Last Updated on November 27, 2025 by Bilal Hasdemir

A brain tumor diagnosis and surgery can change your life. At Liv Hospital, we focus on your care and quality of life for the long term.
Surviving and recovering from brain tumor surgery depends on many things. This includes the tumor type, where it is, and how well you respond. Studies found that people with both low-grade and high-grade gliomas face similar challenges in their quality of life.
We aim to help you not just survive but also thrive after surgery. In this article, we’ll share seven key facts about survival and recovery. These insights will guide you on your path to healing and getting back to your life.
Key Takeaways
- Understanding the factors that influence survival and recovery after brain tumor surgery.
- The importance of complete care in boosting long-term quality of life.
- Insights into the prevalence of low Health Related Quality of Life (HRQoL) in glioma patients.
- Seven vital facts about survival and recovery that every patient and family should know.
- The role of Liv Hospital in providing top-notch healthcare for international patients.
The Reality of Brain Tumor Diagnosis and Treatment

Diagnosing and treating brain tumors is a complex task. It involves knowing the tumor’s type, grade, and characteristics. The type and grade of the tumor greatly affect treatment choices and results.
Types and Grades of Brain Tumors
Brain tumors can be either benign or malignant. Their grade shows how aggressive they are. Studies show that mood disorders and low quality of life in patients with certain brain tumors are linked to cognitive issues, treatments, and tumor traits.
How Tumor Characteristics Affect Treatment Decisions
Location Considerations
The tumor’s location is key in planning surgery and assessing risks. Tumors in critical areas may need more careful techniques to prevent harm.
Size and Growth Rate Factors
The size and how fast a tumor grows also matter in treatment planning. Larger or quicker-growing tumors might need more intense treatments.
| Tumor Characteristic | Influence on Treatment |
|---|---|
| Location | Surgical approach and risk assessment |
| Size | Aggressiveness of treatment |
| Growth Rate | Urgency and type of intervention |
The brain tumor operation success rate depends on these factors. The success rate of brain surgery changes based on the tumor’s details. Knowing these helps in making better care choices.
Fact 1: The Initial Recovery Journey After Surgery

It’s key for patients and their families to know about the recovery after brain tumor surgery. The first days after surgery are all about watching over the patient closely. This is when they start to get better physically and mentally.
The Critical First 48 Hours Post-Operation
The first 48 hours are very important. Patients usually stay in a recovery unit where doctors watch their brain closely. Close monitoring helps catch any problems early and helps the patient recover smoothly.
Week One: Managing Immediate Side Effects
In the first week, dealing with pain, swelling, and tiredness is a big task. We help patients feel better by giving them the right medicine and care.
The One-Month Milestone: When Many Return to Baseline
By the one-month mark, many patients start to feel like themselves again. This is a key time to see how well they’re doing physically and mentally.
Physical Recovery Markers
How well a patient can do everyday things shows how they’re physically recovering. Rehabilitation therapies are very important in helping patients get back to normal.
Cognitive Function Improvements
How fast patients get back to normal thinking can vary. Some get there quickly, while others take longer. Cognitive rehabilitation is customized to help each patient.
The journey to recovery after brain tumor surgery is complex. It needs careful watching, the right care, and rehabilitation. Knowing about the recovery milestones helps patients and their families face the challenges and opportunities ahead.
Fact 2: Brain Tumor Survival Rates After Surgery
Knowing about brain tumor survival rates after surgery is key for patients and their families. It helps them understand treatment and recovery better. Survival rates depend on the tumor’s grade, the patient’s age, and their overall health.
Low-Grade Tumor Survival Statistics
Patients with low-grade gliomas have a better chance of survival. Research shows that their 10-year survival rate can be up to 70% to 80% with the right treatment.
High-Grade Tumor Prognosis
On the other hand, high-grade gliomas have a worse outlook. Patients with these tumors have a lower 1- to 3-year survival rate. Despite aggressive treatment, their median survival is only 12 to 18 months.
How Age and Overall Health Impact Survival
Age and overall health are key in determining survival rates. Younger patients with fewer health issues tend to do better. We will look into how these factors affect survival rates.
The Role of Genetic Markers
Genetic markers are becoming more important in predicting prognosis. Some genetic mutations suggest a better or worse outlook. This helps doctors tailor treatments to each patient’s needs.
Impact of Treatment Compliance
Following the recommended treatment plan is vital for survival. Adhering to surgery, radiation, and chemotherapy plans greatly influences patient outcomes.
Key factors influencing brain tumor survival rates after surgery include:
- Tumor grade and type
- Patient age and overall health
- Genetic markers
- Treatment compliance
Understanding these factors helps patients and their families face the challenges of brain tumor treatment and recovery.
Fact 3: Brain Tumor Operation Success Rate Factors
It’s important to know what makes brain tumor surgery successful. It’s not just about removing the tumor. It’s also about keeping brain function and improving quality of life.
Defining Surgical Success: Beyond Tumor Removal
Surgery for brain tumors is more than just removing the tumor. It’s also about not harming the brain around it. Successful surgery leads to better patient outcomes and longer survival.
Success Rates by Tumor Type and Location
The success of brain surgery depends on the tumor type and where it is. For example, tumors that are not aggressive and are easy to reach have better success rates. But tumors that are aggressive or hard to get to are more challenging.
Technological Advances Improving Outcomes
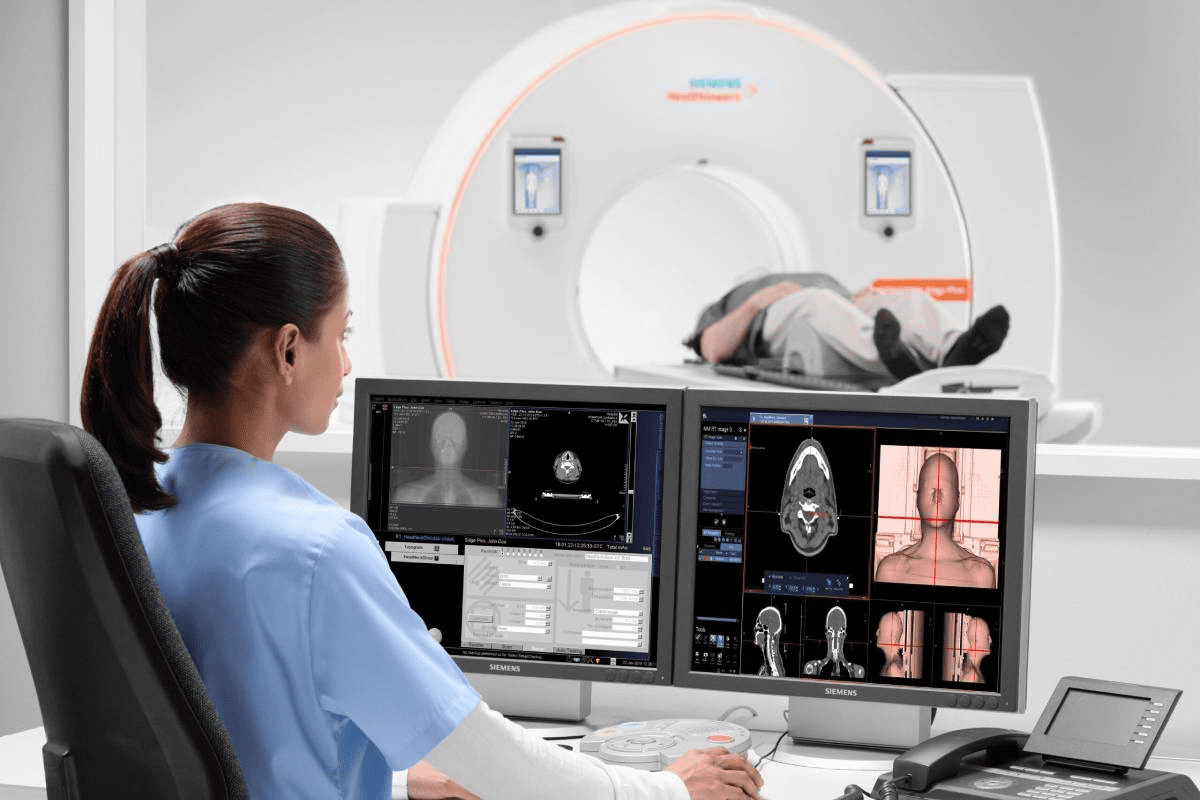
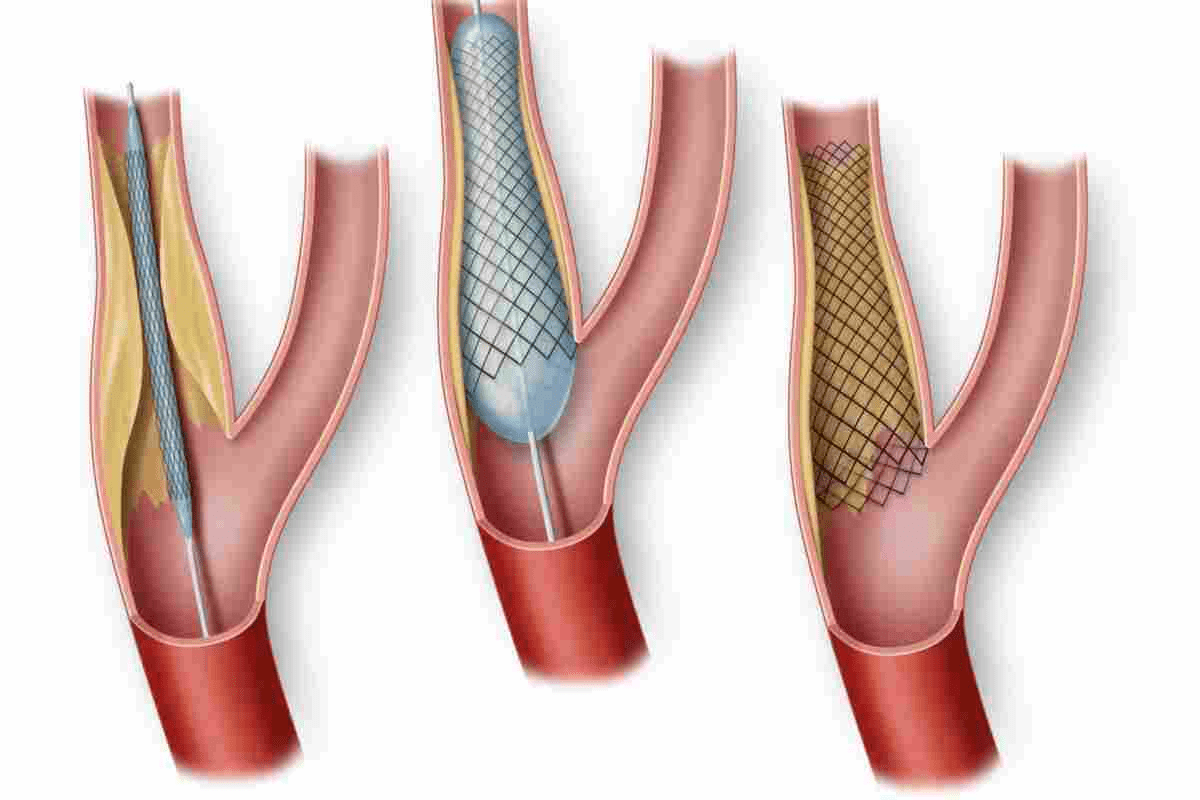
New technologies have greatly improved brain tumor surgery success rates. Tools like intraoperative imaging and awake craniotomy have changed the game.
Intraoperative Imaging
Intraoperative imaging lets surgeons see the tumor and brain tissue in real-time during surgery. This helps them remove the tumor more accurately.
Awake Craniotomy Benefits
Awake craniotomy keeps the patient awake during surgery. This lets surgeons check brain function as they work. It’s very helpful for tumors near important brain areas.
Neurosurgeons use advanced techniques and know a lot about tumors to improve patient results. Technologies like intraoperative imaging and awake craniotomy have been key in making brain tumor surgery more successful.
Fact 4: Quality of Life After Brain Tumor Surgery
After brain tumor surgery, patients focus on improving their quality of life. This journey is unique for each person, touching on physical, cognitive, and emotional health.
Physical Function and Independence Assessment
Being physically strong and independent is key after surgery. Patients might struggle with weakness, fatigue, or balance issues. Healthcare teams use these assessments to create personalized recovery plans.
Cognitive Performance and Adaptation
Cognitive health is also vital. Patients might deal with memory loss or trouble focusing. Special programs help improve cognitive skills, making daily life easier.
Emotional Well-being and Mental Health
Emotional health is a big part of recovery. Patients may feel anxious, depressed, or grieve. It’s important to tackle these feelings for a full recovery.
Managing Depression and Anxiety
It’s key to manage depression and anxiety. This might include therapy, counseling, or medication.
Addressing Body Image and Identity Changes
Changes in appearance can affect self-esteem. Support from loved ones and groups can help patients adjust. This support is essential for rebuilding self-image.
Healthcare teams aim to improve patients’ lives after surgery. This involves a detailed approach, covering physical, cognitive, and emotional aspects. It’s about providing full support for a better quality of life.
Fact 5: Frontal Lobe Tumor Surgery Survival Rate and Outcomes
The survival rate after frontal lobe tumor surgery depends on many factors. These include the tumor’s type and grade, the patient’s health, and the surgery’s techniques.
Unique Challenges of Frontal Lobe Procedures
Surgery in the frontal lobe is very challenging. Tumors in this area can affect personality, decision-making, and motor control. This makes precise planning very important.
Survival Statistics for Early Detection Cases
Early detection of frontal lobe tumors greatly improves survival chances. Studies show that early diagnosis leads to better outcomes. Some reports suggest a survival rate of up to 90% for low-grade tumors.
| Tumor Type | Survival Rate | Factors Influencing Outcome |
|---|---|---|
| Low-Grade | Up to 90% | Early detection, surgical precision |
| High-Grade | Varied, generally lower | Tumor aggressiveness, patient health |
Personality and Executive Function Changes
Frontal lobe tumors can cause big changes in personality and executive function. Patients may experience changes in behavior, emotional regulation, and cognitive processing. These changes can affect their quality of life.
Rehabilitation Strategies for Frontal Lobe Deficits
Rehabilitation is key for patients recovering from frontal lobe tumor surgery. Tailored rehabilitation programs help improve cognitive and motor functions.
Family Adjustment to Behavioral Changes
Family members need to adjust to the patient’s behavioral changes after surgery. Support and education for families are essential in managing these challenges.
Fact 6: Cognitive and Emotional Changes After Tumor Removal
After brain tumor removal, many people face cognitive and emotional changes. These changes can vary a lot. They depend on the tumor’s size, location, and the person’s health.
Memory and Attention Difficulties
Brain tumor surgery can make memory and attention hard. These issues can affect daily life. Neuropsychological assessments help find out where these problems come from.
Language and Communication Challenges
Some people struggle with language and communication after surgery. They might have trouble finding words or understanding complex sentences. Speech therapy can help with these problems.
Emotional Regulation and Personality Shifts
Brain tumor surgery can also change how people feel and act. Mood swings, irritability, or depression are common. Emotional support and counseling are key to recovery.
Neuropsychological Assessment Benefits
Neuropsychological assessments give deep insights into a person’s mind and feelings. They help make rehabilitation plans that fit the person’s needs.
Cognitive Rehabilitation Approaches
Cognitive rehabilitation uses many methods to improve thinking and adapting to changes. This includes memory training, attention exercises, and finding new ways to do things.
| Cognitive Challenge | Rehabilitation Approach | Benefit |
|---|---|---|
| Memory Difficulties | Memory Training | Improved recall and memory function |
| Attention Problems | Attention Exercises | Enhanced focus and concentration |
| Language Challenges | Speech Therapy | Better communication skills |
Understanding the cognitive and emotional changes after brain tumor surgery helps healthcare providers. They can offer better support and rehabilitation. This approach improves the quality of life for those recovering from brain tumor surgery.
Fact 7: Life Expectancy After Benign Brain Tumor Surgery
Patients often wonder about their life expectancy after surgery for a benign brain tumor. The good news is that many patients have a good prognosis. They often return to their normal activities.
Favorable Outcomes for Complete Resection
Studies show that removing the tumor completely leads to high survival rates. Patients with a completely removed tumor have a better outlook.
Recurrence Risks and Monitoring Protocols
Even though benign brain tumors are not cancerous, there’s a chance they could come back. Regular MRI scans are key to catch any recurrence early.
Long-term Quality of Life Considerations
Quality of life after surgery is a big concern. Physical function, cognitive performance, and emotional well-being are all important.
Return to Work Statistics
Many patients can go back to work after surgery. A big number of them start working again within a few months.
Activity and Lifestyle Modifications
Some lifestyle changes may be needed for long-term health. This includes changes in physical activity, diet, and stress management.
A study in a medical journal found that survival rates are much higher with complete tumor removal.
“Complete surgical resection of benign brain tumors offers the best chance for long-term survival and quality of life.”
| Tumor Type | Complete Resection Rate | 5-Year Survival Rate |
|---|---|---|
| Benign Meningioma | 90% | 95% |
| Benign Glioma | 85% | 90% |
Rehabilitation Pathways to Enhance Life After Brain Tumor Surgery
The journey to recovery after brain tumor surgery is complex. Rehabilitation is key to helping patients get back to normal. It helps them regain their strength and improve their life quality.
Physical Therapy Interventions
Physical therapy is essential. It focuses on strengthening, improving mobility, and balance. Personalized exercise programs help patients become independent again.
Occupational Therapy for Daily Living
Occupational therapy helps patients learn daily skills like dressing and cooking. Therapists teach strategies to cope with physical or cognitive challenges.
Speech and Cognitive Rehabilitation
Speech and cognitive therapy tackle communication and thinking issues after surgery. Speech therapy improves language, while cognitive training boosts memory and focus.
Technology-Assisted Rehabilitation
Technology is now a big part of rehab. Tools like virtual reality and computer programs offer new ways to help patients.
Home-Based Exercise Programs
Home-based programs let patients rehab in their own space. These plans are made just for them, helping them reach their goals.
| Rehabilitation Component | Goals | Benefits |
|---|---|---|
| Physical Therapy | Restore physical strength, mobility, and balance | Regain independence, confidence |
| Occupational Therapy | Relearn daily living skills | Adapt to cognitive or physical limitations |
| Speech and Cognitive Rehabilitation | Improve language, memory, and attention | Enhance communication and cognitive function |
As
“Rehabilitation is a critical component of the recovery process, enabling patients to achieve optimal outcomes and improve their quality of life.”
By adding a full rehab program to their care, patients can recover better and live more independently.
Support Systems: The Unsung Heroes of Recovery
A strong support system is key for those recovering from brain tumor surgery. The journey to recovery is not solo. Family, healthcare teams, and peer groups are essential for coping and healing.
Family Caregivers: Challenges and Resources
Family caregivers are the mainstay of support, giving emotional, practical, and medical help. Yet, this role can be tough, leading to burnout. It’s vital to have counseling, support groups, and educational tools to help caregivers stay well.
Professional Support Networks
Healthcare teams, specialists, and mental health experts are critical for recovery. They offer medical care, therapy, and psychological support. This is tailored to meet each patient’s needs.
Patient Communities and Peer Support
Connecting with others who’ve gone through similar experiences is very helpful. Patient communities and support groups let people share, get advice, and offer emotional support.
Online Resources and Forums
Online forums and social media groups are great for connecting. They’re always available, making it easy for those with busy lives or mobility issues to find support.
Local Support Group Benefits
Local groups offer face-to-face interaction, which is very valuable. They meet regularly, providing ongoing support and a sense of community.
Studies show how important these support systems are. They meet the emotional, practical, and informational needs of patients and their families. By using these resources, patients can improve their recovery and quality of life after surgery.
| Support System | Description | Benefits |
|---|---|---|
| Family Caregivers | Provide emotional, practical, and medical support | Personalized care, emotional support |
| Professional Networks | Offer medical care, therapy, and psychological support | Expert care, rehabilitation support |
| Patient Communities | Share experiences, advice, and emotional support | Community, shared understanding |
Returning to Life: Work, Relationships, and Activities
Recovering from brain tumor surgery is more than just healing. It’s about getting back to what matters, like work, social life, and hobbies. As patients get stronger, they look forward to living their lives as usual.
Workplace Accommodations and Disability Benefits
Going back to work after surgery is tough. Workplace accommodations and disability benefits are key. We guide patients through these to make their return to work easier.
Navigating Relationship Changes
Brain tumor surgery can change personal relationships. Patients might need to reconnect with loved ones or make new friends. Open communication and emotional support are vital in these times.
Finding New Purpose and Meaning
After surgery, patients might find new interests or pick up old hobbies. Activities like adaptive sports and creative outlets can be very rewarding.
Adaptive Sports and Recreation
Adaptive sports can boost confidence and improve health. Many groups offer programs for those recovering from brain tumors.
Creative Outlets for Expression
Creative activities like art, music, or writing are therapeutic. They help patients find new meaning in life.
| Activity | Benefits | Resources |
|---|---|---|
| Adaptive Sports | Improved physical health, confidence boost | Local rehabilitation centers, adaptive sports organizations |
| Creative Outlets | Emotional expression, stress relief | Art therapy programs, online creative communities |
Conclusion
The journey after brain tumor surgery is complex. Many factors affect the outcome, like the tumor type and treatment. Yet, studies show that many patients live well and survive after surgery.
Knowing the facts about survival and recovery helps patients and their families. Each person’s recovery is different. Getting support from healthcare, family, and friends is key to the best outcomes.
The survival rate and quality of life after surgery depend on the care received. We aim to offer top-notch healthcare to international patients. Our goal is to help them rebuild their lives after surgery.
FAQ
What is the brain tumor survival rate after surgery?
The survival rate after brain tumor surgery depends on the tumor type and grade. It also depends on the patient’s health. For low-grade tumors, survival rates can be high, over 10 years. High-grade tumors have a poorer outlook, usually 1-3 years.
How does the grade of the tumor impact life expectancy after brain tumor surgery?
The tumor grade is key in determining life expectancy after surgery. Low-grade tumors have a better prognosis. High-grade tumors are more aggressive and have a worse outlook.
What can I expect during the initial recovery journey after brain tumor surgery?
The first few days involve close monitoring in a recovery unit. Then, managing side effects and improving physical and cognitive function become the focus. Significant improvements are often seen within the first month.
How do tumor characteristics affect treatment decisions and outcomes?
Tumor characteristics like location, size, and growth rate are critical. They help determine the best treatment approach. These factors can influence the success of the surgery and the patient’s prognosis.
What is the success rate of brain surgery, and how is it defined?
Brain surgery success is not just about removing the tumor. It’s also about preserving neurological function and quality of life. Advances in technology have improved outcomes for many.
How does frontal lobe tumor surgery impact personality and executive function?
Frontal lobe tumors can affect personality and executive function. Surgery in this area can lead to changes in these functions. Tailored rehabilitation strategies are often necessary.
What are the common cognitive and emotional changes after brain tumor removal?
Patients may face cognitive and emotional changes after surgery. These include memory and attention issues, language challenges, and emotional shifts. Neuropsychological assessment and cognitive rehabilitation can help.
What is the life expectancy after benign brain tumor surgery?
Benign brain tumors often have a favorable prognosis after surgery. Life expectancy is generally good. But, the risk of recurrence and long-term monitoring are important.
How can rehabilitation pathways enhance life after brain tumor surgery?
Rehabilitation programs can greatly improve recovery and quality of life. These include physical therapy, occupational therapy, and speech and cognitive rehabilitation.
What support systems are available for patients and their families during the recovery process?
Family caregivers, healthcare providers, and peer communities are vital. They offer support during recovery. Resources help caregivers, and connecting with others who have gone through similar experiences can be beneficial.
How can patients return to work, rebuild relationships, and find new hobbies and interests after brain tumor surgery?
There are strategies and resources to help patients in these areas. Workplace accommodations, adaptive sports, and creative outlets can be helpful.
What is the quality of life after brain tumor surgery?
Quality of life after surgery depends on physical function, cognitive performance, and emotional well-being. Managing these aspects is key to achieving the best outcomes.
What is the brain tumor operation success rate?
The success rate of brain tumor operations varies. It depends on the tumor type and location, and the use of advanced surgical techniques. Advances in technology have improved outcomes for many patients.
References
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC9267496
- ACS Journals (Wiley Online Library) : https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.34980
- Brain Tumor Foundation : https://braintumor.org/news/what-to-expect-before-and-after-brain-surgery