Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 50% of cancer patients get radiation therapy as part of their treatment. This often happens after surgery to kill any leftover cancer cells. The timing of this treatment is very important for patient results.
Learn how soon radiation after surgery timing. Understand the typical time window for starting post-operative radiation clearly.
The goal of postoperative radiation is to get rid of any tiny cancer cells left after surgery. This lowers the chance of cancer coming back. Usually, radiation starts a few weeks after surgery, giving the body time to heal.
Key Takeaways
- Radiation therapy is a common treatment for cancer, often used in conjunction with surgery.
- The timing of radiation after surgery is critical for optimal patient outcomes.
- Postoperative radiation helps eliminate remaining cancer cells, reducing recurrence risk.
- Adjuvant radiation timing varies depending on individual patient factors.
- Understanding radiation therapy timing is essential for patients and healthcare providers.
The Basics of Post-Surgical Radiation Therapy
Radiation therapy after surgery is key in lowering cancer return risk. It aims to get rid of any cancer cells left after a tumor is removed.
What is Adjuvant Radiation Therapy?
Adjuvant radiation therapy uses high-energy particles to kill cancer cells. It’s meant to destroy any tiny cancer cells left after surgery. This helps lower the chance of cancer coming back.
Doctors decide on adjuvant radiation based on the cancer type, its stage, and surgical results. It’s often suggested for cancers at high risk of coming back or those with positive surgical margins.
Goals of Post-Surgical Radiation

The main aims of post-surgical radiation therapy are to:
- Get rid of any cancer cells left in the body
- Lower the risk of cancer coming back
- Boost survival rates
By doing this, adjuvant radiation therapy can greatly improve cancer patient outcomes. The treatment lasts several weeks. The exact time and frequency depend on the patient’s specific needs.
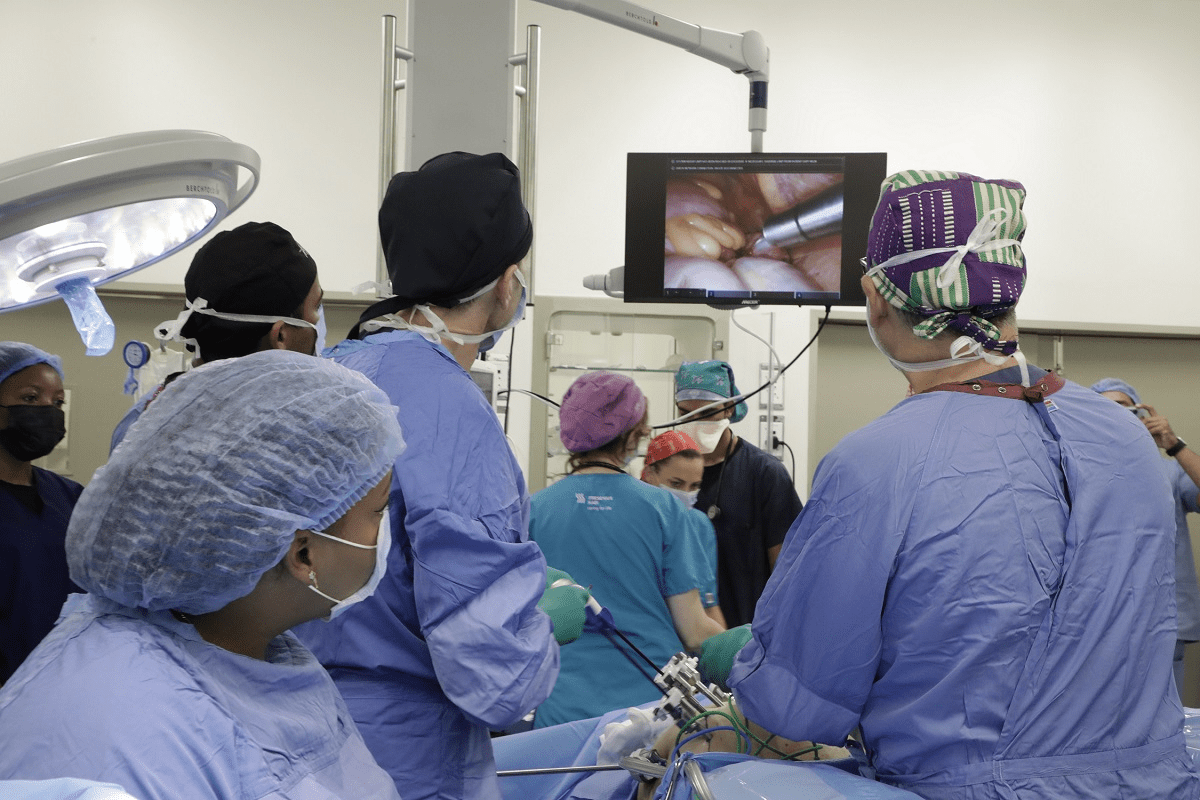
The Multidisciplinary Approach to Treatment Planning
Planning for adjuvant radiation therapy is a multidisciplinary effort. It involves a team of healthcare experts, like radiation oncologists, surgeons, and medical physicists.
This team approach ensures the treatment plan fits the patient’s unique situation. They consider the cancer type, stage, and other health factors. Together, they:
- Figure out the best radiation dose and schedule
- Identify the area to be treated
- Make a plan that reduces side effects and boosts effectiveness
Standard Timelines for Radiation After Surgery Timing
The time to start radiation therapy after surgery changes based on several things. These include the cancer type, how much surgery was done, and the patient’s health.
Typical Waiting Periods
Waiting times for radiation therapy after surgery usually last from 3 to 8 weeks. This time is needed for the wound to heal and for the patient to recover from surgery. During this period, patients go through checks to see if they’re ready for radiation therapy.
Factors Influencing Waiting Periods
- Surgical wound healing
- Pathology report analysis
- Patient’s overall health and recovery
Factors That Influence the Timeline
Many things can affect when radiation therapy starts. These include surgical complications, the need for chemotherapy, and the patient’s health status. For example, if a patient has surgery complications like infection, radiation might start later.
Statistical Averages Across Different Treatment Centers
Studies from different cancer treatment centers show that the waiting time for radiation therapy varies. While the average is 3 to 8 weeks, some centers might start earlier or later. This depends on their specific rules and the patients they see.
Knowing these timelines and factors is key for managing patient hopes and improving treatment results.
The Importance of Surgical Wound Healing
Wound healing is key before starting radiation therapy to avoid complications. Healing after surgery is complex. It involves many steps to fix the tissue.
The body’s first step is inflammation. It cleans the wound by removing debris and bacteria. Then, the proliferation phase brings new tissue and blood vessels. The remodeling phase makes the new tissue stronger.
Normal Tissue Recovery Process
After surgery, the body works hard to get back to normal. This process needs cells like fibroblasts, endothelial cells, and keratinocytes to work together. Knowing this helps doctors decide when it’s safe to start radiation therapy.
How Radiation Affects Healing Tissues
Radiation can slow down healing by harming repair cells. Radiation effects might cause wounds to heal slowly or not at all. It’s important to wait until wounds are fully healed before starting radiation.
Some tissues are more sensitive to radiation than others. For example, skin and gut tissues, with fast-growing cells, are more at risk.
Minimum Healing Requirements Before Radiation
Doctors check if wounds are healed enough before starting radiation. They look for signs like the wound being closed, no infection, and being strong enough for radiation.
Usually, wounds need 2 to 4 weeks to heal before radiation starts. But, this time can change based on the patient and the surgery type.
Cancer-Specific Radiation Timing Guidelines
Radiation therapy timing changes a lot for different cancers. This means we need specific rules for each type to get the best results. Understanding when to start radiation is key for treating cancer well.
Breast Cancer
The timing of radiation for breast cancer depends on the surgery type and risk factors. Usually, it starts 3 to 6 weeks after surgery.
- Whole breast irradiation starts 4 to 6 weeks after surgery.
- Partial breast irradiation can start sooner, based on the method used.
Prostate Cancer
When to start radiation for prostate cancer varies. It depends on the cancer’s stage, grade, and the patient’s health.
| Cancer Stage | Typical Radiation Timing |
| Low-risk | Radiation may be delayed or used as primary treatment. |
| High-risk | Often combined with hormone therapy, starting within a few months of diagnosis. |
Head and Neck Cancers
Head and neck cancers often need radiation therapy. It’s used with surgery and/or chemotherapy.
Radiation therapy usually starts 4 to 6 weeks after surgery. For more advanced cases, concurrent chemoradiation is used.
Brain Tumors
Brain tumors pose special challenges for radiation timing. This is because of their location and how they affect the brain.
The start time for radiation therapy varies. It depends on the tumor type, grade, and the patient’s brain function.
- For glioblastoma, radiation starts 2 to 4 weeks after surgery.
- For lower-grade gliomas, timing can vary, sometimes delayed for clinical reasons.
Medical Considerations That Affect Timing
Several key medical considerations play a big role in deciding when to start radiation therapy after surgery. These factors are important to make sure the treatment works well and is safe for the patient.
Pathology Results and Their Impact
Pathology results give vital information about the tumor. They tell us about the tumor’s type, grade, and how much cancer is left. Accurate pathology results are key for planning treatment.
The report also talks about the surgical margins, lymph node involvement, and any leftover cancer. These details help decide when to start radiation therapy.
Surgical Margins and Residual Disease
The status of surgical margins is very important for timing radiation therapy. If the margins are positive or close, starting radiation therapy sooner is often needed to fight any leftover cancer.
A table summarizing the impact of surgical margins on radiation timing is provided below:
| Surgical Margin Status | Impact on Radiation Timing |
| Negative Margins | Radiation therapy may be delayed based on other factors |
| Close Margins | Radiation therapy is often recommended sooner |
| Positive Margins | Radiation therapy is typically started as soon as possible |
Concurrent Chemotherapy Considerations
In some cases, radiation therapy is given at the same time as chemotherapy. This method can be good for some cancers but needs careful planning to avoid side effects.
The order of chemotherapy and radiation therapy depends on the cancer type and the patient’s health. The treatment plan is made just for the patient to get the best results.
Patient-Specific Factors in Radiation Scheduling
Radiation scheduling is not the same for everyone. It depends on many factors specific to each patient. These factors help make sure radiation therapy works best for each person, with fewer side effects.
Age and Overall Health
A patient’s age and health are very important. Older people or those with health issues might need special treatment plans. For example, older patients might need more time to heal before starting radiation.
Comorbidities and Their Impact
Having other health conditions can change how radiation is planned. Conditions like diabetes or heart disease can make it harder for the body to heal and handle radiation.
Nutritional Status
A patient’s diet is also key in planning radiation therapy. Good nutrition helps the body recover from surgery and handle radiation better. If a patient is malnourished, treatment might be delayed to fix nutritional issues first.
Performance Status Assessment
A patient’s ability to function is another important factor. Doctors use scores like the Karnofsky Performance Status (KPS) to see how well a patient can handle treatment. Patients who can do more normal activities can usually start radiation therapy sooner.
In summary, each patient’s unique factors are critical in planning radiation therapy. By looking at age, health, other conditions, diet, and how well a patient can function, doctors can tailor treatment to get the best results.
Surgical Complications and Their Effect on Radiation Timing
Surgical complications can change when radiation therapy starts. First, we must fix these issues before starting radiation.
Infection Management
Infections are common after surgery. We use antibiotic therapy to treat them. It’s key to clear the infection before starting radiation.
Having an infection means we can’t start radiation right away. The body needs to fight the infection first. Our team keeps a close eye on this to know when it’s safe to start radiation.
Wound Dehiscence Concerns
Wound dehiscence, or when the wound opens again, is another issue. We handle it with wound care and might need more surgery to close it.
Wound healing is important for starting radiation. We make sure the wound heals well to avoid problems during radiation.
Seroma and Hematoma Resolution
Seroma and hematoma are complications that can affect radiation timing. A seroma is fluid, and a hematoma is blood outside blood vessels. Both need proper management to heal and prevent infection.
Fixing seroma and hematoma is key before starting radiation. Sometimes, we need to drain them. Once they’re resolved, we can safely start radiation.
The Radiation Treatment Planning Process
Radiation treatment planning is a detailed process. It includes several key stages, from initial consultation to quality assurance. This complex process is vital for ensuring radiation therapy is delivered effectively and safely.
Initial Consultation Timeline
The initial consultation is a critical step. It happens after the patient is referred by their oncologist or surgeon. During this consultation, the radiation oncologist will assess the patient’s health and review their medical history.
They will also discuss the goals of radiation therapy. The timeline for this initial consultation can vary. But it usually happens within a few days to a week after referral.
Imaging Requirements
Imaging is vital in radiation treatment planning. Techniques like CT scans, MRI, and PET scans are used. They provide detailed information about the tumor’s location, size, and shape.
High-quality imaging is essential for ensuring the radiation dose is delivered precisely to the tumor. This minimizes exposure to surrounding healthy tissues.
Simulation and Treatment Planning Duration
The simulation process involves using imaging technologies. It defines the treatment area and determines the optimal radiation delivery technique. This stage is critical for developing a personalized treatment plan.
The duration of simulation and treatment planning varies. It depends on the complexity of the case. But it usually takes several days to a few weeks.
Quality Assurance Procedures
Quality assurance is a key part of the radiation treatment planning process. It involves verifying that the treatment plan is accurate. Quality assurance checks are performed before and during treatment to ensure the patient receives the correct dose of radiation.
These procedures help to minimize the risk of errors. They ensure that the treatment is effective.
Early vs. Delayed Radiation: The Evidence Base
Research has shown that when to start radiation therapy after surgery matters a lot. It affects how well the treatment works and how it impacts the patient’s life. Finding the best time for radiation therapy is key to getting the most out of treatment while avoiding side effects.
Research on Optimal Timing
Many studies have looked into when to start radiation therapy after surgery. They aim to find the right balance. This balance is between giving the body enough time to heal and starting treatment early enough to fight cancer.
A study in the Journal of Clinical Oncology found that starting radiation therapy early after surgery helps. It lowers the chance of cancer coming back in some patients.
“The timing of radiation therapy is a critical factor in the management of cancer. Early radiation therapy can improve outcomes by reducing the risk of recurrence.”
Cancer Recurrence Risks with Delayed Radiation
Waiting too long to start radiation therapy can raise the risk of cancer coming back. Studies show that starting treatment quickly is better. It leads to better control of the cancer and longer times without it coming back.
| Tumor Type | Early Radiation Therapy | Delayed Radiation Therapy |
| Breast Cancer | Improved local control | Increased recurrence risk |
| Head and Neck Cancer | Better disease-free survival | Higher recurrence rates |
Quality of Life Considerations
The timing of radiation therapy also affects how well a patient feels. Starting treatment early can mean less time in treatment and fewer side effects. This can make patients feel better overall.
In summary, the research clearly shows the importance of timing radiation therapy after surgery. It’s about finding the right balance to heal wounds and fight cancer. More research is needed to make guidelines better for different cancers and patients.
Logistical Factors in Radiation Scheduling
Planning radiation therapy after surgery involves many details. Several factors affect scheduling. Knowing these can help patients get ready for treatment.
Treatment Center Availability
The number of radiation therapy centers and their equipment matters a lot. Patients might have to pick from a few centers that offer the right therapy.
- Waiting lists for popular treatment centers
- Availability of specialized equipment
- Proximity to the patient’s residence
Insurance Authorization Process
The insurance process is key. Patients must check if their insurance covers the needed radiation therapy. This includes:
- Pre-authorization requirements
- Coverage limitations
- Out-of-pocket expenses
Transportation and Accommodation Arrangements
Transportation and where to stay are big concerns for radiation therapy patients. This is more so if the treatment center is far from home.
Important things to think about are:
- Daily transportation to and from the treatment center
- Accommodation options for out-of-town patients
- Potential impact on the patient’s support system
Special Circumstances Requiring Expedited Radiation
Some patients need radiation therapy quickly because of high-risk disease or aggressive tumors. The timing of this treatment is very important and must be planned carefully.
High-Risk Disease Features
Patients with big tumors, close or positive margins, or lymph node involvement might need radiation sooner. These signs show a higher chance of the disease coming back. Quick radiation can help lower this risk.
Incomplete Surgical Resection
When surgery doesn’t remove all the disease, quick radiation therapy is often needed. This is true for tumors that grow fast or are likely to come back locally.
Aggressive Tumor Biology
Tumors with aggressive traits, like high-grade features or certain molecular markers, might need quick radiation. The aim is to stop early recurrence and better outcomes for these patients.
Knowing these special cases helps doctors tailor radiation therapy for each patient. This can lead to better treatment results.
Potential Consequences of Delayed Radiation
Delaying radiation therapy after surgery can have many effects. It can affect how well the treatment works and how the patient feels. This delay can make the treatment less successful overall.
Impact on Treatment Efficacy
Delayed radiation therapy can harm the treatment’s success. If radiation is delayed, cancer can come back more easily. This is because cancer cells can grow and spread, making treatment harder.
Timely radiation therapy is key to kill off cancer cells and lower the chance of cancer coming back. Research shows that waiting too long for radiation can lead to worse outcomes in some cancers.
Tumor Repopulation Concerns
One big worry with delayed radiation is tumor repopulation. When radiation is late, cancer cells can keep growing and form new tumors. This makes the disease worse and limits treatment options.
This is a big problem in cancers that grow fast. Quick radiation therapy is needed to stop new tumors and improve treatment results.
Psychological Effects of Treatment Delays
Delayed radiation therapy also affects patients’ minds. The wait can cause stress and lower their quality of life.
Patients may worry a lot about cancer coming back. This worry can be very hard on them and affect their health. Doctors need to help patients feel better during this tough time.
Preparing for Radiation While Recovering from Surgery
Getting ready for radiation therapy after surgery is a big task. It affects how well you do during treatment. You need to get ready physically and nutritionally for the challenges of radiation therapy.
Nutritional Optimization
Eating right is key when you’re recovering from surgery and getting ready for radiation. A balanced diet with all the nutrients helps your body heal faster. It also keeps you strong during treatment.
It’s important to eat a lot of protein to help fix tissues. You should eat lean proteins like chicken, fish, and legumes. Drinking lots of water is also important. It keeps you healthy and can lessen some side effects of radiation therapy.
| Nutrient | Food Sources | Benefits |
| Protein | Chicken, fish, legumes | Tissue repair and recovery |
| Antioxidants | Fruits, vegetables, nuts | Reducing oxidative stress |
| Whole Grains | Brown rice, quinoa, whole wheat | Providing sustained energy |
Physical Therapy Considerations
Physical therapy is important after surgery. It helps you get ready for radiation therapy too. Gentle exercises can make you more mobile, reduce pain, and improve how you feel physically.
Talk to your healthcare team to make a physical therapy plan that’s right for you. This plan might include exercises to make the affected area stronger. It also helps with moving better and lasting longer. Start slow and gradually do more as you get stronger.
Skin Care Preparation
Preparing your skin for radiation therapy is very important. Radiation can make your skin red, irritated, and dry. You can take steps to get your skin ready.
Keep your skin clean and moisturized. Use gentle, fragrance-free cleansers and moisturizers. Stay away from harsh soaps, hot water, and extreme temperatures to avoid skin irritation during treatment.
- Use gentle, fragrance-free cleansers
- Apply moisturizer regularly
- Avoid harsh soaps and extreme temperatures
By focusing on nutrition, physical therapy, and skin care, you can get ready for radiation therapy while recovering from surgery. This all-around approach can improve your treatment results and make you feel better overall.
Communication Between Surgical and Radiation Oncology Teams
Good communication between surgical teams and radiation oncologists is key for better patient care. They share important information to create a complete treatment plan. This makes sure patients get the best care possible.
Working together, these teams can solve problems early and make smart decisions for patients. This teamwork is very important.
Tumor Board Discussions
Tumor board discussions help teams talk and plan together. These meetings include doctors from different fields to discuss patient cases. They work on a treatment plan that covers all aspects of care.
In these meetings, teams share information and decide on treatment options. This way, they make sure every patient gets the best care. Tumor boards are a big help in planning patient care.
Information Transfer Protocols
It’s important for teams to share patient information well. This includes sharing test results and images. Clear protocols help avoid mistakes in sharing this information.
With good protocols, teams can make sure everyone knows what’s going on with the patient. This helps in giving the best care.
| Information Type | Transfer Protocol | Responsible Team |
| Pathology Results | Electronic Health Record (EHR) System | Surgical Team |
| Imaging Studies | Picture Archiving and Communication System (PACS) | Radiology Department |
| Treatment Plans | Oncology Information System | Radiation Oncology Team |
Coordinated Follow-up Care
Following up with patients is key for ongoing care. Teams schedule check-ups and watch how patients are doing. They also handle any problems that come up.
By working together, teams can give patients seamless care. This approach improves patient outcomes and quality of life.
Patient Advocacy in Treatment Timing
Understanding radiation therapy timing is key for patients. Being proactive in your care can greatly affect your treatment’s success and timing.
Empowering Yourself with the Right Questions
To advocate for yourself, ask the right questions. Here are some important ones to ask your healthcare team:
- What is the recommended timeline for starting radiation therapy after surgery?
- How will my overall health and any comorbidities affect the timing of my radiation therapy?
- Are there any specific factors related to my cancer that could influence when radiation therapy begins?
Navigating Treatment Delays
Treatment delays can happen, even with the best plans. Knowing why and how to handle them is vital. Common causes include logistical issues, insurance authorization, and the need for more pre-treatment checks.
If delays occur, take these steps:
- Talk to your healthcare provider to understand the delay’s cause.
- Ask about possible changes to your treatment plan.
- Look for support from patient groups or counseling if delays stress you out.
Considering a Second Opinion
Getting a second opinion can give new insights into your treatment. A second opinion can offer reassurance or new views on your care plan.
“Getting a second opinion can be a key step in making sure you get the best care for your condition.”
— Oncologist
When thinking about a second opinion, ask your primary doctor for suggestions. Many cancer centers also offer second-opinion services.
Conclusion: Balancing Optimal Timing with Individual Patient Needs
Finding the right time for radiation therapy after surgery is complex. It needs careful thought about many factors. The best timing for radiation must match each patient’s needs for the best results.
We’ve looked at what affects when to start radiation therapy. This includes the cancer type, how the wound heals, medical issues, and what’s special about each patient. Knowing these helps doctors create plans that fit each patient’s unique situation.
It’s key to find the right balance for effective treatment and fewer side effects. This way, patients get the best care. It helps them have a better chance of successful treatment and feeling well overall.
FAQ
What is the typical waiting period before starting radiation therapy after surgery?
The wait time for radiation therapy after surgery varies. It depends on the cancer type, surgery extent, and health. Usually, it starts a few weeks to a couple of months after surgery, once the wound heals.
How does the multidisciplinary approach to treatment planning affect radiation timing?
A team of doctors, including surgeons and radiation oncologists, plan treatments together. This teamwork ensures radiation therapy starts at the best time, after surgery and other treatments.
What factors influence the timeline for starting radiation therapy after surgery?
Several things affect when radiation therapy starts after surgery. These include cancer type and stage, surgery extent, and if there are complications. Also, if chemotherapy or other treatments are needed.
How does wound healing affect the timing of radiation therapy?
Wound healing is key before starting radiation therapy. Radiation can harm healing, so starting too soon increases wound risks. Doctors wait until wounds heal well before starting radiation.
Are there cancer-specific guidelines for radiation timing after surgery?
Yes, different cancers have specific guidelines for radiation timing after surgery. For example, in breast cancer, radiation starts a few weeks after lumpectomy. In prostate cancer, it may be delayed several months.
How do surgical complications, such as infection or wound dehiscence, affect radiation timing?
Complications like infection or wound dehiscence can delay radiation therapy. Doctors wait until these issues are managed before starting radiation.
What is the role of pathology results in determining radiation timing?
Pathology results are very important for timing radiation therapy. They provide details on the tumor, surgical margins, and lymph nodes. This helps doctors decide if and when to start radiation.
How do patient-specific factors, such as age and overall health, influence radiation scheduling?
Age, health, and other factors can affect radiation scheduling. For example, older patients or those with health issues may need adjustments to the schedule to avoid side effects.
What is the impact of delayed radiation therapy on treatment efficacy?
Delayed radiation therapy can affect how well it works. It may let cancer cells grow. The right timing is key to make radiation effective.
How can patients prepare for radiation therapy while recovering from surgery?
Patients can prepare by eating well, doing physical therapy, and protecting their skin. They should follow their doctor’s advice and keep all appointments.
Why is communication between the surgical and radiation oncology teams important?
Good communication between teams is vital for care coordination. It ensures radiation therapy starts at the best time, providing the best care.
What questions should patients ask their healthcare team about radiation timing?
Patients should ask about radiation timing, what affects it, and any risks or benefits. This helps them understand their treatment plan better.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2804035