Last Updated on November 25, 2025 by Ugurkan Demir
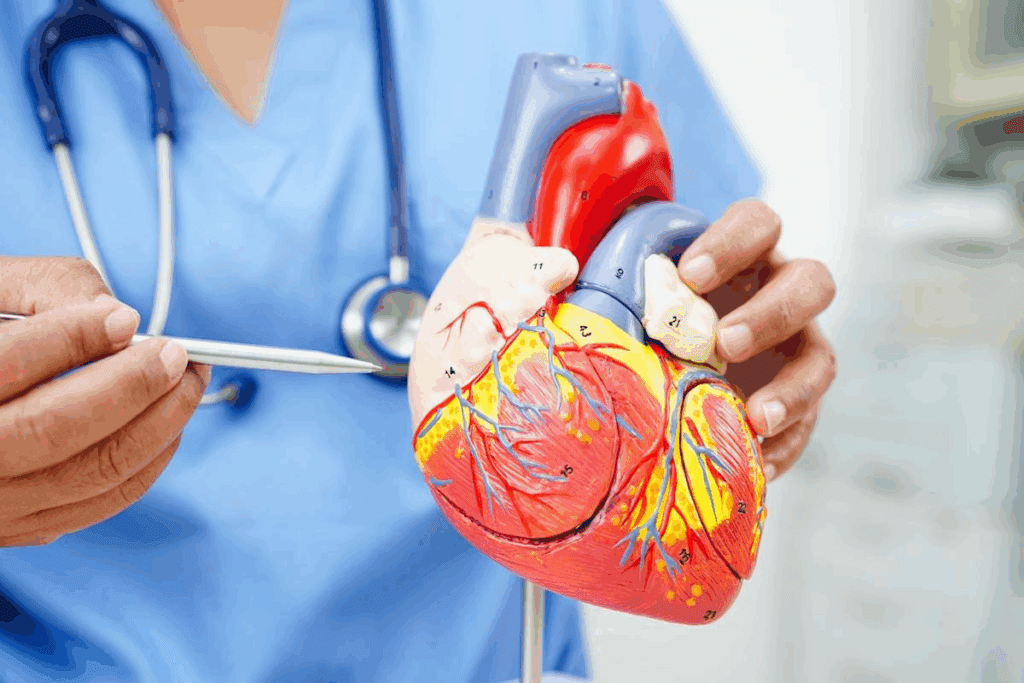
Cardiac arrest is a serious condition where the heart suddenly stops. This leads to a lack of blood flow to the body. Knowing the causes and risk factors is key to preventing and treating it. At Liv Hospital, we focus on the main reasons for cardiac arrest in different age groups.
Heart disease is the top cause of death in the U.S. Every 34 seconds, someone dies from heart disease. The reasons for cardiac arrest differ by age, making it important to know these risks.
This article will look at the 10 main reasons for cardiac arrest and how they affect different age groups. It aims to help those looking to understand and lower these risks.

Cardiac arrest is a sudden and often unexpected medical condition. It can be fatal if not treated quickly. It happens when the heart stops beating well, cutting off blood and oxygen to vital organs. We will look at what happens during cardiac arrest and how it’s different from a heart attack.
During cardiac arrest, the heart’s electrical activity stops. This can be due to heart disease, electrical issues, or severe injury. As a result, the brain and other vital organs lose oxygen and nutrients. This leads to loss of consciousness and, if not treated, death.
Immediate response is key in such cases. CPR and AEDs can help restore the heart’s rhythm. Knowing the causes and signs of cardiac arrest can greatly improve survival chances.
Cardiac arrest and heart attack are serious heart conditions, but they are different. A heart attack happens when blood flow to the heart is blocked, causing heart muscle damage. On the other hand, cardiac arrest is when the heart suddenly stops working, often due to an electrical issue.
It’s important to know that a heart attack can sometimes cause cardiac arrest. But they are not the same. Knowing the difference is key to providing the right medical response.
Cardiac arrest can happen for many reasons, from heart disease to genetic issues. Knowing these causes is key to preventing and treating it. We’ll look at the main reasons for cardiac arrest, shedding light on what leads to this serious event.
The top reason for cardiac arrest is coronary artery disease, which blocks blood flow to the heart. Other big causes include heart attacks and genetic heart rhythm problems.
Key causes of cardiac arrest include:
Cardiac arrest is a big health issue globally. It affects many people yearly, with high death rates if not treated fast. The rates vary by area and depend on age, health, and emergency care access.
Research shows low survival rates for cardiac arrest. This highlights the importance of awareness and prevention. Knowing the data helps find at-risk groups and create better prevention plans.
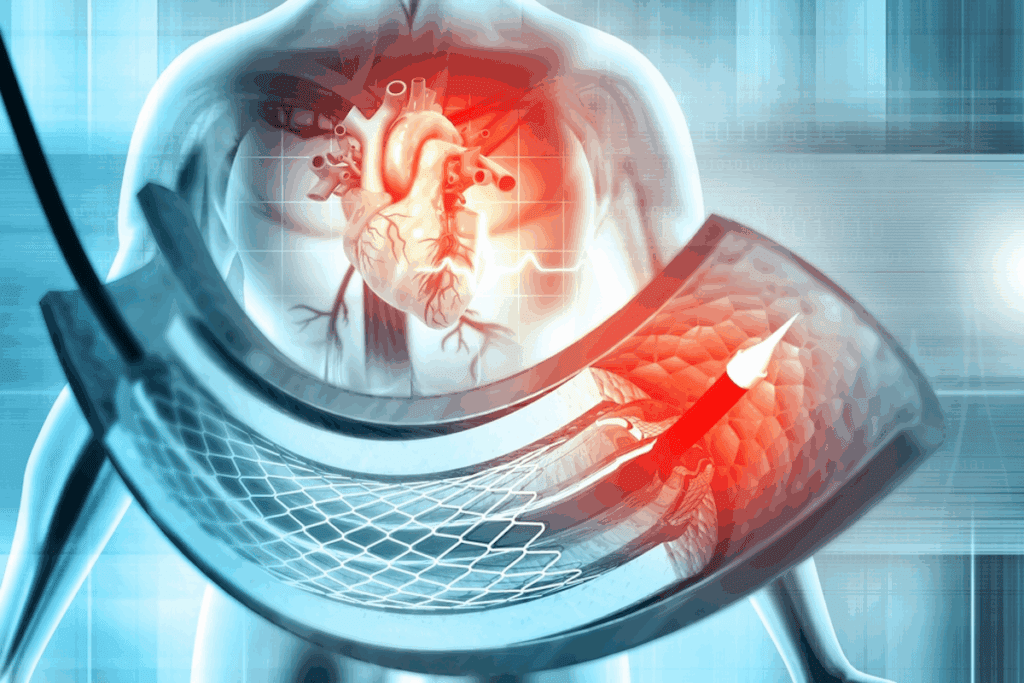
Coronary artery disease is the top reason for cardiac arrest. It happens when the main blood vessels to the heart get damaged. This damage is often due to a buildup of plaque, made of fat, cholesterol, and more, inside the artery walls.
Plaque buildup in the arteries can cause cardiac arrest in several ways. As plaque grows, it narrows the arteries, cutting down blood flow to the heart. This can lead to a blockage, causing a cardiac arrest.
Key factors that contribute to plaque buildup include:
It’s important to know the warning signs of coronary artery disease to prevent cardiac arrest. Symptoms like chest pain, shortness of breath, and fatigue are common. But, some people might not show symptoms until it’s too late.
Preventive measures include:
By understanding the risks of coronary artery disease and taking steps to manage them, you can lower your risk of cardiac arrest.
Heart attacks, or myocardial infarctions, are a major cause of cardiac arrest. This shows how important quick medical help is. A heart attack happens when blood flow to the heart is blocked, damaging the heart muscle.
This damage can mess up the heart’s electrical system. This can lead to cardiac arrest.
The move from a heart attack to cardiac arrest is serious and can be deadly. When a heart attack damages the heart muscle, it can start dangerous heart rhythms. These rhythms can be so bad they cause the heart to stop beating well.
Quick medical action is key to stop this bad sequence. We must spot heart attack signs like chest pain, shortness of breath, and feeling dizzy. Then, we must act fast.
How quickly we respond to a heart attack or cardiac arrest greatly affects survival. Quick CPR and defibrillation can greatly increase a person’s survival odds. The American Heart Association says about 1 in 5 heart attacks are silent, with no clear symptoms but can cause cardiac arrest.
Survival rates for cardiac arrest vary a lot. For example, cardiac arrest in a hospital has a much better survival rate than outside. In the U.S., someone has a heart attack every 40 seconds. Quick action is vital to stop cardiac arrest.
Understanding the link between myocardial infarction and cardiac arrest helps us see why fast medical help is so important. This knowledge lets us react quickly during a heart attack. It could save lives.
Inherited arrhythmia syndromes are genetic conditions that raise the risk of cardiac arrest. They affect the heart’s electrical system, leading to dangerous arrhythmias.
It’s important to understand these genetic predispositions for early detection and management. We’ll look at Long QT Syndrome and Brugada Syndrome, and the importance of genetic testing and family screening.
Long QT Syndrome (LQTS) and Brugada Syndrome are two known inherited arrhythmia syndromes. LQTS causes a prolonged QT interval, leading to a dangerous arrhythmia called Torsades de Pointes. Brugada Syndrome is identified by a specific ECG pattern and increases the risk of ventricular fibrillation.
Both conditions are caused by genetic mutations in the heart’s ion channels. Genetic testing can identify those at risk, allowing for preventive measures and close monitoring.
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT) is another inherited condition that can cause dangerous arrhythmias, often during physical activity or stress. It’s often linked to mutations in the RYR2 gene.
Early diagnosis and treatment are key in managing CPVT. Beta-blockers are commonly used to reduce arrhythmia risk, and lifestyle changes are also recommended.
Genetic testing is vital in identifying individuals with inherited arrhythmia syndromes. If a mutation is found in a family member, relatives can be screened to see if they have the same mutation.
| Condition | Genetic Mutation | Primary Risk |
| Long QT Syndrome | KCNQ1, KCNH2 | Torsades de Pointes |
| Brugada Syndrome | SCN5A | Ventricular Fibrillation |
| CPVT | RYR2 | Ventricular Tachycardia |
Family screening is key for early detection and management of these conditions. By identifying at-risk individuals, we can provide the right care and monitoring to lower the risk of cardiac arrest.
Cardiomyopathy is a group of heart muscle disorders. It can lead to cardiac arrest. It’s a big worry for young athletes and those with heart disease in their families.
Hypertrophic cardiomyopathy (HCM) makes the heart muscle thick. This can block blood flow and cause dangerous heart rhythms. It’s a top reason for sudden death in young athletes. Early detection through genetic tests and echocardiography is key to managing HCM.
Dilated cardiomyopathy (DCM) makes the heart chambers big. This weakens the heart’s pumping power. Arrhythmogenic right ventricular cardiomyopathy (ARVC) replaces heart muscle with fat, leading to deadly heart rhythms. Both raise the risk of cardiac arrest.
Diagnosing cardiomyopathy needs genetic tests, imaging like echocardiography and MRI, and sometimes, invasive tests. Treatment includes medicines, lifestyle changes, and sometimes surgery or devices like ICDs.
| Type of Cardiomyopathy | Characteristics | Risk Factors | Management Strategies |
| Hypertrophic Cardiomyopathy | Thickening of heart muscle | Genetic predisposition, family history | Genetic screening, medications, lifestyle changes |
| Dilated Cardiomyopathy | Enlargement of heart chambers | Coronary artery disease, hypertension, infections | Medications, heart transplantation |
| Arrhythmogenic Right Ventricular Cardiomyopathy | Replacement of heart muscle with fatty tissue | Genetic mutations | ICDs, anti-arrhythmic medications, lifestyle modifications |
Knowing about cardiomyopathy and how to manage it is vital. It helps prevent cardiac arrest and improves patient care. By spotting risk factors and using the right treatments, we can lower cardiac arrest rates from cardiomyopathy.
Electrolytes like potassium, calcium, and magnesium are key for a healthy heart. They help control the heartbeat and make sure the heart muscles work right.
When these electrolytes are off balance, the heart can struggle. For example, potassium is vital for a steady heartbeat. Too much or too little potassium can cause serious heart rhythm problems.
Calcium is also important for the heart. It helps the heart muscles contract. If calcium levels are not right, the heart can’t work well and may have arrhythmias.
Magnesium helps keep potassium and calcium in balance in the heart. Without enough magnesium, the heart can have arrhythmias and other problems.
| Electrolyte | Normal Function | Abnormality Effects on Heart |
| Potassium | Regulates heart rhythm | Hyperkalemia: Arrhythmias, cardiac arrest; Hypokalemia: Arrhythmias, muscle weakness |
| Calcium | Involved in cardiac muscle contraction | Hypercalcemia: Arrhythmias, cardiac arrest; Hypocalcemia: Impaired contraction, arrhythmias |
| Magnesium | Regulates potassium and calcium balance | Hypomagnesemia: Arrhythmias, exacerbates other electrolyte imbalances |
Many health issues can lead to electrolyte imbalances that harm the heart. For instance, kidney disease can cause too much potassium, leading to serious heart problems. Gastrointestinal disorders can also lead to a loss of important electrolytes.
Other problems, like hormonal imbalances or certain medicines, can mess with electrolyte levels. Knowing about these issues is key to avoiding heart problems caused by electrolyte imbalances.
Certain substances, whether prescribed or illicit, can harm the heart, leading to cardiac arrest. The link between substance use and cardiac arrest is complex. It involves many mechanisms that can disrupt normal heart function.
Some prescription drugs, meant to treat health issues, can increase the risk of cardiac arrest. Antiarrhythmic drugs can sometimes cause arrhythmias, a phenomenon known as proarrhythmia. Other medications, like certain antidepressants and antipsychotics, can also prolong the QT interval. This is a risk factor for a type of irregular heartbeat known as Torsades de Pointes.
It’s important for patients to follow their medication dosage. They should also tell their healthcare providers about any other medications or substances they are using. This helps avoid harmful interactions.
Illicit drugs, including cocaine, amphetamines, and synthetic cathinones, can have significant cardiac effects. These substances can cause coronary artery vasoconstriction, hypertension, and increased myocardial oxygen demand. All these can contribute to cardiac ischemia or infarction.
The use of illicit drugs can also lead to cardiomyopathy and arrhythmias. This further increases the risk of cardiac arrest.
Alcohol consumption, mainly binge drinking, can lead to cardiac arrhythmias. This condition is known as “holiday heart syndrome.” Chronic alcohol abuse can result in alcoholic cardiomyopathy. This further increases the risk of cardiac arrest.
Stimulants, including energy drinks and certain medications, can also cause cardiac events. These include arrhythmias and cardiac arrest, often when combined with other substances.
Understanding the risks of substance use is key to preventing cardiac arrest. We must be aware of the cardiac effects of both prescription medications and illicit substances. We also need to know the dangers of excessive alcohol consumption.
It’s important to know about physical and environmental triggers to prevent cardiac arrest. Many external factors can cause cardiac arrest. Knowing these can help us take steps to prevent it.
Physical trauma, drowning, and respiratory failure are big triggers for cardiac arrest. Trauma can hurt the heart or cause severe blood loss. Drowning leads to cardiac arrest due to lack of oxygen. Respiratory failure, from diseases like COPD or pneumonia, can also cause cardiac arrest if not treated right.
Some important factors include:
Extreme temperatures, hot or cold, can also trigger cardiac arrest. Hypothermia and hyperthermia can disrupt the heart’s function. Electrical injuries, from lightning or accidents, can also disrupt the heart’s electrical activity.
Important things to consider are:
Commotio cordis happens when a chest blow, often in sports, messes with the heart’s function. This is a big worry in sports like baseball, hockey, and football. Chest impacts can happen from projectiles or collisions.
To prevent it, we should wear protective gear and have emergency plans at sports events.
It’s important to know how cardiac arrest risks change with age. This knowledge helps in preventing and treating it. As we get older, our risk for cardiac arrest grows due to genetics, environment, and lifestyle.
Children and teens often face cardiac arrest due to heart defects, inherited conditions, or accidents. For example, hypertrophic cardiomyopathy is a risk for young athletes.
Young adults are at risk due to inherited heart problems, drug use, and injuries. Being very active without checking your heart health also increases the risk.
Middle-aged people are more at risk for cardiac arrest. This is because of heart disease, high blood pressure, and other heart risks. Bad lifestyle choices, like smoking and not exercising, make these risks worse.
Older adults face the highest risk of cardiac arrest. This is because of heart disease, heart failure, and other health issues that get worse with age. Their heart function also declines with age.
Knowing these age-specific risks is key to preventing cardiac arrest. Here’s a table that summarizes the main risks by age:
| Age Group | Primary Risk Factors |
| Children and Adolescents | Congenital heart defects, inherited conditions, trauma |
| Young Adults | Inherited arrhythmia syndromes, substance abuse, trauma |
| Middle-Aged Adults | Coronary artery disease, hypertension, lifestyle factors |
| Older Adults | Coronary artery disease, heart failure, comorbid conditions, age-related decline |
By knowing these risks, we can all take steps to lower our chances of cardiac arrest. This includes making healthy choices and being ready for emergencies.
Knowing what causes cardiac arrest is key to preventing it. By making smart lifestyle choices and managing health issues, you can lower your risk. This can help you avoid cardiac arrest.
Keeping your heart healthy means staying active, eating right, and avoiding bad habits. It’s also important to manage conditions like high blood pressure, diabetes, and high cholesterol. Knowing the signs of cardiac arrest, like chest pain and shortness of breath, helps you get help fast.
If you have a family history of heart problems or other risk factors, see your doctor often. Taking care of your heart can reduce your risk of cardiac arrest. This improves your overall health and well-being.
By focusing on preventing cardiac arrest and living a heart-healthy lifestyle, we can make our community healthier. This effort can help lower the number of cardiac arrests.
Cardiac arrest happens when the heart suddenly stops working. This is often due to an electrical problem. A heart attack, on the other hand, is caused by a blockage in the heart’s blood vessels. This blockage damages the heart muscle.
The main causes include coronary artery disease and heart attacks. Other causes are inherited heart rhythm problems, heart muscle diseases, and imbalances in body salts. Substance use and physical or environmental factors also play a role.
Coronary artery disease can cause cardiac arrest. This is because plaque builds up in the arteries. This buildup can lead to a heart attack or abnormal heart rhythms, which can cause cardiac arrest.
Inherited heart rhythm problems, like long QT syndrome, can increase the risk of cardiac arrest. These problems can cause abnormal heart rhythms.
Yes, big changes in body salts like potassium, calcium, and magnesium can mess with the heart. This can lead to cardiac arrest.
Certain drugs and alcohol can affect the heart in ways that might lead to cardiac arrest. This includes prescription drugs and illegal substances.
Physical and environmental factors can trigger cardiac arrest. These include trauma, drowning, and extreme temperatures. Electrical injuries and commotio cordis, linked to sports, are also risks.
Risk factors change with age. Young athletes might face risks from heart muscle diseases. Older adults are more likely to face cardiac arrest due to heart disease.
To lower the risk, make lifestyle changes and manage risk factors. Knowing warning signs and how to act in an emergency is also key.
Quick action, like CPR and defibrillation, is vital. It helps save lives and reduces damage during a cardiac arrest.
Genetic testing can spot those at risk. This allows for early action and management to prevent cardiac arrest.
While some cardiomyopathies can’t be prevented, managing the condition is key. Medical care and lifestyle changes can lower the risk of cardiac arrest.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!