.About 30% of breast cancer patients receive radiotherapy radiation oncology as part of their treatment. This shows how important radiation oncology is in fighting breast cancer.
Radiotherapy radiation oncology for breast cancer is a detailed process. It involves sending radiation exactly to the tumor sites. Knowing how it’s given helps patients make better choices about their car
Key Takeaways
- The importance of radiation oncology in breast cancer treatment.
- Overview of how radiation therapy is administered.
- Benefits and possible side effects of breast cancer radiation therapy.
- The role of oncology services in supporting patients.
- Insights into the latest advancements in radiation therapy.
Understanding Breast Cancer Radiation Therapy Basics
It’s key for patients to understand breast cancer radiation therapy basics. This knowledge helps them make better choices about their care. Radiation therapy is a big part of breast cancer treatment. It kills any cancer cells left after surgery, lowering the chance of cancer coming back.
The Role of Radiation in Breast Cancer Treatment
Radiation therapy is very important in treating breast cancer. It’s used a lot after surgeries like lumpectomy or mastectomy. It helps by getting rid of tiny cancer cells that might be left behind in the breast, chest wall, or lymph nodes.
Doctors decide if radiation therapy is needed based on several things. These include the cancer’s stage, the type of surgery, and the patient’s health.
When Radiation Therapy is Recommended
Radiation therapy is often suggested for those who had a lumpectomy. It’s also for some who had a mastectomy, if the cancer was big or spread to lymph nodes. It’s also considered for patients with high-risk features, like close or positive margins.
Goals of Radiation Treatment
The main goal of radiation therapy is to get rid of any cancer cells left behind. This helps prevent cancer from coming back and improves survival chances. It targets areas where cancer is likely to return, making sure it doesn’t.
Also, radiation therapy tries to keep the breast looking and working like normal. This is important, mainly for those who had a lumpectomy.
Types of Radiation Therapy for Breast Cancer
There are several types of radiation therapy for breast cancer. Each has its own benefits and uses. The right choice depends on the cancer’s stage, tumor size and location, and the patient’s health.
External Beam Radiation Therapy
External beam radiation therapy (EBRT) is the most common treatment. It uses high-energy beams from outside the body to target the tumor. Patients usually get treatment daily, Monday through Friday, for weeks.
Benefits of EBRT: It precisely targets tumors, reducing harm to healthy tissues.
Internal Radiation (Brachytherapy)
Brachytherapy places radioactive material close to the tumor. This method delivers a high dose of radiation to cancer cells while protecting healthy tissues.
“Brachytherapy offers a promising approach for delivering targeted radiation therapy, potentially reducing side effects and improving outcomes for breast cancer patients.”
Radiation Oncologist
Types of Brachytherapy:
- Permanent brachytherapy, where the radioactive material is left in place permanently.
- Temporary brachytherapy, where the material is removed after a certain period.
Intraoperative Radiation Therapy
Intraoperative radiation therapy (IORT) delivers radiation directly to the tumor during surgery. It’s often used for patients having a lumpectomy.
| Type of Radiation Therapy | Description | Benefits |
| External Beam Radiation Therapy | High-energy beams directed from outside the body | Precise targeting of tumors, minimizing damage to healthy tissues |
| Brachytherapy | Radioactive material placed directly into or near the tumor | Higher dose of radiation to cancer cells, reduced exposure to healthy tissues |
| Intraoperative Radiation Therapy | Single dose of radiation delivered during surgery | Effective for patients undergoing lumpectomy, potentially reducing recovery time |
Each radiation therapy type has its own benefits. The right choice depends on the patient’s specific situation. Knowing these options helps patients make informed decisions about their treatment.
The Science Behind Radiotherapy Radiation Oncology

Radiation oncology targets cancer cells without harming healthy tissue. “Radiation therapy is a highly effective treatment for breast cancer, giving a significant chance of cure,” says a leading radiation oncologist.
How Radiation Targets Cancer Cells
Radiation therapy damages cancer cells’ DNA, stopping them from growing. It uses high-energy particles or waves aimed at the tumor. The goal is to kill cancer cells while protecting healthy tissue.
Precision is key in radiation therapy. New radiation technology lets doctors tailor treatments for each patient. This improves results and lowers side effects.
Radiation Dosage and Measurement
The radiation dose is carefully planned to fight cancer without harming healthy tissue. Dosage is measured in Gray (Gy). One Gy is the energy absorbed by one kilogram of matter.
- Radiation dosage is tailored to the individual patient’s needs.
- The total dose is often fractionated, or divided, into multiple smaller doses.
- This fractionation allows healthy cells to recover between treatments.
Radiation Biology and Cancer Cell Death
The effect of radiation on cancer cells is complex. It involves many pathways leading to cell death. Understanding radiation biology is key to better treatment plans.
“The biological response to radiation involves a complex interplay of cellular and molecular processes that can lead to the death of cancer cells,” according to recent studies in molecular cancer research.
By knowing how radiation targets cancer cells and the importance of precise dosage, doctors can create effective treatment plans. This improves patient outcomes.
The Radiation Planning Process
The journey to successful radiation therapy starts with a detailed planning process. This process is tailored to each patient’s needs. It’s key to ensure radiation therapy is delivered safely and effectively.
Initial Consultation with Radiation Oncologist
The first step is a meeting with a radiation oncologist. The oncologist will check the patient’s health and medical history. They will also discuss the cancer diagnosis. This meeting helps decide the best radiation therapy plan.
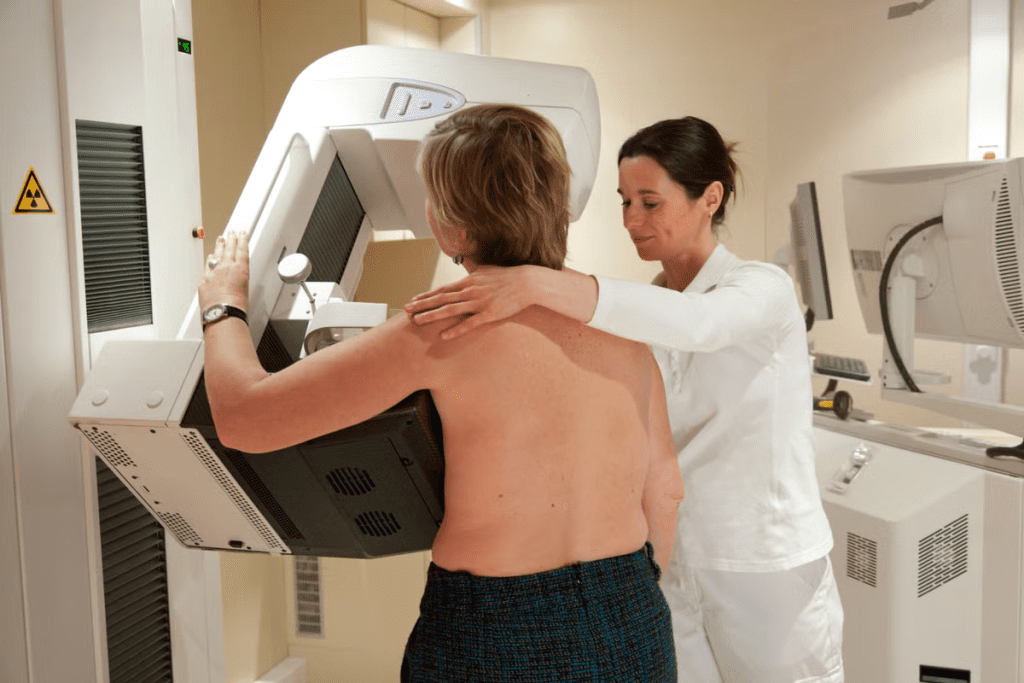
Imaging and Simulation
Next, imaging and simulation follow. This includes CT scans, MRI, or PET scans. These scans help find the tumor’s exact location and size. The patient is then positioned for a personalized treatment plan.
Treatment Planning and Dosimetry
Treatment planning and dosimetry are key steps. The oncologist, medical physicists, and dosimetrists work together. They create a plan to target the tumor with the right dose of radiation, while protecting healthy tissues. Dosimetry ensures the radiation dose is accurate and meets the plan.
| Step | Description | Key Professionals Involved |
| Initial Consultation | Assessment of patient’s health and cancer diagnosis | Radiation Oncologist |
| Imaging and Simulation | Imaging tests to locate the tumor and plan treatment | Radiation Oncologist, Radiologic Technologists |
| Treatment Planning and Dosimetry | Development of a personalized treatment plan | Radiation Oncologist, Medical Physicists, Dosimetrists |
The radiation planning process is detailed and requires a team of experts. By planning each step carefully, radiation oncologists ensure patients get the best treatment. This targeted approach helps patients receive effective therapy.
The Radiation Oncology Team
Radiation oncology needs a team with different skills and specialties. This team works together to make sure patients get the best radiation therapy.
Roles of Radiation Oncologists
Radiation oncologists are doctors who use radiation to treat cancer. They decide the best radiation treatment for each patient. They consider the cancer type, stage, and the patient’s health.
Key responsibilities include:
- Evaluating patients to determine if radiation therapy is appropriate
- Developing a personalized treatment plan
- Monitoring the patient’s progress during treatment
- Adjusting the treatment plan as necessary
Medical Physicists and Dosimetrists
Medical physicists and dosimetrists are key in the radiation oncology team. Medical physicists make sure the radiation equipment works right and doses are correct.
Dosimetrists work with the radiation oncologist to plan the treatment and calculate the dose.
Their key responsibilities include:
- Calculating the radiation dose
- Developing and implementing the treatment plan
- Ensuring the accuracy of radiation delivery
Radiation Therapists and Oncology Nurses
Radiation therapists run the radiation equipment and give the treatment. Oncology nurses care for patients getting radiation therapy. They manage side effects and offer emotional support.
Their roles include:
- Delivering radiation treatment as planned
- Monitoring the patient’s condition during treatment
- Providing patient education and support
Working together, radiation oncologists, medical physicists, dosimetrists, radiation therapists, and oncology nurses ensure top-notch radiation therapy.
Preparing for Radiation Treatment
Before starting radiation therapy, patients go through many evaluations and preparations. This is key to make sure they’re ready for treatment. It helps the therapy work better and reduces side effects.
Medical Evaluations and Tests
Medical checks are a big part of getting ready. These tests help doctors know how the patient’s health might affect the treatment. They might include blood work, imaging studies, and more to check the patient’s health fully.
Common medical evaluations include:
- Complete blood count (CBC) to check overall health and find any issues.
- Imaging tests like CT scans or MRI to plan the treatment.
- Other tests based on the patient’s history and current health.
| Test Type | Purpose | What to Expect |
| Complete Blood Count (CBC) | Check overall health, find any problems. | A blood sample is taken and analyzed. |
| Imaging Tests (CT, MRI) | Plan the treatment, check tumor size and location. | Lie in a scanner that takes detailed images. |
Skin Marking and Positioning Devices
Skin marking is a key step in getting ready for radiation therapy. It marks the skin to help the therapists aim the treatment right. Positioning devices also help keep the patient in the right spot during treatment.
The goal of skin marking and positioning devices is to ensure precision and consistency in the delivery of radiation therapy.
Lifestyle Adjustments Before Treatment
Changing your lifestyle a bit before treatment can help you cope better. This might mean eating right, managing stress, and getting enough sleep.
Recommended lifestyle adjustments include:
- Eat a balanced diet full of nutrients to support your health.
- Drink plenty of water to stay hydrated.
- Try stress-reducing activities like meditation or yoga.
The Radiation Treatment Schedule for Breast Cancer
Breast cancer radiation therapy has a detailed treatment plan. It’s made just for each patient. This plan considers the cancer type, stage, and the patient’s health.
Standard Fractionation Schedules
Standard fractionation schedules give radiation in small doses over weeks. Patients usually get treated daily, Monday to Friday, for 5-7 weeks. This method helps protect healthy tissues around the cancer.
Benefits of standard fractionation: It’s well-studied and works well for many patients. The long treatment time lets some tissues recover between doses.
Hypofractionated Radiation Therapy
Hypofractionated therapy uses bigger doses in fewer visits, often in 3-4 weeks. It’s gaining popularity for its shorter treatment time without losing effectiveness.
Advantages of hypofractionation: It’s quicker, with fewer visits to the radiation department. It might also cause fewer side effects because of the lower total dose.
Accelerated Partial Breast Irradiation
Accelerated Partial Breast Irradiation (APBI) targets only the tumor area. It’s much shorter, usually 1-2 weeks. This method is great for early-stage cancer patients after lumpectomy.
APBI benefits: It’s faster, with less radiation to the rest of the breast. It could also mean fewer side effects. APBI is perfect for those with early-stage breast cancer.
What Happens During a Radiation Session
Understanding what happens during a radiation session can help patients feel less anxious. A radiation session is a precise procedure. It aims to deliver the right amount of radiation to the right area.
Step-by-Step Procedure
The process starts with the patient getting on a treatment table. The therapists then align the machine with marks on the patient’s skin. They use X-rays or CT scans for accuracy.
After the patient is set up, the therapists leave the room. They control the machine from another area. They watch the patient through a camera and talk to them through an intercom. The machine sends out radiation beams as planned, and this is done for the number of sessions needed.
Duration of Each Treatment
The radiation treatment duration changes based on the therapy type and plan. A session usually lasts 15 to 30 minutes. But, the actual radiation time is just a few minutes.
The rest of the time is for setting up the patient. This ensures the radiation is given correctly. How often and how many sessions depend on the cancer stage, therapy type, and treatment goals.
The Role of Radiation Therapists
Radiation therapists are key in the therapy process. They operate the machines and follow the doctor’s plan.
They work with the oncology team to make sure the patient gets the right dose of radiation. Their skill and focus are essential for safe and effective treatment.
Advanced Radiation Techniques for Breast Cancer
Advanced radiation techniques have changed how we treat breast cancer. They offer better precision and possibly better results. These new methods help doctors target tumors more accurately while protecting healthy tissue.
3D Conformal Radiation Therapy
Three-dimensional conformal radiation therapy (3D-CRT) uses advanced imaging to create a detailed 3D picture of tumors. This lets doctors deliver radiation beams that fit the tumor’s shape. It reduces harm to nearby healthy tissues.
“3D-CRT has greatly improved treatment outcomes in breast cancer,” says a top radiation oncologist.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy (IMRT) is a step up from 3D-CRT. It not only shapes the radiation beams to fit the tumor but also changes the intensity of the radiation. This makes the radiation delivery even more precise, lowering the risk to healthy tissues.
IMRT is great for complex cases or when tumors are near important structures.
Proton Therapy
Proton therapy uses protons instead of X-rays to kill cancer cells. It’s very precise and can give a high dose to the tumor while protecting nearby tissues. Proton therapy is best for tumors near critical areas or in young patients to avoid long-term radiation effects.
These advanced radiation techniques are a big leap in breast cancer treatment. They improve precision and lower side effects, making care better for breast cancer patients.
Managing Side Effects of Breast Cancer Radiation
It’s key to know and handle the side effects of radiation therapy for breast cancer patients. This therapy is vital but can cause side effects, from mild to severe.
Common Short-Term Side Effects
Short-term side effects include fatigue, skin changes, and swelling. Fatigue is common, making it hard to do daily tasks because of feeling very tired.
- Skin irritation or redness
- Swelling or tenderness in the breast
- Fatigue or feeling extremely tired
These effects are usually short-lived and go away once treatment ends.
Potential Long-Term Side Effects
Long-term side effects are less common but can happen. They include changes in breast texture, lymphedema, or rare secondary cancers. Lymphedema is swelling in the arm or hand from radiation to lymph nodes.
- Changes in breast texture or appearance
- Lymphedema or swelling in the arm
- Rarely, secondary cancers
Strategies for Side Effect Management
Managing side effects well is important for better outcomes. Good skin care, rest, and exercise help. Wearing supportive clothes can also reduce swelling.
| Side Effect | Management Strategy |
| Skin Irritation | Keep the skin clean and dry, avoid harsh soaps |
| Fatigue | Balance rest and exercise, take regular breaks |
| Lymphedema | Use compression garments, elevate the affected limb |
Knowing about side effects and using good management strategies helps patients deal with radiation therapy better.
Nutrition and Lifestyle During Radiation Therapy
When you’re going through radiation therapy, eating right and living well can make a big difference. Good nutrition helps you handle the treatment better. It also lowers the chance of side effects and keeps you healthy.
Dietary Recommendations
Eating a balanced diet full of important nutrients is key for radiation therapy patients. High-protein foods like lean meats, fish, eggs, and legumes help fix damaged tissues. Fruits and vegetables give you the vitamins and minerals you need.
Drinking lots of water is also important. Avoiding foods high in sugar and fat can help with nausea and tiredness. Talk to your doctor or a nutritionist to make a diet plan that’s right for you.
Exercise Guidelines
Doing gentle exercises during radiation therapy can help you feel less tired, happier, and more active. Low-impact activities like walking, yoga, or light stretching are good choices. But remember to listen to your body and not push too hard, when you’re feeling really tired.
Talk to your radiation oncologist before starting any exercise routine. They can make sure it’s safe for you.
Rest and Recovery Strategies
Getting enough rest and recovery is very important during radiation therapy. Try to get a regular sleep schedule and make your sleep area comfy. Short naps during the day can also help with tiredness.
Using stress management techniques like meditation, deep breathing, or reading can help you relax. This can improve your overall well-being.
Special Considerations for Different Breast Cancer Types
Understanding radiation therapy for various breast cancer types is key. Each type of breast cancer may need a special approach to radiation therapy. This depends on the cancer’s characteristics, the patient’s health, and the treatment goals.
Radiation After Lumpectomy
Radiation therapy is common after lumpectomy for early-stage breast cancer. It aims to kill any cancer cells left in the breast. This helps lower the chance of cancer coming back.
Key Considerations:
- The radiation dose and how often it’s given are planned carefully. This is to kill cancer cells while protecting healthy tissue.
- The treatment area is set to cover the tumor bed and the surrounding breast tissue.
Radiation After Mastectomy
Patients with high-risk features, like big tumors or cancer in lymph nodes, may get radiation after mastectomy. This treatment aims to lower the risk of cancer coming back in the same area.
Important Factors:
- Whether to use radiation depends on the cancer’s pathology report and other factors.
- The treatment area might include the chest wall and nearby lymph nodes.
Radiation for Inflammatory Breast Cancer
Inflammatory breast cancer is rare and aggressive. It needs quick and intense treatment. Radiation therapy is a key part of managing this disease.
| Breast Cancer Type | Radiation Therapy Approach | Goals of Treatment |
| Early-stage breast cancer after lumpectomy | Whole breast radiation therapy | Reduce risk of local recurrence |
| High-risk breast cancer after mastectomy | Chest wall and regional lymph node radiation | Reduce risk of local recurrence |
| Inflammatory breast cancer | Intensive multimodality treatment including radiation | Control disease, improve survival |
Monitoring Progress During Radiation Treatment
It’s key to watch how radiation therapy is working. This helps doctors tweak plans for better results. They can see if the treatment is effective and make changes if needed.
Regular Check-ups with Radiation Oncologist
Seeing a radiation oncologist often is very important. These visits let the doctor check how you’re doing with the therapy. They can also fix any problems or side effects and change the plan if it’s not working.
At these visits, you’ll get a full check-up and talk about any side effects. This is important for managing side effects and keeping you comfortable during treatment.
Imaging and Assessment
Imaging like CT scans and MRI are key for checking how well radiation therapy is working. They help doctors see how the tumor is reacting. This info helps them adjust the treatment to hit the cancer harder and protect healthy tissues.
“Advanced imaging techniques are integral to modern radiation therapy, enabling precise targeting of tumors and reducing the risk of damage to adjacent healthy tissues.”
Adjusting Treatment Plans
Being able to change treatment plans is a big plus of watching progress closely. If the tumor isn’t responding as hoped, the doctor can make changes. This could mean adjusting the dose, changing how often you get treatment, or adding other therapies.
- Revising the radiation dosage based on tumor response
- Adjusting the treatment schedule to optimize outcomes
- Incorporating complementary therapies to enhance effectiveness
By keeping a close eye on how you’re doing and being ready to make changes, doctors can make radiation therapy work best for breast cancer patients.
Follow-up Care After Completing Radiation
The journey doesn’t end after radiation treatment. In fact, follow-up care is key to cancer survivorship. After treatment, patients start a new phase of care. This phase focuses on monitoring health, managing side effects, and improving survival and quality of life.
Follow-up care is essential for spotting and managing late effects of radiation therapy. Regular check-ups can greatly improve health outcomes. They help catch issues early, when they’re easier to manage.
Post-Treatment Appointments
Post-treatment appointments are set up to check on the patient’s recovery. They look for signs of cancer coming back. These appointments include:
- Physical exams to check overall health and find any problems.
- Imaging tests like mammograms, ultrasounds, or MRIs to watch the treated area for signs of cancer.
- Talking about any symptoms or worries, like pain, tiredness, or changes in the treated area.
One survivor said, “Regular follow-up appointments gave me peace of mind. They helped my doctors catch any issues early.” This proactive care can really improve a patient’s quality of life.
Long-term Monitoring
Long-term monitoring is key for managing late effects of radiation therapy. This includes:
| Monitoring Aspect | Description | Frequency |
| Mammography | Annual mammograms to check for cancer coming back. | Annually |
| Thyroid Function Tests | Tests to see if the thyroid is working right, a possible late effect of radiation. | As recommended by the doctor |
| Cardiac Monitoring | Watching for heart problems that might come from radiation. | As recommended by the doctor |
Early detection of issues is key to managing them well. Regular checks let doctors address problems quickly, improving long-term results.
Managing Late Effects
Managing late effects of radiation therapy is a big part of follow-up care. Late effects can include:
- Fibrosis: Scarring in the treated area, causing stiffness or changes in skin texture.
- Lymphedema: Swelling in the arm or breast area from lymph node removal or damage.
- Cardiac Issues: Long-term heart problems, if the treatment area was near the heart.
Managing these effects often needs a team effort. This includes physical therapy, medicine, and lifestyle changes.
“The key to managing late effects is early detection and a complete care plan,” says a radiation oncologist.
In conclusion, follow-up care after radiation therapy is vital for cancer survivors’ long-term health. Understanding the importance of post-treatment appointments, long-term monitoring, and managing late effects helps patients navigate this critical phase with confidence.
Conclusion: The Future of Breast Cancer Radiation Therapy
The world of breast cancer treatment is changing fast. New discoveries in radiation oncology are making treatments better. This brings hope to those fighting the disease.
New methods like precision radiation therapy are making a big difference. They target tumors more accurately, protecting healthy tissue. This is great news for breast cancer patients, as it lowers side effects and boosts their quality of life.
The future looks bright for breast cancer radiation therapy. New technologies and techniques are on the horizon. As we learn more about breast cancer, radiation therapy will keep playing a key role. It will offer patients more effective and tailored treatments.
FAQ
What is radiation therapy and how is it used in breast cancer treatment?
Radiation therapy uses high-energy rays to kill cancer cells. It’s used in breast cancer to destroy any remaining cells after surgery. This helps ensure all cancer is gone.
What are the different types of radiation therapy used for breast cancer?
There are several types of radiation therapy for breast cancer. The most common is external beam radiation therapy. This type delivers radiation from outside the body.
How is radiation therapy planned for breast cancer patients?
Planning radiation therapy involves several steps. First, there’s an initial consultation and imaging. Then, a treatment plan is made. The team works together to create a personalized plan.
What is the role of a radiation oncologist in breast cancer treatment?
A radiation oncologist specializes in using radiation to treat cancer. They oversee the treatment plan and work with other doctors. They also monitor the patient’s progress.
How long does radiation therapy for breast cancer typically last?
Radiation therapy for breast cancer can last different amounts of time. External beam radiation therapy usually takes several weeks. Brachytherapy, on the other hand, can be completed in a few days.
What are the common side effects of radiation therapy for breast cancer?
Common side effects include fatigue, skin changes, and swelling. Long-term side effects may include changes in breast appearance and increased risk of secondary cancers.
How can patients manage side effects during radiation therapy?
Patients can manage side effects by eating healthy, staying hydrated, and exercising. They should also get enough rest and follow their doctor’s advice.
What is the importance of follow-up care after completing radiation therapy?
Follow-up care is important to monitor for cancer recurrence and manage late effects. It also helps address any concerns or questions the patient may have.
Are there any advanced radiation techniques used in breast cancer treatment?
Yes, advanced techniques like 3D conformal radiation therapy and intensity-modulated radiation therapy (IMRT) are used. These aim to target the tumor more precisely while protecting surrounding tissues.
Can radiation therapy be used after a mastectomy?
Yes, radiation therapy can be used after a mastectomy. It’s often used if the cancer was large or spread to lymph nodes. The decision depends on the cancer’s stage and type.
How does radiation therapy target cancer cells?
Radiation therapy damages cancer cells’ DNA, stopping them from dividing. It aims to deliver radiation precisely to the tumor while protecting healthy tissues
Reference
National Cancer Institute. (2015). Radiation therapy for cancer. National Cancer Institute. https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy