Pregnancy brings many changes to the body, some of which raise the risk of serious issues like blood clots in the lungs. Women expecting a baby are more likely to get these clots. This is because their body makes more clotting factors and blood flow decreases. At Liv Hospital, we stress the need to spot the signs of pulmonary embolism during pregnancy.

Coughing up blood or feeling short of breath can signal a serious problem. Medical studies show pregnant women are five times more likely to get a pulmonary embolism than others. The risk is highest in the third trimester and the first six weeks after giving birth.
Key Takeaways
- Pregnant women are at a higher risk of developing blood clots due to increased clotting factors.
- Recognizing symptoms like shortness of breath and coughing up blood is critical.
- Pulmonary embolism is a major cause of maternal deaths.
- Liv Hospital offers top-notch medical care for pregnant women.
- Quick diagnosis and treatment are key to managing pulmonary embolism.
Understanding the Dangers of Blood Clots During Pregnancy
Pregnancy brings many changes to the body, some of which can raise the risk of blood clots. We need to understand the dangers of blood clots during pregnancy. This includes knowing about pulmonary embolism and why pregnant women are more at risk.
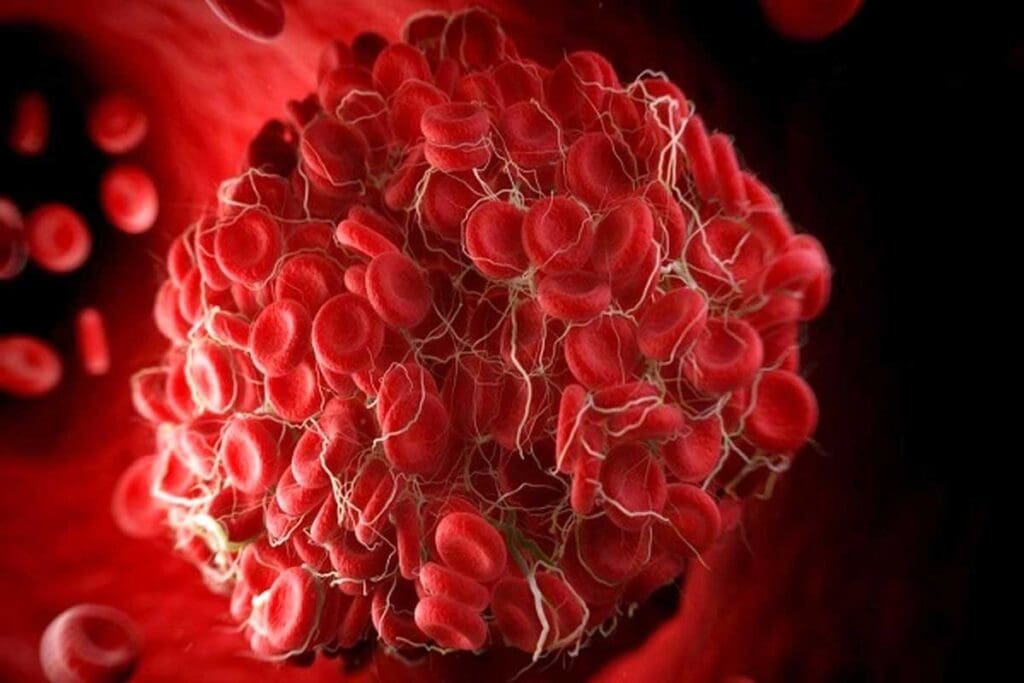
What is a Pulmonary Embolism?
A pulmonary embolism happens when a blood clot breaks loose and goes to the lungs. It blocks an artery and can be deadly. Pregnant women are at higher risk because their body’s blood volume and clotting factors increase.
Pregnant women face a higher risk of blood clots due to body changes. The growing uterus can block blood flow in the lower body veins. The body also makes more clotting factors to prepare for childbirth, which can lead to clots.
Why Pregnant Women Face Increased Risk
Pregnancy raises the risk of blood clots, including DVT and pulmonary embolism. This risk is even higher after giving birth. It’s important to understand these risks to manage them.
The body’s changes during pregnancy, like more blood and vein pressure, increase the risk. Age, obesity, and pre-existing conditions can also raise this risk.
| Risk Factor | Description | Impact on Pregnancy |
| Increased Clotting Factors | The body produces more clotting factors to prepare for childbirth. | Heightened risk of forming unwanted clots. |
| Pressure on Veins | The growing uterus can impede blood flow in the veins. | Increased risk of deep vein thrombosis. |
| Age and Obesity | Pre-existing factors that can increase the risk of blood clots. | Additional risk during pregnancy and postpartum. |
Pregnant women should know the signs of pulmonary embolism. These include sudden shortness of breath, chest pain, and coughing up blood. If they experience these symptoms, they should get medical help right away.
The 7 Critical Symptoms of Pulmonary Embolism Pregnancy Complications
It’s vital for pregnant women to know the signs of pulmonary embolism. This condition happens when a blood clot blocks a lung artery. It’s dangerous and can be deadly if not treated fast.
Pregnant women face a higher risk because of pregnancy changes. These changes can affect blood flow and clotting.
1. Sudden Shortness of Breath
Sudden shortness of breath is a key sign of pulmonary embolism. It can happen without warning and isn’t tied to exercise. As Dr. Sarah Johnson, an obstetrician, notes, “Sudden dyspnea, or shortness of breath, is a red flag that should not be ignored, specially in pregnant women.”
2. Chest Pain That Worsens with Deep Breathing
Chest pain from pulmonary embolism can be sharp. It often gets worse with deep breaths or coughs. This pain might seem like other, less serious issues. But, if it’s severe or comes with other symptoms, get medical help right away.

3. Coughing Up Blood or Blood-Streaked Mucus
Coughing up blood or blood-streaked mucus is a serious sign. It means you need to see a doctor fast. This symptom, along with shortness of breath or chest pain, could mean you have a pulmonary embolism.
4. Rapid or Irregular Heartbeat
A fast or irregular heartbeat might signal a pulmonary embolism. The clot in the lungs can stress the heart. This can cause arrhythmias or tachycardia. If your heart beats fast or irregularly, and you have other symptoms, get help right away.
Pregnant women should know these symptoms and act fast if they happen. As
“Pulmonary embolism is a medical emergency, and prompt treatment is critical to avoid serious outcomes.”
stresses the need for quick action.
Risk Factors for Pulmonary Embolism in Pregnancy
It’s key for doctors to know the risk factors for pulmonary embolism in pregnant women. This helps them give better care and prevent problems. Several things can make a pregnant woman more likely to get a pulmonary embolism.
Pre-existing Medical Conditions
Some medical conditions before pregnancy can raise the risk of pulmonary embolism. For example, clotting disorders like factor V Leiden or antiphospholipid syndrome can make blood clots more likely. Women who have had previous venous thromboembolism are also at higher risk. Heart disease and obesity can also make pregnancy riskier and increase the chance of pulmonary embolism.
Pregnancy-Specific Risk Factors
Pregnancy makes a woman more likely to form blood clots. Some pregnancy-specific factors can make this risk even higher. For example, women who have a cesarean delivery face a higher risk than those who have vaginal deliveries. Postpartum hemorrhage and other delivery complications can also raise the risk. Conditions like preeclampsia can also increase the risk because they affect clotting.
Lifestyle and Environmental Factors
Lifestyle and environment also play a big part in the risk of pulmonary embolism during pregnancy. Smoking is a big risk factor because it harms the heart and increases blood clot chances. Long periods of immobility, whether from travel, bed rest, or other reasons, can also raise the risk. Being overweight or obese not only increases blood clot risk but also makes pregnancy and childbirth harder.
Knowing these risk factors is key to preventing and catching pulmonary embolism early in pregnancy. Doctors can spot women at higher risk and take steps to prevent it. They can also keep a close eye on these women during their pregnancy and after they give birth.
Diagnosis and Treatment of Pulmonary Embolism During Pregnancy and the SMB
Diagnosing and treating pulmonary embolism in pregnant women is a careful process. It aims to keep the mother safe while also protecting the fetus. The health of the mother affects the fetus, so treatments must consider both.
Diagnostic Approaches Safe for Pregnant Women
Choosing the right tests to diagnose pulmonary embolism in pregnant women is key. Ultrasound is often the first choice because it’s safe and works well for finding deep vein thrombosis. A ventilation-perfusion (V/Q) scan is preferred for direct pulmonary embolism diagnosis because it uses less radiation.
When a V/Q scan is done, it’s important to follow protocols to reduce radiation. The choice of test depends on the situation, how far along the pregnancy is, and local expertise.
Treatment Options and Management
The main treatment for pulmonary embolism in pregnancy is anticoagulant therapy. This helps prevent more clots and dissolves existing ones. Low molecular weight heparin (LMWH) is the preferred choice because it’s safe for both the mother and the fetus.
In severe cases, more aggressive treatments like thrombectomy might be needed. This involves surgically removing the clot. The mother’s condition and the fetus’s health are closely monitored, and delivery plans are made.
Preventing further problems is also important. This includes watching for signs of more clotting and managing risk factors. Teaching patients about the signs of pulmonary embolism and the need to seek help quickly is also key.
Conclusion
It’s very important to know the signs of pulmonary embolism during pregnancy. This includes sudden shortness of breath, chest pain, and coughing up blood. We also talked about the factors that make it more likely to happen.
Pregnant women and doctors need to be on the lookout for these signs. At Liv Hospital, we focus on giving top-notch care to pregnant women. We stress the need for quick medical help to avoid serious problems.
By knowing the symptoms, how to diagnose, and treatment options for pulmonary embolism in pregnancy, we can help pregnant women. Our goal is to provide the best healthcare possible. We also offer support and guidance to international patients.
FAQ
What are the symptoms of a pulmonary embolism during pregnancy?
Symptoms include sudden shortness of breath and chest pain that gets worse with deep breathing. Coughing up blood or blood-streaked mucus is also a sign. Rapid or irregular heartbeat is another symptom. It’s important to seek medical help right away if you notice these signs.
Why are pregnant women at a higher risk for pulmonary embolism?
Pregnancy changes the body in ways that increase blood clot risk. This includes higher clotting factors and less blood flow. Cesarean delivery and postpartum hemorrhage are also pregnancy-specific risks.
How is pulmonary embolism diagnosed during pregnancy?
Safe tests like ultrasound and ventilation-perfusion scans are used. These tests check for blood clots in the lungs.
What are the treatment options for pulmonary embolism during pregnancy?
Treatment includes anticoagulant medication and thrombectomy. The goal is to prevent further complications and manage the condition effectively.
Can coughing up blood during pregnancy be a sign of pulmonary embolism?
Yes, coughing up blood or blood-streaked mucus can be a sign. It’s important to seek immediate medical attention if you experience this symptom.
How can I reduce my risk of developing a pulmonary embolism during pregnancy?
Be aware of risk factors like pre-existing medical conditions and pregnancy-specific risks. Lifestyle factors like smoking and prolonged immobility also play a role. Discussing your risk factors with your healthcare provider can help you take preventive measures.
What is the significance of recognizing the symptoms of pulmonary embolism in pregnancy?
Recognizing symptoms is key because prompt diagnosis and treatment can improve outcomes. Pulmonary embolism is a serious condition that can be life-threatening if not treated promptly.
Are there any specific risk factors that increase the likelihood of a blood clot in the lung during pregnancy?
Yes, specific risk factors include pre-existing medical conditions like clotting disorders. Pregnancy-specific risks like cesarean delivery and lifestyle factors like smoking also increase risk. Being aware of these can help in taking preventive measures.
References
- Simcox, L. E., et al. (2015). Pulmonary thrombo-embolism in pregnancy: diagnosis and management. Thrombosis Research, 135(2), S1–S7.
- Cueto-Robledo, G., et al. (2023). Pulmonary Embolism During Pregnancy: An Updated Review. Thrombosis Update, 12, 100123.


































