Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know that radiation therapy is a common treatment method for cancer, used for about 60% of all cancer patients? This highlights the significance of radiation therapy in cancer care. We keep working to make radiation therapy more accurate and successful, making it a key part of cancer treatment plans.
We aim to give top-notch healthcare, and that means looking at medical treatment outcomes closely. Learn the methods and tests used for Radiation treatment effectiveness evaluation, like follow-up scans and blood work.
Key Takeaways
- Radiation therapy is used for approximately 60% of cancer patients.
- Advances in radiation therapy have improved its accuracy and success rates.
- Evaluating medical treatment outcomes is key for high-quality patient care.
- Comprehensive cancer care includes many treatment options, like radiation therapy.
- We aim to give personalized care that fits each patient’s needs.
For those facing cancer, knowing about radiation therapy is key. It is a primary treatment that employs high-energy particles or waves to target and destroy cancer cells. Over time, it’s become better at hitting cancer cells while keeping healthy tissues safe.
What is Radiation Therapy?
Radiation therapy is a treatment that kills or controls cancer cells with ionizing radiation. It damages the DNA of cancer cells, stopping them from growing. There are two main types: external beam radiation therapy (EBRT) and internal radiation therapy.
Types of Radiation Used
External beam radiation therapy (EBRT) is the most common. It uses a machine outside the body to send beams to the tumor. This method is precise, reducing harm to nearby tissues. Internal radiation therapy places radioactive material inside or near the tumor, like seeds or pellets.
- External Beam Radiation Therapy (EBRT)
This highlights the significance of radiation therapy in cancer care.
The aim is to give a precise dose of radiation to the tumor, protecting healthy tissues. It starts with a simulation to map the treatment area. Then, a plan is made, and radiation is given over several sessions.
The Role of Radiation in Cancer Treatment
Cancer treatment often includes radiation therapy, a key part of oncology. It helps treat many cancers, improving patient outcomes and quality of life.
Common Cancers Treated with Radiation
Radiation therapy treats various cancers like blood, bone, brain, and more. Its versatility makes it a valuable treatment for many patients.
| Cancer Type | |
| Brain Cancer | Used to target tumors with precision, minimizing damage to surrounding brain tissue. |
| Breast Cancer | Often used after surgery to eliminate any remaining cancer cells. |
| Prostate Cancer | Can be used as a primary treatment or in combination with other therapies. |
Combining Radiation with Other Therapies
Radiation therapy is often paired with surgery and chemotherapy. This approach can boost treatment benefits and survival rates.
Combining radiation with surgery: Radiation can be used before surgery to shrink tumors or after surgery to eliminate any remaining cancer cells.
Example: In the treatment of breast cancer, radiation therapy is commonly used after lumpectomy to reduce the risk of recurrence.
Treatment Goals: Curative vs. Palliative
The goals of radiation therapy vary based on the patient’s condition and cancer stage. We focus on curative and palliative care.
- Curative Care: The goal is to eliminate the cancer and achieve a cure.
- Palliative Care: The focus is on relieving symptoms, improving quality of life, and managing pain.
Knowing the treatment goals helps us tailor radiation therapy to each patient’s needs. This makes the treatment more effective.
Measuring the Effectiveness of Radiation Treatment
The success of radiation treatment is measured in several ways. These include looking at how patients respond and the results of clinical trials. This helps doctors see if the treatment is working well and where it can be better.
Key Metrics in Evaluation
Several key metrics are used to check if radiation treatment is effective. These include tumor response and survival rates. These show how the cancer is reacting and the patient’s long-term chances of survival.
Other important metrics are local control and quality of life assessments. Local control shows if the treatment can stop the tumor from growing. Quality of life assessments check how the treatment affects the patient’s overall health and happiness.
Patient Response and Outcomes
How well a patient responds to radiation treatment is very important. Doctors watch how the tumor reacts and any side effects the patient has.
Outcomes are measured by cancer survival rates and the patient’s quality of life after treatment. By looking at these, doctors can make treatment better for patients.
Clinical Trials and Their Importance
Clinical trials are key in making radiation therapy better. They test new ways of treating cancer. This helps find the best treatments and improves patient results.
By joining clinical trials, researchers get important data. This data helps create more effective and tailored treatment plans for patients.
Factors Influencing Treatment Effectiveness
It’s important to know what affects how well radiation therapy works. The success of this treatment depends on many things.
Tumor Type and Location
The type and where a tumor is located matter a lot. Some tumors get better with radiation, while others don’t. This is because tumors react differently to radiation.
Where the tumor is also matters. Tumors near important organs need special care to avoid harm. Advanced methods like intensity-modulated radiation therapy (IMRT) help with this.
Individual Patient Factors
By evaluating the effectiveness of radiation therapy, we can make more informed choices for our patients.
Also, if a patient has other health issues or has had treatments before, it can change how well they do with radiation. We think about these things when deciding if radiation is right for someone.
Treatment Timing and Frequency
When and how often radiation therapy is given is very important. Doctors plan this carefully to make sure it works well and doesn’t cause too many side effects. The amount and how it’s given are adjusted for each patient and their tumor.
At times, using radiation with other treatments like chemo or surgery can make it work better. How these treatments are ordered is very important for the best results.
By evaluating the effectiveness of radiation therapy, we can make more informed choices for our patients.
Radiation therapy has both good and bad sides. It’s important to know the short-term and long-term effects. This helps us understand what to expect.
Short-Term Side Effects
Short-term side effects include fatigue, skin changes, and hair loss. These effects usually go away after treatment ends. But, they can really affect how you feel during treatment.
To manage these effects, rest is key. Eating well also helps. For skin issues, keep it clean and avoid harsh products.
Long-Term Risks
Long-term risks are also important to consider. These can include fibrosis, secondary cancers, and organ damage. Knowing these risks helps patients make informed choices.
The chance of long-term effects depends on the radiation dose and where it’s applied. For example, chest radiation might harm the heart. Pelvic radiation could affect fertility.
Managing Side Effects Effectively
It’s important to manage side effects well. This improves treatment outcomes and quality of life. Education, support, and lifestyle changes are key.
Cancer patient support is essential. It includes medical, emotional, and psychological help. Healthcare providers should educate patients on managing side effects. This makes treatment better.
By understanding the pros and cons of radiation therapy, patients and doctors can make better choices. Managing side effects well ensures patients get the most from their treatment while keeping their quality of life high.
Advances in Radiation Technology
Radiation technology has evolved, leading to more tailored and effective cancer treatments. We’ve seen big improvements in radiation therapy. These changes make treatments more precise and effective.
Innovations in Delivery Techniques
New delivery techniques have made radiation therapy more accurate. Intensity-Modulated Radiation Therapy (IMRT) and Stereotactic Body Radiation Therapy (SBRT) target tumors better. This reduces harm to healthy tissues nearby.
- IMRT changes the shape of radiation beams to match the tumor.
- SBRT uses high doses in fewer sessions, boosting treatment success for some cancers.
Personalized Radiation Treatment Plans
Personalized treatment plans are key in cancer care today. Advanced imaging and artificial intelligence (AI) help create plans that fit each patient. This boosts medical treatment effectiveness.
The future of radiation therapy is bright, with new research and technologies. Cancer treatment options and radiation therapy guidelines are getting better. New methods like proton therapy and flash radiation therapy could lead to even better results.
- Proton therapy aims to reduce side effects by targeting tumors more precisely.
- Flash radiation therapy uses high dose rates to possibly improve treatment outcomes.
As we keep improving radiation technology, we’re dedicated to top-notch patient care. We follow the latest radiation therapy assessment guidelines. This ensures our treatments are as effective as possible.
Patient Perspectives on Radiation Treatment
It’s important to see how radiation treatment affects patients. By hearing from those who have gone through it, we learn a lot. We find out how well the treatment works and what challenges patients face.
Real Patients’ Experiences
People’s experiences with radiation therapy are different. Some see big benefits, while others face tough challenges. For example, a patient might say that radiation therapy made their tumor smaller, improving their chances of survival.
This highlights the significance of radiation therapy in cancer care.
Take a breast cancer patient getting radiation therapy. They might feel tired and have skin issues but also see the treatment’s precision in targeting cancer cells. Stories like these show why personalized treatment and support are key to better outcomes.
Quality of Life Considerations
Radiation treatment can change a patient’s life a lot. They might worry about side effects, keeping their body strong, and dealing with emotional stress. We focus on improving quality of life by providing support like nutrition advice, mental health help, and rehab programs.
- Managing side effects through medication and lifestyle adjustments
- Maintaining physical function with tailored exercise programs
- Coping with emotional stress through counseling and support groups
Informed Decision-Making
It’s vital for patients to make informed choices about radiation treatment. We give them all the details about their options, including the good and bad of radiation therapy. This way, patients can choose what’s best for them based on their own situation and goals.
What affects a patient’s decision includes:
- The type and stage of cancer
- The patient’s overall health and medical history
- The impact of treatment on their quality of life
By thinking about these things and talking to their healthcare team, patients can make choices that fit their needs.
Radiation Treatment Evaluation Methods
Checking how well radiation treatment works is key. We use many methods to see if it’s effective. This makes sure patients get the best care.
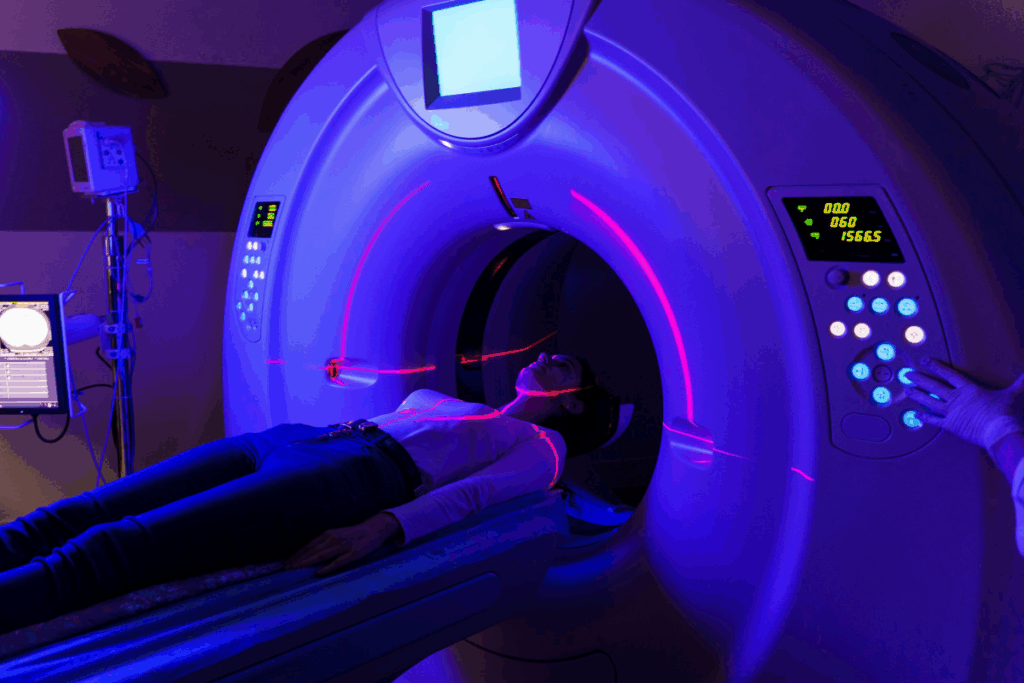
Imaging Techniques in Evaluation
Imaging is vital for checking treatment success. We use MRI, CT scans, and PET scans to see how treatment is going. These tools help us see changes in tumors and tissues. This lets us change treatment plans if needed.
Biomarkers and Their Role
Biomarkers are important for checking treatment success. We look at certain biomarkers to see how the body reacts to radiation. This helps us predict how well a patient will do and make better treatment choices.
Follow-Up Care and Monitoring
Keeping up with patients after treatment is important. We watch how they do and handle any side effects. Regular check-ups and tests help us act fast and support our patients well.
By using imaging, biomarkers, and close follow-up, we get a full picture of treatment success. This way, we can make treatment plans that fit each patient’s needs. It helps them have the best chance of a good outcome.
Radiation therapy is effective but costly. We need to look closely at its cost-benefit ratio. It’s important to consider many factors that affect its value.
Financial Considerations for Patients
The cost of radiation therapy is high, and patients often struggle financially. Out-of-pocket expenses like deductibles and copays can change a lot. We must think about these costs when we talk about the cost-benefit analysis.
To understand the financial side, let’s look at the average costs of radiation therapy:
| Treatment Type | Average Cost | Insurance Coverage |
| External Beam Radiation Therapy | $30,000 – $50,000 | Partial to Full Coverage |
| Internal Radiation Therapy (Brachytherapy) | $20,000 – $40,000 | Partial Coverage |
| Stereotactic Body Radiation Therapy (SBRT) | $40,000 – $60,000 | Partial to Full Coverage |
Insurance Coverage and Challenges
Insurance coverage is key for making radiation therapy available to patients. But, coverage limitations and pre-authorization requirements can cause delays or make things harder. We need to understand these issues to support patients better.
Some common insurance challenges include:
- Deductibles and copays
- Network restrictions
- Pre-authorization requirements
- Coverage limitations for certain treatment types
Value of Treatment vs. Cost
When we look at radiation therapy’s value, we must compare its benefits to its costs. The effectiveness of treatment, improved survival rates, and quality of life enhancements are key. Even though the costs are high, the long-term benefits often make it worth it.
By looking at both the financial and health aspects, we can fully understand radiation therapy’s cost-benefit analysis. This helps patients make informed decisions about their care.
Expert Opinions on Treatment Efficacy
Experts like oncologists and researchers weigh in on radiation treatment’s success. We’ll look at what they say to understand radiation’s role in fighting cancer.
Insights from Oncologists
Oncologists are key in deciding if radiation works for cancer patients. “Radiation therapy is a top choice for many cancers, giving patients a good chance to beat the disease.” Today, treatments are more tailored to each patient’s needs.
New tech has made radiation therapy more precise.
Perspectives from Researchers
Researchers keep working to make radiation therapy better through trials and studies. A recent study found that mixing radiation with immunotherapy can help some patients more.
“Our studies show radiation can boost the immune system, making patients respond better.” There’s growing interest in using radiation with other treatments.
Multi-Disciplinary Team Approach
Working together is key for the best patient care. Oncologists, radiologists, surgeons, and others team up to plan treatments.
When teams work together, care gets better. “A team effort means all parts of care are covered, leading to better results.” This teamwork is vital in judging radiation treatment’s success.
| Expert Opinion | Key Points |
| Oncologists | Personalized treatment plans, advanced technologies, improved patient outcomes |
| Researchers | Combining radiation with immunotherapy, optimizing treatment outcomes |
| Multi-Disciplinary Team | Comprehensive care, collaboration among healthcare professionals, better patient outcomes |
Conclusion: Is Radiation Worth It?
Looking into radiation therapy, we see it has good and bad sides for cancer patients. We need to think about both to make smart choices about treatment.
Assessing Benefits and Risks
Radiation can shrink tumors and help patients live longer. But, it also has side effects and long-term risks. It’s important to carefully look at these to make the right choice.
Personalized Care Considerations
Every cancer patient is different, and so is their treatment. It’s key to assess each case individually. This way, patients can choose what’s best for them.
Knowing the good and bad of radiation therapy helps patients make better decisions. We aim to give top-notch care to all our patients, including those from abroad. We want to ensure they get the best results.
FAQ
This highlights the significance of radiation therapy in cancer care.
It is a primary treatment that employs high-energy particles or waves to target and destroy cancer cells.
What are the different types of radiation therapy?
There are two main types. External radiation therapy sends radiation from outside the body. Internal radiation therapy places radioactive material inside the body.
How is the effectiveness of radiation treatment measured?
By evaluating the effectiveness of radiation therapy, we can make more informed choices for our patients.
What factors influence the effectiveness of radiation therapy?
The type and location of the tumor, patient health, and treatment timing matter. Knowing these helps us tailor treatments better.
What are the possible side effects of radiation therapy?
It can cause short-term side effects like fatigue and skin irritation. There are also long-term risks, like secondary cancers. We help manage these side effects.
How have advances in radiation technology improved treatment?
New delivery techniques and personalized plans have made radiation therapy better. These advances help target tumors more precisely and reduce side effects.
What role do patient perspectives play in radiation treatment decisions?
Patient experiences and quality of life are key in deciding treatments. We share real patients’ stories to help others understand radiation therapy’s impact.
This highlights the significance of radiation therapy in cancer care.
We use imaging, biomarkers, and follow-up care to check treatment success. These methods help us make informed decisions.
What are the financial considerations for radiation therapy?
Radiation therapy can be expensive, and insurance coverage varies. We discuss the cost and value of treatment to help patients make informed choices.
What do experts say about the efficacy of radiation therapy?
Oncologists and researchers agree it’s a valuable treatment for many cancers. A team approach ensures patients get the best care.
How do I know if radiation therapy is right for me?
We consider many factors, like tumor type and patient health, to decide. This helps patients make informed decisions about their care.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/16043945/
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/16043945/
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/16043945/
The Lancet. Evidence-Based Medical Insight. Retrieved from https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(06)70701-7/fulltext
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/nrclinonc2011134