
Psoriatic arthritis disability affects many adults in the United States, making daily life and mobility difficult. About 1.5 million adults live with psoriatic arthritis, a chronic condition that causes pain, stiffness, and inflammation in the joints.
The Centers for Disease Control and Prevention (CDC) defines a disability as any condition that limits daily activities. For those living with psoriatic arthritis disability, even simple tasks can become challenging due to pain and reduced movement.
Understanding whether psoriatic arthritis is a disability is crucial for people seeking benefits or filing disability claims. Knowing the criteria and available support can make it easier to manage both the physical and financial challenges of PsA.
Key Takeaways
- Psoriatic arthritis is a chronic condition that affects daily life and mobility.
- The CDC defines disability as a condition that impacts daily tasks.
- Individuals with psoriatic arthritis may be eligible for disability benefits.
- Filing disability claims requires understanding the condition’s impact.
- Psoriatic arthritis can significantly affect an individual’s quality of life.
Psoriatic arthritis is a chronic condition that affects both the skin and joints. It causes pain and limits movement. It impacts about 15% of people with psoriasis, usually starting between 30 and 50 years old.
What is Psoriatic Arthritis?
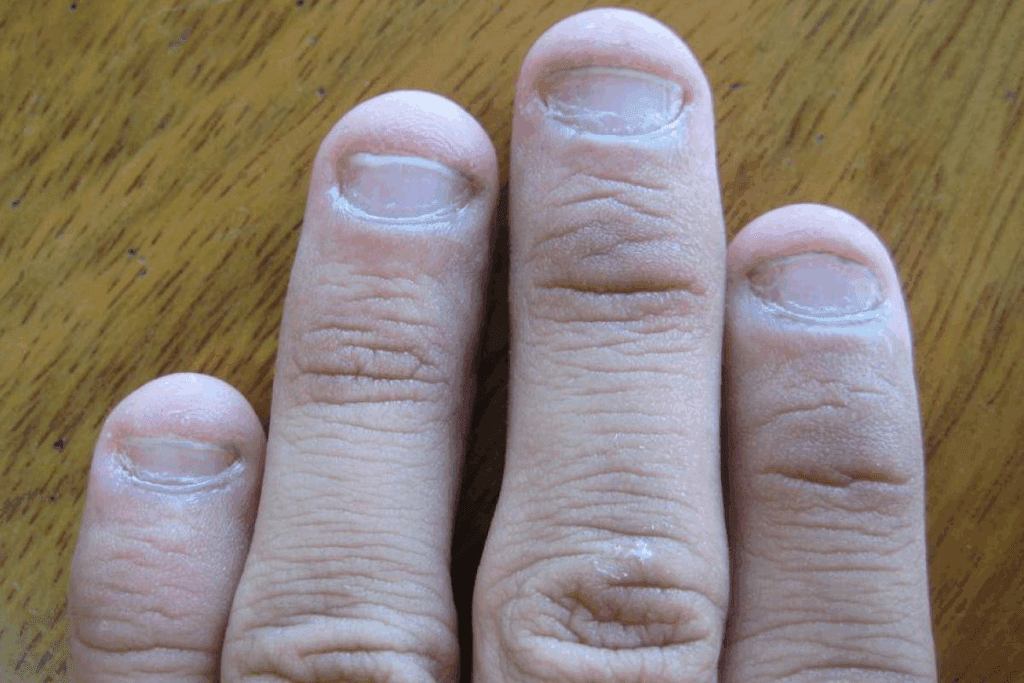
Psoriatic arthritis is a type of arthritis linked to psoriasis, a skin condition with red, scaly patches. The arthritis part brings joint pain and inflammation. This can cause limited mobility and disability if not managed well.
Common Symptoms and Manifestations
Joint Pain and Inflammation
The joint pain from psoriatic arthritis can be mild or severe. It often comes with swelling and stiffness. If not treated, it can cause deformity and permanent damage.
Skin Involvement
Skin symptoms, like psoriatic plaques, show how severe the condition is. These can be itchy and painful, making health issues worse.
Prevalence and Demographics
Psoriatic arthritis hits men and women the same, usually between 30 and 50. The severity can vary a lot among people. This affects the long-term effects on arthritis sufferers.
| Demographic | Characteristics |
| Age of Onset | Typically between 30 and 50 years |
| Gender Distribution | Affects men and women equally |
| Prevalence in Psoriasis Patients | Affects approximately 15% of people with psoriasis |
The Impact of Psoriatic Arthritis on Daily Life
Psoriatic arthritis affects many parts of life, including physical health, mood, and social interactions. People with PsA face various challenges that impact their quality of life.
Physical Limitations and Mobility Challenges
Psoriatic arthritis can limit physical abilities and make moving hard. Joint pain, stiffness, and swelling make simple tasks hard, like getting dressed or cooking. Even walking can be tough, and some may need help with daily tasks.
Pain Management Struggles
Managing pain is key for those with PsA. The condition can cause long-lasting pain that affects both body and mind. Finding good ways to manage pain is vital to reducing the emotional toll of chronic pain.
Psychological and Emotional Effects
The mental and emotional effects of PsA are significant. The ongoing nature of the condition and its impact on looks and abilities can cause deep emotional pain.
Depression and Anxiety
People with PsA are more likely to feel depressed and anxious. The constant fight against symptoms, the unpredictability of flare-ups, and the daily challenges can lead to sadness and worry.
Social Isolation
Social isolation is a common issue for those with PsA. The physical and pain issues can make it hard to join in social activities, leading to feelings of loneliness and isolation.
Understanding how PsA affects daily life is crucial. This knowledge helps in finding ways to manage not just the physical symptoms but also the mental and emotional ones.
Psoriatic Arthritis Disability: Medical Classification

It’s key to know the medical classification of psoriatic arthritis. This helps healthcare providers, patients, and the Social Security Administration (SSA) figure out the disability level.
Psoriatic arthritis ranges from mild to severe. The SSA uses this range to classify it. They look at how many joints are affected, the inflammation level, and other symptoms like skin psoriasis.
Functional Impairment Assessment Tools
Healthcare providers use functional impairment assessment tools to gauge disability. These tools check how well patients can perform daily tasks and work-related activities. The Health Assessment Questionnaire (HAQ) and the Arthritis Impact Measurement Scales (AIMS) are common tools used.
| Assessment Tool | Description | Use in Psoriatic Arthritis |
| HAQ | Measures the patient’s ability to perform daily activities | Assesses functional impairment |
| AIMS | Evaluates the impact of arthritis on various aspects of health | Assesses overall health status |
Progressive Nature of the Condition
Psoriatic arthritis gets worse over time if not managed well. It has flare-ups and remission cycles. These cycles can greatly affect a person’s life and work ability.
Flare-ups and Remission Cycles
Flare-ups are when symptoms get worse, and remission is when they get better. Understanding how PsA affects daily life is crucial.is helps keep functional ability and prevents long-term damage.
Legal Definition of Disability in the United States
In the United States, the legal definition of disability is mainly set by the Americans with Disabilities Act (ADA). The ADA outlines what makes someone disabled under the law.
Americans with Disabilities Act (ADA) Criteria
The ADA says a disability is a physical or mental issue that greatly limits major life activities. This includes conditions like psoriatic arthritis, which can really affect someone’s daily life.
State-Specific Disability Definitions
Even though the ADA gives a federal definition of disability, states have their own rules. These rules can be different from what the federal government says.
Medical vs. Legal Disability Classifications
It’s important to know the difference between medical and legal definitions of disability. A doctor might say you have a condition, but it must also meet legal criteria to be called a disability.
Social Security Disability Benefits for Psoriatic Arthritis
SSDI Eligibility Requirements
To get SSDI, you need to have worked and earned certain work credits. The number of credits needed depends on your age when you became disabled.
Work Credits and Qualifications
The SSA figures out work credits based on how much you earned. You usually need 40 work credits. At least 20 of these must have been earned in the last 10 years before you got disabled.
SSI Considerations for Limited Income Individuals
SSI is for people with little income and few resources. You must show you need the money and have a serious disability. Your work history doesn’t matter as much.
The Blue Book Listing for Inflammatory Arthritis
The SSA’s Blue Book lists different disabilities, including inflammatory arthritis. To qualify, you need medical proof and meet certain criteria.
Meeting vs. Equaling the Listing
You can get benefits if your condition meets or equals the arthritis listing. Meeting the listing means your condition is severe enough to qualify automatically. Equaling the listing means your condition is as bad as the listed criteria, even if you don’t meet all of them.
Filing for Disability with Psoriatic Arthritis
Required Medical Documentation and Evidence
To apply for disability, you must provide detailed medical records and evidence. This includes:
Physician Statements
A doctor’s statement is key. It should explain the diagnosis, symptoms, and how psoriatic arthritis impacts daily life and work.
Treatment History
It’s also important to document treatment history. This includes medications, therapies, and surgeries. It shows the severity of the condition and the efforts to manage it.
The Application Process Step-by-Step
The process for applying for disability benefits has several steps:
- Initial Application: Submitting the initial application with all required documents.
- Review Process: Waiting for the review process to be completed, during which the application is assessed.
- Potential Appeal: If denied, understanding the appeal process and preparing for it.
Common Reasons for Claim Denial
Claims can be denied for several reasons, including:
- Insufficient Medical Evidence: Lack of detailed medical documentation.
- Failure to Follow Treatment Plans: Not following prescribed treatments.
- Incomplete Application: Submitting an application that’s not fully filled out.
Knowing these common reasons can help you prepare your application better. This can lower the chance of your claim being denied.
The Americans with Disabilities Act (ADA) requires employers to offer reasonable accommodations for employees with disabilities. This includes those with psoriatic arthritis. It’s important for ensuring people with psoriatic arthritis can do their job well.
Reasonable Accommodations Under the ADA
Reasonable accommodations are changes made to the workplace or job to help people with disabilities. For those with psoriatic arthritis, these can include:
- Flexible work schedules to manage flare-ups
- Ergonomic workstation adjustments to reduce strain on joints
- Modified job duties to avoid exacerbating the condition
- Telecommuting options to reduce commuting stress
Discussing Your Condition with Employers
Talking about psoriatic arthritis with employers can be tough. But it’s a key step to get the help you need. Be ready to explain how your condition affects your work and suggest possible solutions.
Disclosure Strategies
When you tell your employer about psoriatic arthritis, it helps to:
- Be clear about the condition and its impact on work
- Provide medical documentation to support the need for accommodations
- Suggest specific accommodations that would be beneficial
Flexible Work Arrangements and Ergonomic Solutions
Flexible work arrangements and ergonomic solutions are important for psoriatic arthritis in the workplace. Employers can support employees in many ways, such as:
| Accommodation Type | Description | Benefit |
| Flexible Scheduling | Allowing employees to adjust their work hours | Helps manage fatigue and flare-ups |
| Ergonomic Workstations | Adjusting workstations to reduce physical strain | Reduces joint stress and discomfort |
| Telecommuting | Allowing employees to work from home | Reduces commuting stress and allows for a comfortable work environment |
Treatment Options and Their Impact on Disability Status
Managing psoriatic arthritis involves various treatments. These can greatly affect a person’s disability status. The main goal is to lessen symptoms, improve function, and boost quality of life.
Medications and Disease-Modifying Therapies
Medications are key in managing psoriatic arthritis. Disease-modifying antirheumatic drugs (DMARDs) are used to slow the disease’s progress and reduce inflammation.
Biologics and Their Effectiveness
Biologic agents, like TNF-alpha inhibitors, are very effective. They help reduce symptoms and slow disease progression in many patients. Examples include etanercept and adalimumab.
| Biologic Agent | Mechanism of Action | Common Side Effects |
| Etanercept | TNF-alpha inhibitor | Injection site reactions, infections |
| Adalimumab | TNF-alpha inhibitor | Infections, headache, rash |
Physical Therapy and Rehabilitation Approaches
Physical therapy is vital in managing psoriatic arthritis. It helps keep joints mobile, strengthens muscles, and improves function. A physical therapist can create a custom exercise plan for each person.
“Physical therapy can significantly improve functional ability and reduce pain in patients with psoriatic arthritis.” –
Journal of Rheumatology
Surgical Interventions for Severe Cases
In severe cases, surgery may be needed. This is when joint damage is significant. Surgical options include joint replacement or synovectomy to repair or replace damaged joints.
Long-term Prognosis and Disability Management
Understanding the long-term outlook for psoriatic arthritis is key. It involves knowing how the disease progresses and finding effective ways to manage it. Good management can greatly improve life quality and reduce disability for those with this chronic condition.
Disease Progression Factors
| Factor | Description | Impact on Disease Progression |
| Genetic Predisposition | Inherited traits that increase the risk of developing psoriatic arthritis. | It can accelerate disease onset and severity. |
| Environmental Triggers | External factors, such as stress or infections that can trigger or exacerbate symptoms. | It can lead to flare-ups and increased disease activity. |
| Treatment Effectiveness | The efficacy of medications and other treatments in managing symptoms. | Effective treatment can slow disease progression. |
Lifestyle Modifications for Symptom Control
Making lifestyle changes is important for managing psoriatic arthritis symptoms. These changes include dietary adjustments, regular exercise, and stress management techniques.
Dietary Changes: Eating an anti-inflammatory diet full of fruits, vegetables, and omega-3 fatty acids can help lessen symptoms.
Regular Exercise: Gentle exercises like yoga or swimming can improve joint mobility and reduce stiffness.
Maintaining Employment with Chronic Symptoms
Many people with psoriatic arthritis keep working despite their condition. Making workplace adjustments and adapting work routines can help keep productivity up.
Career Adaptations
Career adaptations might include flexible hours, ergonomic workspace changes, and regular breaks to manage fatigue and pain. Talking to employers about these needs can lead to solutions that work for everyone.
Additional Resources and Support Services
Managing psoriatic arthritis can be easier with the right help. There are many resources and support services available. They offer everything from medical advice to financial aid.
Patient Advocacy Organizations
Patient advocacy groups are key for those with psoriatic arthritis. They offer education, support, and help in navigating the condition. The National Psoriasis Foundation is a great example. They have online support groups and educational materials.
Financial Assistance Programs
Legal Aid for Disability Claims
For those with psoriatic arthritis seeking disability benefits, legal aid is essential. Specialized lawyers can guide you through the complex claim process.
Finding Specialized Attorneys
To find a good lawyer, start with your local bar association. Or, look into organizations like the National Organization of Social Security Claimants’ Representatives. They can connect you with lawyers who know disability law well.
| Resource | Description | Benefit |
| National Psoriasis Foundation | Provides education and advocacy for psoriasis and psoriatic arthritis patients. | Access to support groups and educational materials. |
| Patient Access Network Foundation | Offers financial assistance for patients with psoriatic arthritis. | Help with medication costs and copays. |
| National Organization of Social Security Claimants’ Representatives | Provides referrals to attorneys specializing in disability law. | Assistance in navigating disability claims. |
Conclusion
Understanding how PsA affects daily life is crucial.
The outlook for people with psoriatic arthritis varies a lot. Some have mild symptoms, while others face big challenges. Disability support services are key in helping those affected. They help manage the condition and deal with disability claims.
When looking at disability claims, it’s important to think about both physical and mental effects. Knowing all about the condition helps people get the support they need. This way, they can keep their independence and quality of life.
FAQ
What is psoriatic arthritis, and how does it affect daily life?
Psoriatic arthritis is a chronic condition that causes joint pain and skin issues. It makes everyday activities hard, affecting your mobility and overall health.
Can psoriatic arthritis be considered a disability under the Americans with Disabilities Act (ADA)?
Yes, it can be seen as a disability under the ADA. This is if it limits major life activities like walking or doing manual tasks.
What are the eligibility requirements for Social Security Disability Insurance (SSDI) benefits for psoriatic arthritis?
To get SSDI benefits, you need a condition that the SSA calls a disability. You must have worked, paid Social Security taxes, and earned enough work credits.
How does the SSA evaluate disability claims for psoriatic arthritis?
The SSA looks at how severe your symptoms are and how they affect your daily life. They use the Blue Book listing for inflammatory arthritis to decide.
What are the common reasons for claim denial for psoriatic arthritis disability benefits?
Claims are often denied for not having enough medical proof. Or if your condition doesn’t meet the SSA’s disability standards. Lack of evidence about your symptoms and how they limit you is another reason.
What workplace accommodations are available for individuals with psoriatic arthritis?
The ADA requires employers to make reasonable accommodations. This can include flexible work hours, ergonomic tools, and job duty changes to help you do your job well.
How do treatment options impact disability status for psoriatic arthritis?
Treatment can change your disability status. Medications and therapies can reduce symptoms and slow disease progression. This can help you qualify for disability benefits.
What lifestyle modifications can help manage psoriatic arthritis symptoms?
To manage symptoms, try to stay healthy, exercise regularly, and manage stress. These lifestyle changes can improve your overall health and well-being.
Are there resources available to support individuals with psoriatic arthritis?
Yes, there are many resources. Patient advocacy groups, financial help programs, and legal aid services can offer support and guidance.
Can individuals with psoriatic arthritis maintain employment despite chronic symptoms?
Yes, with the right management and accommodations, many people with psoriatic arthritis can keep working. They can continue to be productive despite their chronic symptoms.
References
- Coates, L. C., Helliwell, P. S. (2024). Psoriatic arthritis. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547710/




































