterone to DHT. This hormone promotes prostate growth.
Q: Can BPH be treated with lifestyle changes?
Yes, lifestyle changes can help manage BPH symptoms. Maintaining a healthy weight, exercising regularly, and managing stress are beneficial.