Last Updated on November 26, 2025 by Bilal Hasdemir
Radiation therapy is a key part of cancer treatment. Many patients go through this therapy. About 50% of cancer patients get radiation therapy as part of their treatment.
The number of radiation therapy rounds varies a lot. It depends on the cancer type, stage, and the treatment plan.
Knowing the usual radiation dosage and what affects it is important. It helps both patients and doctors.
Key Takeaways
- The number of radiation therapy sessions varies based on cancer type and stage.
- Radiation dosage is tailored to individual patient needs.
- A significant portion of cancer patients undergo radiation therapy.
- Treatment plans are highly personalized.
- Radiation therapy is a common and effective cancer treatment.
Understanding Radiation Therapy Basics
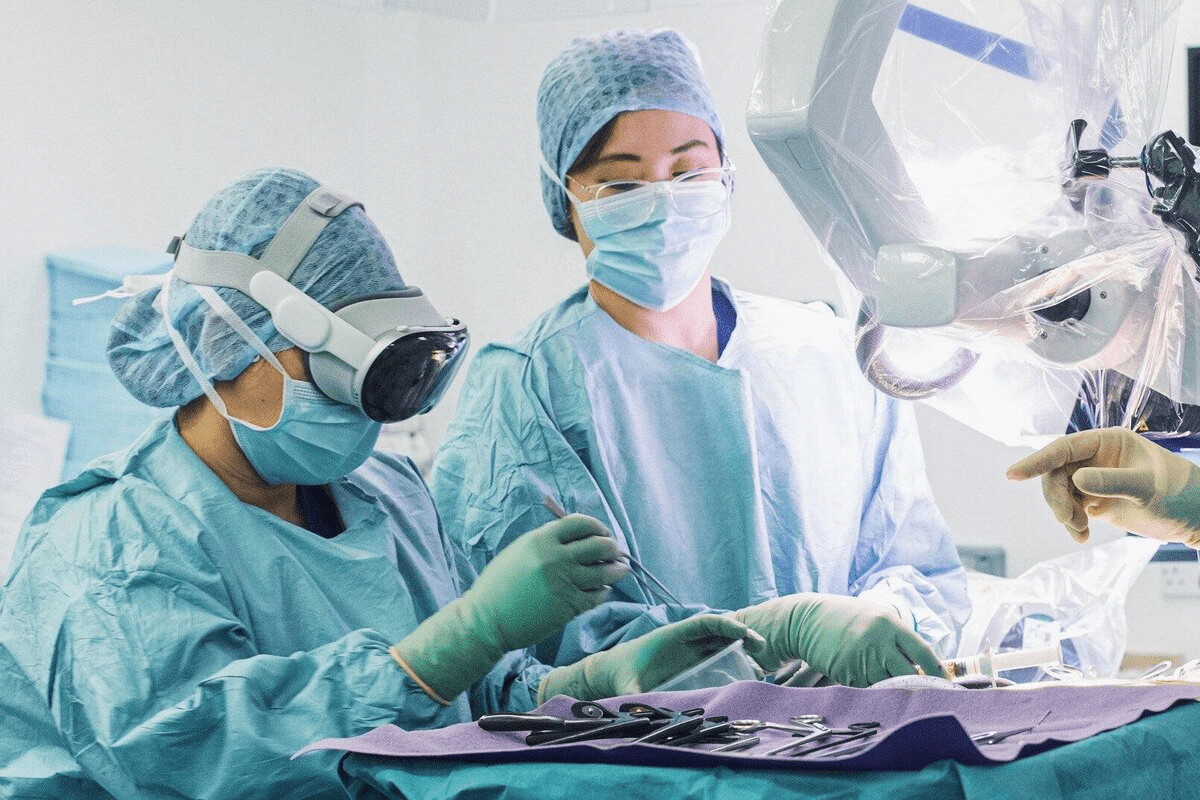
It’s important for patients with cancer to know about radiation therapy. This treatment uses high-energy particles or waves to kill or harm cancer cells.
What is Radiation Therapy?
Radiation therapy damages the DNA of cancer cells. This stops them from growing and dividing. It can be used alone or with other treatments like surgery or chemotherapy.
Types of Radiation Treatment
There are two main types of radiation therapy. External beam radiation therapy (EBRT) sends radiation from outside the body to the cancer. Internal radiation therapy (brachytherapy) places radioactive material inside or near the tumor.
How Radiation Treats Cancer
Radiation therapy targets the DNA of cancer cells. This causes damage that stops them from reproducing. The aim is to give the right amount of radiation to the tumor without harming healthy tissues.
Radiation treatment schedules vary depending on the cancer type, stage, and individual health factors. Knowing the radiation therapy cost per session helps patients plan their treatment financially.
How Many Radiation Treatments for Prostate Cancer

The number of radiation treatments for prostate cancer varies. It depends on the cancer’s specific traits.
Radiation therapy is a key treatment for prostate cancer. It comes in different forms to meet various patient needs. The goal is to be effective while keeping side effects low.
Standard Protocols for Prostate Cancer Radiation
For prostate cancer, treatments often include external beam radiation therapy (EBRT) or brachytherapy. EBRT is given daily, from Monday to Friday, for weeks. The number of treatments can be between 35 to 40, spread over 7 to 8 weeks.
- Conventional fractionation: 1.8 to 2 Gy per fraction, totaling 75.6 to 79.2 Gy
- Hypofractionation: Higher doses per fraction, reducing the total number of sessions
Factors Affecting Treatment Duration
Several things can change how long and how many treatments you need for prostate cancer. These include:
- Cancer stage and grade: More advanced cancers might need more treatment.
- Patient health: Your overall health and other medical conditions can impact how well you can handle treatment.
- Treatment goals: Whether you’re aiming for a cure or just to ease symptoms can also affect your treatment plan.
Conventional vs. Hypofractionated Treatment
Choosing between conventional and hypofractionated radiation therapy depends on several factors. These include the cancer’s characteristics and what the patient prefers.
| Treatment Type | Dose per Fraction | Total Sessions |
| Conventional | 1.8-2 Gy | 35-40 |
| Hypofractionated | Higher than 2 Gy | Fewer than 35 |
It’s important for patients to understand these factors and options. This helps them make informed decisions about their treatment.
Radiation Treatment Schedules for Breast Cancer
Knowing about radiation treatment schedules is key for breast cancer patients. It helps them understand their treatment better. Radiation therapy is a big part of breast cancer care. It comes in different schedules based on the cancer’s stage and type.
Early-Stage Breast Cancer Radiation Protocols
For early-stage breast cancer, radiation is used after a lumpectomy. It aims to kill any cancer cells left behind. The usual plan is whole breast irradiation (WBI), given daily, Monday to Friday, for 5-6 weeks. The total dose is about 45-50 Gy, with each daily dose being 1.8-2 Gy.
Some patients might get hypofractionated radiation therapy. This gives higher doses in a shorter time, usually 3-4 weeks. Studies show it works as well as the usual WBI for some patients.
Advanced Breast Cancer Treatment Schedules
For advanced breast cancer, radiation helps control symptoms or is part of a bigger treatment plan. The schedule varies a lot, depending on the patient’s needs. This includes how far the disease has spread and any treatments they’ve had before.
Advanced cancer treatment might need higher doses of radiation, up to 60 Gy or more. This is spread over several weeks. The exact plan depends on the tumor’s size, location, and the patient’s health.
Partial vs. Whole Breast Irradiation
The choice between partial breast irradiation (PBI) and whole breast irradiation depends on several things. These include the cancer’s stage, the tumor’s characteristics, and what the patient prefers. PBI targets the area around the tumor, protecting more healthy tissue.
PBI can be done in different ways, like brachytherapy or external beam radiation. It usually takes less time than WBI, often just 1-2 weeks.
By learning about the different radiation schedules for breast cancer, patients can get ready for their treatment. They can make better choices about their care.
Lung Cancer Radiation Treatment Courses
The way to treat lung cancer with radiation depends on the cancer’s type and stage. Radiation therapy is key in managing lung cancer. It can be used to cure or ease symptoms, depending on the situation.
Small Cell Lung Cancer Radiation Schedules
For small-cell lung cancer, radiation and chemotherapy are often used together. The treatment schedule can change, but it usually involves a high dose of radiation in fewer fractions. This is because small-cell lung cancer is aggressive and needs intense treatment.
Typical Treatment Schedule: Radiation for small-cell lung cancer might be given in 15 to 30 fractions over 3 to 6 weeks.
Non-Small Cell Lung Cancer Protocols
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer. Radiation therapy for NSCLC can aim to cure it, mainly in early stages. It can also be part of palliative care for more advanced cases.
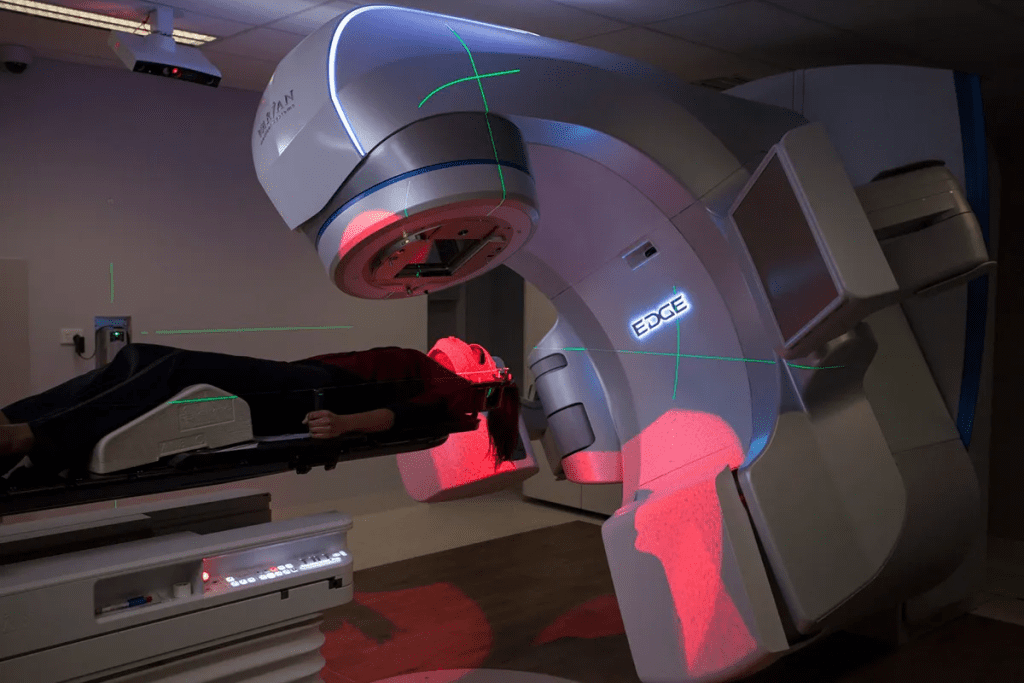
The treatment plans for NSCLC change based on the tumor’s stage and location. Stereotactic body radiation therapy (SBRT) is a precise method used for early-stage NSCLC. It delivers high doses in a few fractions.
Palliative Radiation for Lung Cancer
Palliative radiation therapy helps ease symptoms in advanced lung cancer. It can reduce pain, cough, or breathing trouble caused by tumor growth. The goal is to enhance the patient’s quality of life.
Palliative Treatment Schedules: Palliative radiation for lung cancer is usually given in a shorter course. It can be 1-5 fractions, based on the patient’s condition and symptoms.
Radiation Therapy for Other Common Cancers
Radiation therapy is key in fighting many cancers, not just prostate, breast, and lung. It’s a flexible treatment that fits different cancers, each with its own needs.
Brain Cancer Radiation Protocols
Brain cancer treatment with radiation is very precise because the brain is so delicate. The goal is to hit the tumor hard but protect the brain. Stereotactic radiosurgery (SRS) and fractionated stereotactic radiotherapy (FSRT) are the top choices for this.
“New radiation methods have greatly helped brain cancer patients,” studies show. Whether to use SRS or FSRT depends on the tumor’s size and where it is, plus the patient’s health.
Colorectal Cancer Radiation Schedules
For colorectal cancer, radiation often goes hand-in-hand with surgery and chemo. The schedule changes based on when the radiation comes before or after surgery. Preoperative radiation makes tumors smaller before surgery. Postoperative radiation targets any cancer cells left behind to lower the chance of it coming back.
- Preoperative radiation is usually 45-50 Gy over 5 weeks.
- Postoperative radiation might be more if there’s cancer left.
Head and Neck Cancer Treatment Courses
Head and neck cancer radiation is complex because of the area’s detailed anatomy. Each treatment plan is made just for the patient, considering the cancer’s location, stage, and overall health. Intensity-modulated radiation therapy (IMRT) is often used, aiming to hit the tumor right while avoiding important areas like the salivary glands and spinal cord.
“New radiation methods have greatly improved life quality for head and neck cancer patients by cutting down side effects and better tumor control.”
How long and how often head and neck cancer patients get radiation varies. But usually, they get treatment 5 days a week for 6-7 weeks.
Understanding Radiation Dosage Measurements
Knowing how to measure radiation dosage is key for treating cancer. The dosage is vital for the success of radiation therapy. It’s measured in specific units for accuracy and consistency.
Radiation therapy uses the Gray (Gy) and Centigray (cGy) to measure dosage. The Gray (Gy) is the main unit, meaning one joule of radiation energy per kilogram of matter. The Centigray is smaller, with 1 Gy being 100 cGy.
Gray (Gy) and Centigray (cGy) Explained
The Gray and Centigray are key in radiation therapy. The Gray is for larger doses, and the Centigray for smaller, more precise ones. For example, cancer treatment doses are often in Gy, with cGy for fine adjustments.
Typical Dose Ranges for Different Cancers
Each cancer type needs a different radiation dose. For example, prostate cancer might get 70-80 Gy in many fractions. Breast cancer treatment might be 40-50 Gy, also in fractions.
The dose and how it’s given depend on the cancer type, stage, location, and the patient’s health. A radiation oncologist decides the best dose and schedule based on these factors.
Fractionation: Breaking Down Total Dose
Fractionation divides the total dose into smaller parts given over time. This method helps reduce side effects and boosts the treatment’s benefits.
The fractionation schedule varies by cancer type and treatment goals. For example, curative treatments might use daily 2 Gy fractions for weeks. Palliative treatments might have larger fractions given less often.
What is Considered a High Dose of Radiation Therapy
High doses of radiation therapy are sometimes needed for cancer treatment. But they must be managed carefully to avoid side effects. The definition of a high dose depends on the cancer type, its location, and the patient’s health.
Normal vs. High Dose Radiation
Radiation therapy doses are measured in Gray (Gy). The total dose is split into fractions given over time. Normal doses can range from 8 Gy for some treatments to over 70 Gy for others.
A high dose is usually above 60 Gy, depending on the situation. Knowing the difference between normal and high doses is key. Higher doses can lead to more side effects.
Maximum Safe Radiation Doses
Finding the maximum safe dose of radiation involves looking at the tolerance of normal tissues. Different tissues can handle different doses before complications arise. For example, the spinal cord’s tolerance is low, around 45-50 Gy.
The liver can handle higher doses, up to 60 Gy or more, depending on the area treated. Radiation oncologists use guidelines and charts to find the safest dose. These are based on clinical evidence and ongoing research.
Radiation Dose Charts and Guidelines
Radiation dose charts and guidelines are vital for radiation oncologists. They help determine the right dose based on the cancer type, stage, and patient health. These are developed from clinical trials and research.
For some head and neck cancers, a 70 Gy dose is recommended. For palliative treatments, a lower dose, like 20 Gy in 5 fractions, might be used. Following these guidelines is key to safe and effective treatment.
Factors That Determine Number of Radiation Sessions
Knowing the factors that determine the number of radiation sessions is key for good treatment planning. The number of radiation therapy sessions, or fractions, changes a lot from one patient to another.
The main factors that affect how many radiation sessions a patient needs fall into three main areas. These are the type and stage of cancer, the treatment’s goal, and the patient’s specific needs.
Cancer Type and Stage
The type and stage of cancer greatly affect how many radiation sessions are needed. Different cancers react differently to radiation. The cancer’s stage also affects how aggressive the treatment should be.
- Early-stage cancers might need fewer sessions but with higher doses each time.
- Advanced cancers often require more sessions, with lower doses each time. This helps protect healthy tissues.
Treatment Intent: Curative vs. Palliative
The intent of the radiation treatment also matters a lot. The treatment’s goal can be either to cure the cancer or to ease symptoms.
- Curative treatments aim to get rid of the cancer. They use a higher total dose spread over more sessions.
- Palliative treatments focus on easing symptoms like pain or breathing trouble. They use fewer sessions but with higher doses each time.
Patient-Specific Considerations
Patient-specific factors also greatly influence the number of radiation sessions. These include the patient’s health, age, and any other health issues they might have.
| Patient Factor | Impact on Radiation Sessions |
| Age | Older patients may need adjustments in dosing and scheduling. |
| Overall Health | Patients with significant comorbidities may need modified treatment plans. |
| Previous Treatments | Patients who have had radiation therapy before may have limits on total dose. |
Radiation oncologists use these factors to create treatment plans that fit each patient. This helps ensure the best possible results from the radiation sessions.
Radiation Treatment Duration and Frequency
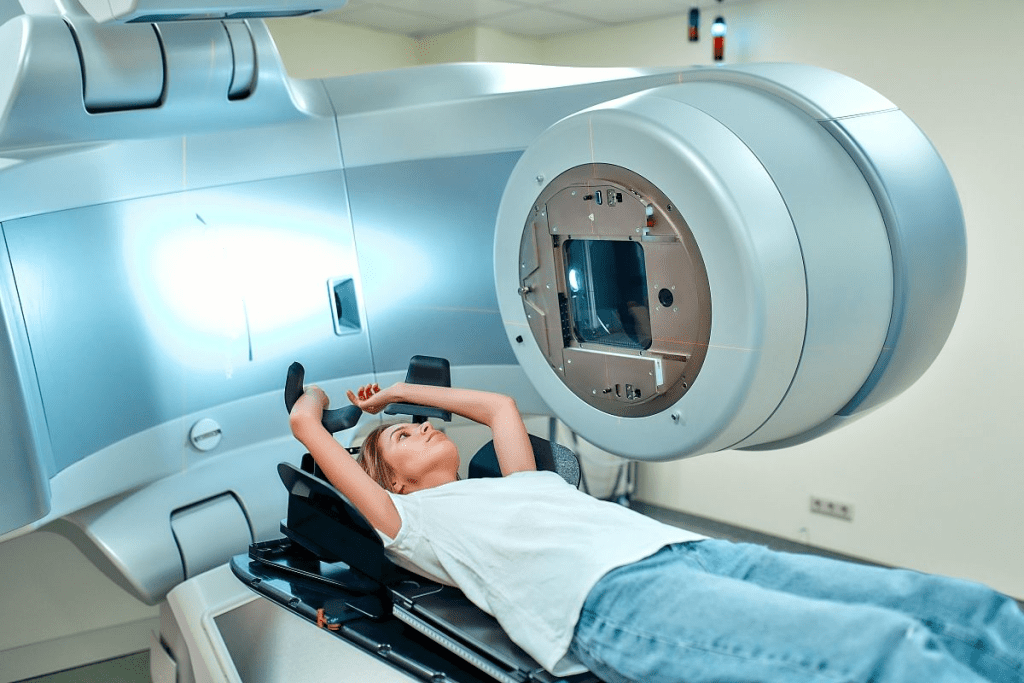
Radiation therapy can be given daily or weekly. The total time needed varies based on the treatment plan. The plan is made to fit the patient’s needs and the cancer type.
Daily Treatment Sessions Explained
Daily sessions are common for many cancers. These sessions are from Monday to Friday, with weekends off. This break helps the body recover. Each session is short, lasting just a few minutes.
Benefits of daily treatment sessions include:
- Effective management of rapidly growing tumors
- Reduced risk of cancer cells repopulating between sessions
- Potential for better treatment outcomes due to consistent dosing
Weekly Treatment Schedules
Weekly schedules are less common but used for some cases. This is often for less aggressive cancers or when the goal is to ease symptoms. This schedule might be easier for some patients and could make treatment less burdensome.
Considerations for weekly treatment include:
- Higher doses per session compared to daily treatments
- Potential for fewer side effects due to less frequent exposure
- The need for careful planning to ensure effective treatment
Total Treatment Course Timeline
The length of a radiation treatment course can vary a lot. For some cancers, treatment might last just a few weeks. For others, it could take several months.
| Cancer Type | Typical Treatment Duration | Frequency |
| Prostate Cancer | 4-8 weeks | Daily (Monday-Friday) |
| Breast Cancer | 3-6 weeks | Daily (Monday-Friday) |
| Lung Cancer | 2-7 weeks | Daily (Monday-Friday) |
It’s important for patients to understand the treatment duration and frequency. Knowing what to expect helps them manage their treatment and any side effects better.
Managing Side Effects During Multiple Radiation Sessions
Getting radiation therapy can cause different side effects, depending on where it’s aimed. Even though it’s focused, it can affect more than just the treated area. It’s important for patients to know about these side effects and how to handle them, which is key for those going through many sessions.
Common Side Effects by Treatment Area
The side effects of radiation therapy vary by area. For example:
- Head and Neck: Patients might get dry mouth, trouble swallowing, and changes in taste or smell.
- Breast: Side effects include skin irritation, feeling tired, and swelling in the treated breast.
- Prostate: Common issues are needing to urinate often, feeling urgent, and bowel changes.
- Lung: Coughing, shortness of breath, and feeling tired are common.
Fatigue and Tiredness During Treatment
Feeling fatigued or tired is a common side effect across all areas. It’s not just physical tiredness. It can also be mental or emotional exhaustion. The exact reason for this fatigue is not fully known, but it’s thought to be related to how the body responds to radiation.
To fight fatigue, patients are often told to:
- Save energy by focusing on important activities.
- Take breaks to rest regularly.
- Do gentle exercises, like walking, if their doctor says it’s okay.
Strategies to Minimize Side Effects
While some side effects can’t be avoided, there are ways to lessen their impact:
- Skin Care: For areas exposed to radiation, gentle skin care can help. Use mild soap, avoid harsh scrubbing, and apply recommended creams or ointments.
- Nutritional Support: Good nutrition is key. Eat a balanced diet, stay hydrated, and consider talking to a dietitian for advice.
- Rest and Relaxation: Getting enough rest and doing stress-reducing activities, like meditation or yoga, can help manage side effects.
Managing side effects during radiation therapy needs a team effort. This includes the patient, their healthcare team, and sometimes family and friends. By understanding the side effects and using strategies to lessen them, patients can improve their quality of life during and after treatment.
Can You Undergo Radiation Therapy More Than Once?
Whether you can have radiation therapy again depends on many things. These include the cancer type and stage, how much radiation you’ve had before, and your health.
Retreatment Considerations and Limitations
Oncologists look at a few things when thinking about giving you radiation again. They check how much radiation your healthy tissues have had and if more therapy will help. They also weigh the risks and benefits of giving you more radiation.
Key considerations include:
- The time that has passed after your first radiation therapy
- The dose and area covered by the first radiation
- How big your cancer is now
Lifetime Dose Limits for Normal Tissues
Our bodies can only handle so much radiation before it causes harm. To avoid serious side effects, doctors set limits on how much radiation you can get in your lifetime.
| Tissue | Maximum Tolerated Dose (Gy) | Complication |
| Spinal Cord | 50 | Myelopathy |
| Lung | 20-30 | Pneumonitis |
| Liver | 30-35 | Hepatitis |
Alternative Options After Previous Radiation
If you’ve had radiation therapy before, there are other treatments you might consider. These could be surgery, chemotherapy, immunotherapy, or joining a clinical trial.
The right treatment for you depends on your cancer type, what treatments you’ve had, and your health.
Conclusion: What to Expect from Your Radiation Treatment Journey
Radiation therapy is a detailed treatment that needs careful planning. It covers the basics and different cancer treatment plans. Each patient’s journey is unique.
When you start radiation therapy, knowing what to expect is key. You’ll learn about your dosage, how often you’ll get treated, and possible side effects.
Being informed helps you understand your treatment better. Your radiation oncologist and team will create a plan just for you. They’ll consider your specific needs.
Remember, your treatment team is there to support you. With their help, you can face the challenges of radiation therapy. This way, you can get the best results possible.
FAQ
What is radiation therapy?
Radiation therapy is a treatment for cancer. It uses high-energy particles or waves. These destroy or damage cancer cells, shrinking tumors and slowing growth.
How many rounds of radiation is normal?
The number of treatments varies. It depends on the cancer type and stage, treatment goals, and patient factors. Treatments can range from a few sessions to several weeks of daily treatments.
What is the standard measure of energy in radiation treatment?
The standard measure is the Gray (Gy). One Gy is the energy absorbed by one kilogram of matter per joule.
How does radiation treat cancer?
Radiation therapy damages cancer cells’ DNA. This stops them from dividing and growing. It leads to cell death and tumor shrinkage.
Can you have radiation therapy more than once?
Yes, in some cases. It depends on the initial dose, treatment area, and patient factors.
What is considered a high dose of radiation therapy?
A high dose is above 60 Gy. This can vary based on cancer type, treatment intent, and patient factors.
How long does radiation therapy last?
Its duration varies. Some treatments last minutes, while others require daily sessions for weeks.
How often are radiation treatments given?
Treatments are usually given daily, Monday through Friday. Some schedules may involve weekly or hypofractionated treatments.
What are the common side effects of radiation therapy?
Side effects include fatigue, skin changes, hair loss, and nausea. The specific effects depend on the treatment area and patient factors.
Can radiation therapy cure cancer?
It can cure cancer in some cases. This depends on the cancer type and stage. It’s often used with other treatments like surgery and chemotherapy.
How much is radiation therapy?
Costs vary by treatment center, location, and patient factors. It’s generally a costly treatment option.
What is the success rate of radiation therapy?
Success rates vary by cancer type and stage. It’s an effective treatment for many cancers.
Is radiotherapy the same as radiation therapy?
Yes, they’re often used interchangeably. Some sources may distinguish between the two terms.
How many radiation treatments are normal for breast cancer?
Treatments for breast cancer vary by stage and type. It’s usually around 15-30 treatments.
How many radiation treatments are normal for prostate cancer?
Treatments for prostate cancer vary by stage and type. It’s usually around 20-40 treatments.
What is the maximum number of radiation treatments?
The maximum varies by patient factors and treatment intent. It’s generally around 30-40 treatments.
Can you find your way through a maze with radiation?
No, radiation is not a navigational tool. It can’t be used to find one’s way through a maze.
What is gy in radiation?
Gy, or Gray, is the standard unit of measurement. It represents the absorption of one joule of radiation energy per kilogram of matter.
What is the abbreviation for radiotherapy?
The abbreviation for radiotherapy is RT.
How long is a radiotherapy session?
Session length varies by treatment center and patient factors. It’s usually around 10-30 minutes.
References
- National Cancer Institute. (2024, February). Radiation therapy to treat cancer. U.S. Department of Health and Human Services. https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy