Last Updated on November 27, 2025 by Bilal Hasdemir
Spine surgery is a big deal and usually a last choice for spinal problems. Nearly 500,000 spine surgeries are done every year in the United States. Many of these surgeries lead to complications.
We want to help patients make smart choices about their health. Thinking about spine surgery can be scary. It’s important to know the reasons to avoid spine surgery, such as risks of complications, unpredictable results, and long recovery times, and to determine if these risks outweigh the benefits.
It’s key to understand the risks of spine surgery to make good choices about your spine. We aim to give you a fair view. This helps you think about other treatments before surgery.
Key Takeaways
- Spine surgery is a major operation with possible complications.
- Try other treatments before surgery.
- Knowing the risks helps you make better decisions.
- We’re dedicated to giving you full care and support.
- We want you to be able to make informed choices about your spine.
Understanding Spine Surgery: When Is It Typically Recommended?
Knowing why spine surgery is suggested can help patients choose the right treatment. It’s a big step that comes after trying other options.
Doctors recommend surgery for serious pain or nerve problems. They look at other treatments first. Then, they weigh the surgery’s benefits and risks.
Common Spinal Conditions That Lead to Surgical Recommendations
Some spinal issues might need surgery. These include:
- Herniated Discs: When the soft center leaks out, pressing on nerves.
- Spinal Stenosis: The spinal canal gets too narrow, pressing on nerves.
- Scoliosis: An abnormal spine curve that can cause pain and breathing issues.
- Spondylolisthesis: When a vertebra slips forward, irritating nerves.
These problems can really affect a person’s life. Surgery might be an option if other treatments don’t work.
The Evolution of Spine Surgery Approaches
Spine surgery has changed a lot, thanks to new tech and methods. Old open surgeries are now mostly replaced by minimally invasive procedures. These new methods aim to cut down on recovery time and damage.
The changes include:
- Minimally Invasive Surgery (MIS): Smaller cuts and less damage to tissues.
- Endoscopic Surgery: Uses an endoscope for small incisions.
- Robotic-Assisted Surgery: Adds precision and accuracy to surgeries.
These updates have helped many patients. But, it’s important to remember that each case is different. And, there’s always a chance of complications.
Key Reasons to Avoid Spine Surgery: Risks vs. Benefits

When thinking about spine surgery, it’s key to know the risks and benefits. This surgery can greatly change a patient’s life.
The decision to have spine surgery is big.Patients need to know the risks and benefits well to make a smart choice.
Statistical Overview of Spine Surgery Outcomes
Research shows that spine surgery results can vary a lot. For example, a study in the Journal of Neurosurgery: Spine found 50% to 60% of patients see big improvements for some spinal issues.
But, the same study found many patients don’t see as much improvement or face complications. This shows why it’s vital to look at each case carefully.
Risk-Benefit Analysis for Different Spinal Conditions
Each spinal problem has its own risks and benefits with surgery. For instance, surgery for herniated discs or spinal stenosis might help some, but it also has risks like infection or nerve damage.
For degenerative disc disease, surgery might be considered if other treatments don’t work. But, the decision must consider the patient’s age, health, and the condition’s details.
Elderly patients face higher risks with spine surgery because of health issues or less ability to heal. Surgical problems in older patients can be serious. It’s important to think carefully about these risks and benefits.
In summary, while spine surgery might help some, it’s not without risks. Knowing these risks and benefits well is key for making good choices.
High Failure Rates: Understanding Failed Back Surgery Syndrome
For some, spine surgery doesn’t bring the relief they hoped for. Instead, it leads to Failed Back Surgery Syndrome (FBSS). This condition causes ongoing or returning pain after surgery, greatly affecting a patient’s life quality.
Defining Failed Back Surgery Syndrome
Failed Back Surgery Syndrome is when patients keep feeling pain or symptoms after spine surgery. It’s not because the surgeon failed, but because of many factors. These include the initial problem, the surgery type, and the patient’s health.
FBSS can happen for many reasons. It might be due to poor surgery technique, not fully fixing the problem, or new issues from the surgery. Knowing these reasons helps surgeons and patients make better choices.
Statistics on Spine Surgery Failure Rates
Research shows that spine surgery failure rates vary. For example, up to 40% of patients with lumbar spine surgery might face persistent pain or FBSS.
These numbers highlight the need to think carefully about spine surgery. It’s important to consider other treatments before deciding on surgery.
Long-term Consequences of Failed Surgeries
Failed back surgery can have lasting effects. It can cause chronic pain, reduced mobility, and affect mental health. Patients might feel depressed, anxious, and have a lower quality of life due to pain and limited movement.
The economic costs of FBSS are also high. They include extra medical bills, rehabilitation, and lost work time. So, it’s key to think about these long-term effects when choosing spinal treatment.
Significant Risk of Nerve Damage and Neurological Complications
Spine surgery carries a big risk of nerve damage. This can greatly affect a patient’s life quality. The surgery involves working with delicate areas around the spinal cord and nerves. This increases the chance of injury to these important parts.
Types of Nerve Injuries During Spine Surgery
Nerve injuries during spine surgery can vary in severity and type. Some common types include:
- Neurapraxia: A temporary disruption in nerve function that usually resolves on its own.
- Nerve root injury: Damage to the nerve roots as they exit the spinal canal, potentially causing pain, numbness, or weakness.
- Spinal cord injury: The most severe form, which can result in significant and potentially permanent neurological deficits.
Neurological Complications and Their Impact on Quality of Life
Neurological complications from nerve damage during spine surgery can greatly affect a patient’s life. These complications may include chronic pain, muscle weakness, numbness, or tingling sensations. In severe cases, patients may experience paralysis or loss of bladder and bowel control. This can drastically change their daily lives and independence.
The impact on quality of life is not just physical; neurological complications can also lead to emotional and psychological distress. Patients may experience depression, anxiety, or frustration due to their changed circumstances. This highlights the need for care that addresses both physical and emotional needs.
We must carefully consider these risks when deciding on spine surgery. We need to weigh the possible benefits against the possible neurological complications. Understanding the types of nerve injuries and their long-term effects is key for making informed decisions about spinal health.
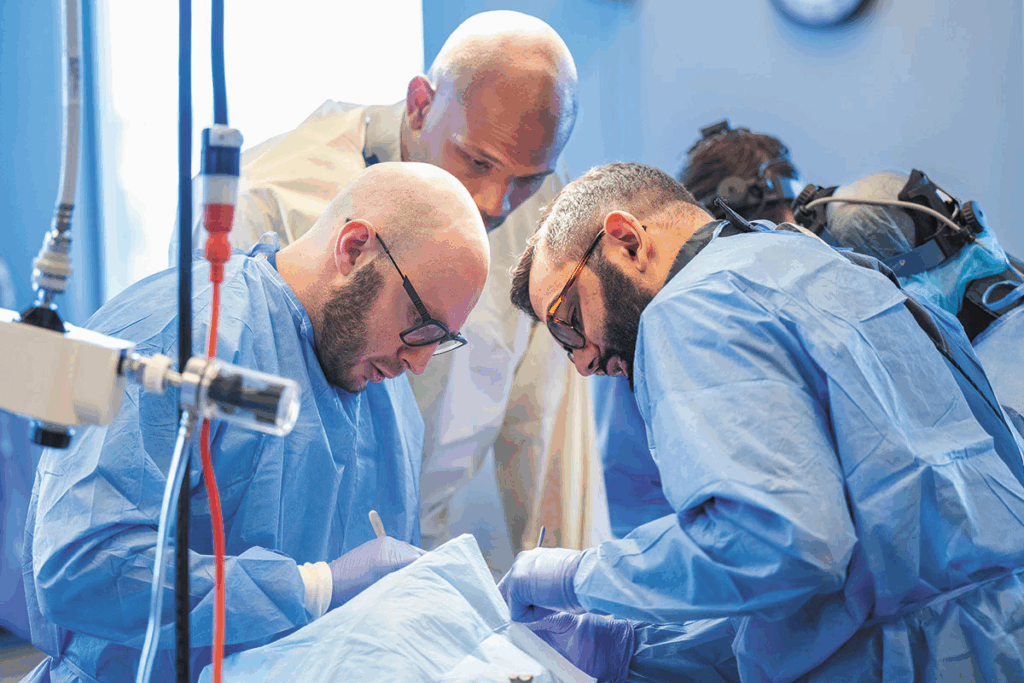
Infection Risks and Post-Surgical Complications
Infections and complications after spine surgery are serious. Patients need to know about these risks. Spine surgery can help many spinal conditions, but it comes with dangers.
Common Infections Following Spine Surgery
Surgical site infections (SSIs) are common after spine surgery. These can be skin infections or deeper ones in the vertebrae or discs. It’s important to treat SSIs quickly to avoid more problems.
Studies show SSIs rates vary. This depends on the surgery type, patient health, and how the surgery is done. Keeping the surgery area clean and following care instructions can lower infection risk.
Hardware Complications and Implant Failures
Spine surgery often uses rods, screws, and cages to support the spine. These implants help during healing but can fail. Failure might need more surgery, increasing risk and recovery time.
“The use of instrumentation in spine surgery has become more common, but it also introduces additional risks, including hardware failure and infection.”
Systemic Complications Affecting Overall Health
Spine surgery can also cause problems that affect the whole body. These include DVT, pulmonary embolism, and heart issues. People with health problems before surgery are at higher risk. This highlights the need for a detailed check before surgery.
Knowing these risks is key for those thinking about spine surgery. Being informed helps patients make better choices. It also helps them work with doctors to avoid complications.
Chronic Pain After Spine Surgery: A Common Outcome
Many patients face chronic pain after spine surgery, even when they hope for relief. Spine surgery aims to ease back pain, but some patients find their pain doesn’t go away or even gets worse.
It’s important to understand why this happens. This knowledge helps manage expectations and look for other ways to treat pain. We’ll explore the reasons behind this issue and the hurdles in managing pain after surgery.
Why Pain Often Persists or Worsens After Surgery
Several reasons can cause pain to stay or get worse after spine surgery. These include:
- Incomplete resolution of the underlying condition
- Nerve damage during surgery
- Instability or hardware failure
- Scarring and adhesions
These factors show how complex spinal conditions are and how hard surgery can be to fix them.
The Challenge of Managing Post-Surgical Pain
Dealing with chronic pain after spine surgery is tough. Patients need a mix of treatments to find relief.
| Treatment Approach | Description | Potential Benefits |
| Pain Management Medications | Use of pharmaceuticals to control pain | Reduced pain levels, improved quality of life |
| Physical Therapy | Targeted exercises to improve mobility and strength | Enhanced functional ability, reduced pain |
| Alternative Therapies | Includes acupuncture, chiropractic care, and other non-pharmacological interventions | Potential for pain reduction, improved well-being |
By knowing why chronic pain happens after spine surgery and trying different treatments, patients and doctors can improve life quality together.
The Lengthy and Challenging Recovery Process
Recovering from spine surgery is a long and tough journey. It involves both physical and emotional challenges. It’s important for patients to know what to expect during this time.
Typical Recovery Timeline for Different Spine Procedures
The time it takes to recover from spine surgery varies. A simple discectomy might need less time than a complex spinal fusion surgery.
| Procedure | Typical Recovery Time | Key Activities During Recovery |
| Discectomy | 2-6 weeks | Light walking, gradual return to daily activities |
| Spinal Fusion | 3-6 months | Physical therapy, avoiding heavy lifting, bending |
| Laminectomy | 4-8 weeks | Rest, physical therapy, improving mobility |
Physical and Emotional Challenges During Recovery
Recovering from spine surgery is not just about physical healing. It also requires emotional strength. Patients often face pain, discomfort, and frustration.
Physical Therapy is key in the recovery process. It helps patients regain strength, improve mobility, and reduce pain. A good physical therapy plan can greatly improve surgery results.
Support from family, friends, and healthcare professionals is vital. Patients should share their feelings and concerns. They should also seek help when needed.
Spinal Fusion Complications and Long-term Mobility Issues
Spinal fusion aims to stabilize the spine but can lead to mobility problems. It’s meant to ease pain and stabilize the spine. Yet, it can cause complications that impact daily life. We’ll look at the long-term effects of spinal fusion, focusing on adjacent segment disease and its impact on daily activities.
Adjacent Segment Disease and Accelerated Degeneration
Adjacent segment disease (ASD) is a major complication of spinal fusion. It happens when the segments next to the fusion site bear more stress, leading to faster wear and tear. This can cause new or worsening pain, possibly needing more surgery.
The risk factors for ASD include:
- The number of levels fused
- Pre-existing degeneration at adjacent levels
- Alterations in spinal biomechanics post-fusion
Accelerated degeneration can cause a series of problems, like herniated discs, spinal stenosis, and facet joint arthritis. It’s important for those thinking about spinal fusion to know these risks.
Impact on Range of Motion and Daily Activities
Spinal fusion surgery can greatly reduce a patient’s range of motion. By joining vertebrae, it limits flexibility in the spine. This can make everyday tasks harder, like bending, twisting, or lifting.
Some common issues patients face include:
- Difficulty with bending or twisting
- Challenges in maintaining proper posture
- Increased strain on other parts of the body to compensate for reduced spinal mobility
It’s key for patients to talk to their healthcare provider about these possible limitations. This way, they can understand how spinal fusion might change their lifestyle and plan for it.
The High Financial Cost of Spine Surgery
Knowing the true cost of spine surgery is key to making smart healthcare choices. Spine surgery is complex and often needed for many spinal issues. It comes with a big financial cost. This cost includes not just the surgery itself but also long-term care and possible complications.
Direct Medical Costs and Insurance Considerations
The direct costs of spine surgery include hospital fees, surgeon charges, and anesthesia. These costs can range from $50,000 to over $150,000. This depends on the surgery’s complexity and the patient’s health.
Insurance coverage is important in reducing these costs. But, how much coverage you get varies a lot. It’s important to know what your insurance covers, including deductibles and co-pays.
Hidden Costs: Rehabilitation, Lost Income, and Long-term Care
There are hidden costs to spine surgery too. Recovery often involves physical therapy and may need more surgeries or long-term care. These costs can add up fast, making things harder financially for patients.
Another hidden cost is lost income from time off work. Recovery can take months, leaving patients without a paycheck. This can be hard to get back.
| Cost Category | Average Cost | Notes |
| Hospital Charges | $30,000 – $100,000 | Varied based on length of stay and services |
| Surgeon Fees | $5,000 – $20,000 | Dependent on surgeon’s experience and location |
| Rehabilitation Costs | $2,000 – $10,000 | Physical therapy and other recovery expenses |
| Lost Income | Varies | Dependent on patient’s salary and recovery time |
It’s important to understand these costs to make informed decisions. By looking at both direct and hidden costs, patients can better prepare for the financial side of spine surgery.
Psychological Impact and Quality of Life Concerns
Spine surgery’s psychological impact is a big deal for both patients and doctors. It can change a person’s mental health and life quality a lot.
Depression and Anxiety Associated with Surgical Outcomes
Research shows spine surgery patients face a higher risk of depression and anxiety. The stress and doubt about surgery outcomes can make these problems worse.
Recovering from surgery is not just about the body. It’s also about the mind. Patients might feel scared, anxious, frustrated, or disappointed.
Impact on Family Dynamics and Social Relationships
Spine surgery affects family and social life too. The recovery is long and hard, needing help from family and friends.
But, the support can get tough. This is because the patient’s mood or behavior might change because of their condition or the surgery.
| Aspect | Pre-Surgery | Post-Surgery |
| Emotional State | Anxious, hopeful | Relieved, sometimes depressed |
| Family Support | High | Variable, sometimes strained |
| Social Activities | Limited due to pain | Gradually increasing |
It’s key to understand these impacts for full care. By knowing the mental and social challenges of spine surgery, doctors can help patients more.
Special Considerations for High-Risk Populations
People in high-risk groups, like older adults and athletes, face big challenges with spine surgery. They need special care and treatment plans that fit their needs.
Elderly Patients and Increased Surgical Complications
Elderly people have a higher risk of problems during spine surgery. This is because of health issues, less energy, and taking many medicines. They are at risk for infections, heart problems, and longer recovery times.
Doctors should do detailed checks before surgery to lower these risks. Improving nutrition, managing health problems, and cutting down on medicines can help. Personalized care plans that consider the patient’s health and lifestyle are key.
Athletes and Active Individuals: Career and Lifestyle Implications
Athletes and active people have their own set of challenges with spine surgery. They worry about how it will affect their career and lifestyle. They want to know when they can get back to their sport and if they’ll be as good as before.
Choosing to have surgery is a big decision for athletes. They must think about the benefits and risks. Rehab programs that match their sport can help them get back to their game.
It’s important to understand the effects of spine surgery on high-risk groups. This way, doctors can give better support and advice.
The Problem of Misdiagnosis Leading to Unnecessary Surgery
Getting a correct diagnosis is key to avoiding unnecessary surgeries in spinal health. If a diagnosis is wrong, it can lead to treatments that don’t fix the real problem. This includes surgeries that might not solve the patient’s symptoms.
Diagnosing spinal conditions can be tricky. Imaging like MRI or CT scans might not always show what’s wrong. This can cause doctors to guess wrong if they focus too much on the scans and not enough on the patient’s overall health.
When Imaging Doesn’t Match Symptoms
It’s not always easy to match what scans show with what patients feel. Some people might have big problems on scans but feel fine. Others might be in a lot of pain but scans show little. This shows how important it is to link what scans show with how patients feel and act.
- Careful Clinical Evaluation: A detailed check-up is key to finding out what’s causing a patient’s symptoms.
- Advanced Diagnostic Techniques: Using new ways to diagnose, like injections, can help find the source of pain.
The Importance of Multiple Opinions Before Surgery
Getting advice from several doctors before spine surgery is wise. It lets patients hear different views on their condition and what treatment might work best.
- Verify the Diagnosis: Getting several doctors to agree on a diagnosis can make sure surgery is really needed.
- Explore Alternative Treatments: Other doctors might suggest treatments that haven’t been considered yet.
By being thorough and careful in diagnosis and treatment planning, patients can lower the chance of wrong diagnoses leading to unnecessary surgery.
Effective Non-Surgical Alternatives for Back Pain
Back pain doesn’t have to mean surgery. There are many non-surgical treatments that work well. Many people find relief without the risks of surgery.
Physical Therapy and Rehabilitation Approaches
Physical therapy is key for back pain. It includes exercises to strengthen muscles, improve flexibility, and posture. Therapists also use heat, cold, and electrical stimulation to lessen pain and swelling.
Benefits of Physical Therapy:
- Improved strength and flexibility
- Enhanced posture and reduced strain on the back
- Pain reduction through targeted exercises and modalities
Pain Management Strategies and Interventions
Pain management is vital for treating back pain without surgery. This includes medication, injections, and other methods to reduce pain and improve life quality.
| Pain Management Strategy | Description | Benefits |
| Medication | Use of analgesics and anti-inflammatory drugs | Reduces pain and inflammation |
| Injections | Corticosteroid injections to reduce inflammation | Provides targeted relief |
| Nerve Blocks | Blocking pain signals to the brain | Effective for severe pain |
Lifestyle Modifications and Ergonomic Solutions
Changing your lifestyle can help a lot with back pain. This includes better ergonomics at work and home, staying healthy, and exercising regularly.
Ergonomic Tips:
- Ensure proper chair height and lumbar support
- Position computer monitors at eye level
- Take regular breaks to stretch and move
By trying these non-surgical options, you can manage your back pain well. This improves your life quality a lot.
Conservative Treatment Options with Proven Effectiveness
Back pain relief can often be found through non-invasive, evidence-based treatments. Surgery should be a last choice. So, it’s key to explore these alternatives first.
Conservative treatments include many therapies and interventions. They help reduce pain and improve function and quality of life. This makes them a great first step for many patients.
Evidence-Based Non-Invasive Treatments
Non-invasive treatments have strong evidence supporting their effectiveness. Physical therapy is a key part of these treatments. It focuses on exercises to strengthen the back, improve flexibility, and posture.
Pain management strategies, like medication and injections, also play a big role. They provide relief when used carefully.
Other effective treatments include:
- Chiropractic care, which improves alignment and reduces pain through spinal manipulation.
- Acupuncture, a traditional Chinese medicine technique that stimulates healing by inserting thin needles into specific points on the body.
Complementary and Alternative Medicine Approaches
Complementary and alternative medicine (CAM) offers more options for back pain relief. These include:
- Yoga and Pilates, which improve flexibility, strength, and body awareness through exercise.
- Massage therapy, which reduces muscle tension and promotes relaxation.
- Mind-body therapies, such as meditation and cognitive-behavioral therapy, which help manage chronic pain’s psychological aspects.
By combining these treatments in a care plan, patients can see big improvements. They can feel better and live better lives.
Questions to Ask Before Considering Spine Surgery
Deciding on spine surgery needs careful thought. You must understand the surgery, its results, and other treatment options. This is key during your pre-surgery talk.
Essential Questions for Your Surgeon
It’s important to ask the right questions to your surgeon. This ensures you’re well-informed. Here are some key ones:
- What are the expected outcomes of the surgery?
- What are the possible risks and complications?
- Are there other treatments or therapies that could work?
- What’s the recovery like, and how long will it take?
- How will the surgery affect my daily life and quality of life?
These questions help you grasp the surgeon’s view. They aid in making a better choice.
| Question | Purpose | Example |
| Expected Outcomes | Understand the surgery’s goals | “How will this surgery improve my condition?” |
| Potential Risks | Know possible complications | “What are the most common complications associated with this surgery?” |
| Alternative Treatments | Look into non-surgical options | “Are there any non-surgical treatments that could be as effective?” |
Red Flags in Surgical Recommendations
While most surgeons give good advice, some red flags exist. Be cautious of:
- Overly optimistic promises about surgery results without considering your situation.
- Not discussing alternative treatments or ignoring non-surgical options without thought.
- Lack of transparency about risks, complications, or the surgeon’s experience.
Knowing these red flags helps you make a better choice. It’s wise to seek a second opinion if needed.
Conclusion: Making Informed Decisions About Spine Health
It’s very important for patients to make smart choices about their spine health before surgery. We’ve looked at the good and bad sides of spine surgery. This helps patients take charge of their health.
Knowing the possible problems and long-term effects of surgery is key. Patients can then choose what’s best for them. Options like physical therapy and pain management are good alternatives to surgery.
Being in control of your spine health is the goal. We urge patients to ask questions and get different opinions. This way, they can make choices that improve their life.
FAQ
What are the main risks associated with spine surgery?
Spine surgery can lead to nerve damage and infection. It may also cause chronic pain. There’s also a risk of complications from spinal fusion, like disease in other segments. Knowing these risks helps in making informed choices.
What is Failed Back Surgery Syndrome (FBSS), and how common is it?
Failed Back Surgery Syndrome (FBSS) is when pain persists after surgery. The exact rate of FBSS varies. But it’s a big concern, showing the importance of thinking carefully before surgery.
Are there non-surgical alternatives for managing back pain?
Yes, there are many non-surgical ways to manage back pain. These include physical therapy and lifestyle changes. They can be very effective and should be considered first.
How long does recovery take after spine surgery?
Recovery from spine surgery can take a long time. It depends on the surgery type. Recovery times range from weeks to months. Patients face physical and emotional challenges during this time.
What are the financial implications of spine surgery?
Spine surgery comes with financial costs. This includes direct medical expenses and insurance issues. There are also hidden costs like rehabilitation and lost income. Understanding these costs is key for making informed decisions.
Can spine surgery lead to long-term mobility issues?
Yes, spinal fusion can cause long-term mobility problems. This includes disease in other segments and faster degeneration. It can affect patients’ movement and daily activities.
How can misdiagnosis lead to unnecessary spine surgery?
Misdiagnosis can cause unnecessary surgery. This happens when symptoms don’t match images or when diagnosis is incomplete. Getting multiple opinions is important to avoid unnecessary surgery.
What are the psychological impacts of spine surgery?
Spine surgery can deeply affect patients’ mental health. It can lead to depression and anxiety. It also impacts family and social relationships.
Are there special considerations for elderly patients undergoing spine surgery?
Yes, elderly patients face more risks with spine surgery. It’s important to weigh the benefits and risks carefully. Their overall health and recovery chances need to be considered.
What questions should I ask my surgeon before considering spine surgery?
Before spine surgery, ask your surgeon about risks and benefits. Also, ask about other treatments and recovery expectations. Knowing red flags in surgical advice is also important.
What are the benefits of conservative treatment options for back pain?
Conservative treatments, like non-invasive options and alternative medicine, can be very effective. They offer choices beyond surgery. They can help manage back pain well.
Reference
- Inoue, S. (2017). Prevalence, characteristics, and burden of failed back surgery syndrome: A nationwide internet survey in Japan. Pain Research & Management, 2017, Article ID 3581307. https://pmc.ncbi.nlm.nih.gov/articles/PMC5388346/