Last Updated on November 27, 2025 by Bilal Hasdemir
Robotic prostate surgery has changed how we treat prostate cancer. It’s a minimally invasive option compared to old methods. Today, over 80% of prostate cancer surgeries in the U.S. use robots.
Robotic-assisted prostatectomy offers many benefits, including greater precision and reduced risk of complications. The recovery time prostatectomy robotic is an important factor for patients, with most recovering faster than with traditional open surgery. Typically, patients spend one night in the hospital and can resume normal activities within 2 to 3 weeks, while full recovery including return to work and increased physical activity usually takes about 4 to 6 weeks. This quicker recovery timeline helps patients make well-informed choices about their treatment options.
We’ll dive into robotic prostate surgery. We’ll see how it stacks up against traditional methods. And what patients can expect while they recover.

Prostate surgery has changed a lot, giving patients many choices. It’s a key treatment for prostate issues like cancer. Knowing the different surgeries helps patients make better choices.
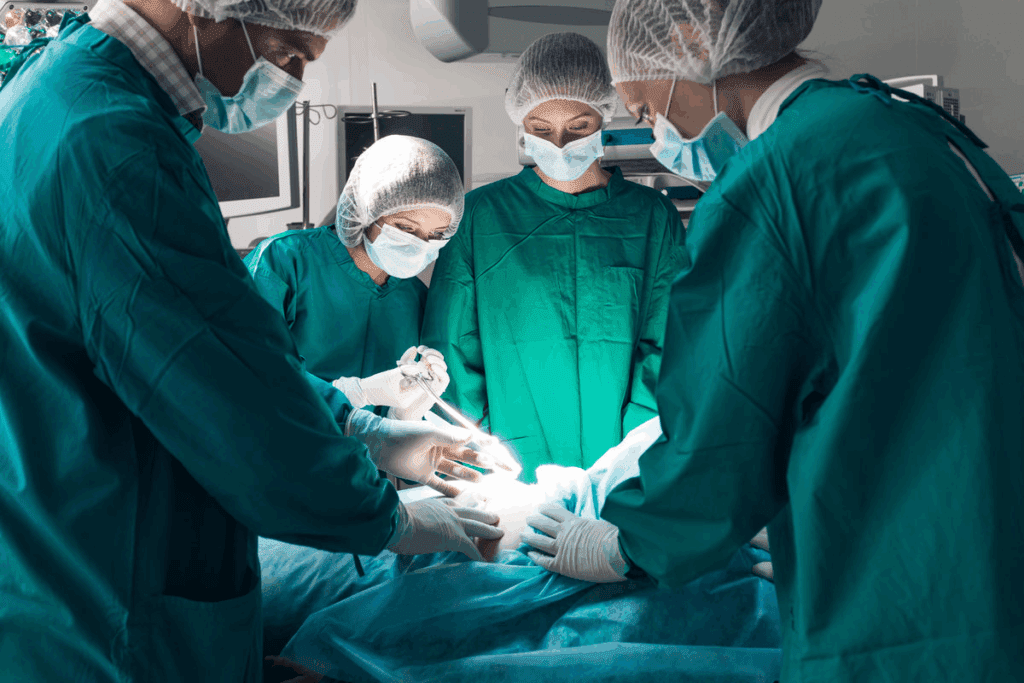
Traditional open prostatectomy uses a big cut in the belly to reach the prostate. It’s been around for a long time and works well. But it takes longer to get better than newer methods.
This surgery has a big drawback: a big cut can hurt more and keep you in the hospital longer. You might also feel more pain and take longer to get back to normal.
Laparoscopic prostatectomy uses small cuts and special tools. It’s less invasive and can be more precise. This might mean less pain and a faster recovery.
But, it’s harder to do and needs skilled surgeons. They use a camera and tools to work inside you without a big cut.
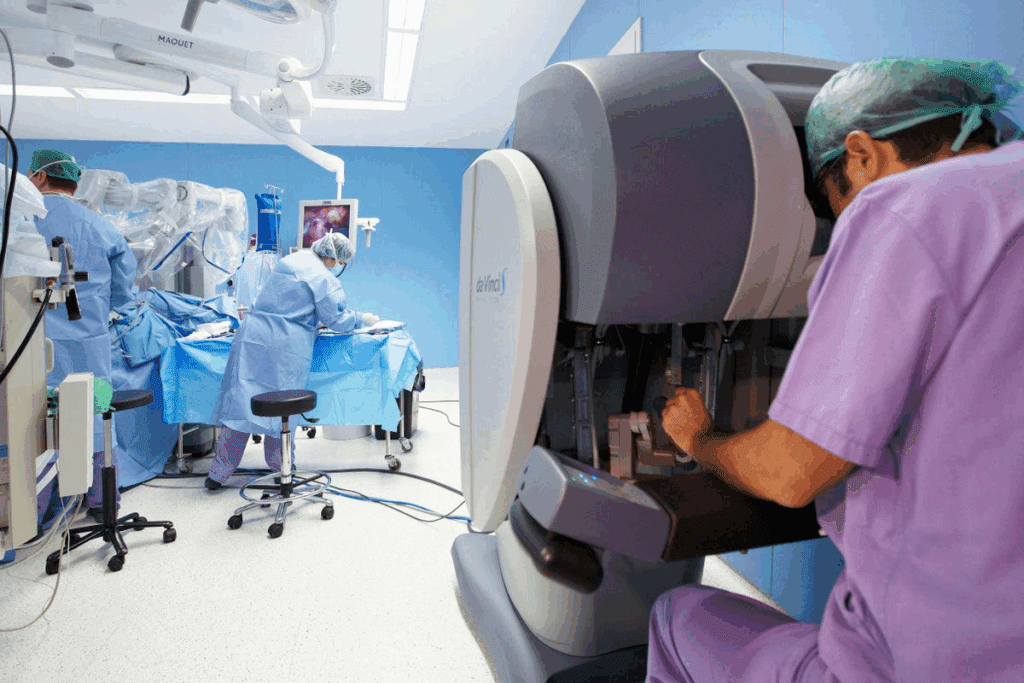
Robotic-assisted prostatectomy is the newest option. It uses a Da Vinci Surgical System for better control and vision. This system helps surgeons be more precise.
This method can lead to less pain and a quicker recovery. It also helps keep nerves and tissues safe, which can improve your quality of life.
Each surgery has its own benefits and is chosen based on the patient’s health and the surgeon’s skills. Knowing the differences helps patients make informed choices.
Robotic prostate surgery has changed a lot over the years. New technology has made surgeries better for patients. This has led to better results for those undergoing the surgery.
The Da Vinci Surgical System was a big step forward. It helps surgeons be more precise and in control. This system makes surgeries less invasive, helping patients recover faster.
Over time, the Da Vinci System has gotten even better. These updates have helped surgeons do their jobs better. They have also led to better results for patients.
New tech has been key in improving robotic prostate surgery. Today’s systems have better 3D views, more control, and are easier for surgeons to use. These changes help with more accurate surgeries and less blood loss.
Also, adding artificial intelligence and machine learning could make things even better. These tools might help surgeons do their jobs even more accurately.
In the U.S., more doctors are using robotic surgery. Hospitals are buying these systems, and more surgeons are learning how to use them.
How fast this happens depends on a few things. These include training programs, the cost of the systems, and how well they work. As more evidence comes in, we expect more doctors to start using robotic surgery.
Understanding robotic prostate surgery is key for those considering it for prostate cancer. This advanced treatment uses a robotic system to help with the surgery.
The Da Vinci Robotic System is the top choice for prostate surgery. It has a surgeon’s console, robotic arms, and a 3D vision system. The surgeon’s console gives a detailed view, allowing for exact control.
The Da Vinci System’s main parts are:
The Da Vinci System gives surgeons better control and precision. It has:
This precision helps surgeons do complex surgeries more accurately. This can lead to better results for patients.
The time for robotic prostate surgery varies. It depends on the case’s complexity and the surgeon’s experience. On average, it takes 2 to 4 hours.
The time in the operating room might be longer. This includes preparation and anesthesia. But the surgery itself usually takes 2-4 hours.
Patients have many options for prostatectomy surgery. Each method has its own benefits and drawbacks. The right choice depends on the patient’s health, cancer stage, and the surgeon’s skill.
Open prostatectomy uses one big cut in the belly to reach the prostate. Laparoscopic surgery makes small cuts for tools and a camera. Robotic surgery is a laparoscopic method that uses a robot for better control.
The robotic approach has big pluses. It offers precision and visualization that can lead to better results. The robot’s 3D view helps surgeons be more accurate and careful with nerves and tissues.
The robot helps surgeons do complex tasks more accurately. Its high-definition 3D view and precise tools make it easier to work in the pelvis’s complex area.
Research shows robotic surgery can mean less blood loss and fewer complications than open surgery. The robot’s better view and control also lowers the chance of leaving cancer behind.
Blood loss is a big worry in prostate surgery. Robotic prostatectomy tends to have less blood loss than open surgery. The robot’s exact dissection and control help here.
A study found robotic surgery had much less blood loss than open surgery. Less blood loss means fewer blood transfusions and fewer complications.
In summary, choosing the right surgery for prostatectomy depends on many things. Robotic surgery is a good choice for many because of its precision, better view, and less blood loss.
After a robotic prostatectomy, patients often wonder about their recovery. The recovery time can vary, but knowing what to expect helps ease anxiety. It also helps manage expectations.
Right after surgery, patients go to the recovery room. They are watched for a few hours. We manage pain and look for any immediate problems.
Most patients feel a bit groggy and uncomfortable. But severe pain is rare because of the robotic technique’s minimally invasive nature.
Key aspects of immediate recovery include:
The hospital stay after robotic prostatectomy varies. Most patients leave within 1 to 2 days. The exact time depends on how quickly they recover and if there are any complications.
Our team checks if a patient is ready to go home. They look at pain control, ability to urinate, and overall health.
| Day | Typical Activities | Expected Milestones |
| 1 | Rest, pain management, and initial walking | Stable vital signs, manageable pain |
| 2 | Increased mobility, removal of catheter (if applicable) | Discharge preparation, self-care assessment |
Getting back to normal after a robotic prostatectomy takes time. Most can do light activities in a few weeks. But it may take longer to fully recover.
We advise avoiding heavy lifting and strenuous exercise for at least 6 weeks after surgery.
“The robotic technique has significantly reduced my recovery time. I was back to my normal routine in no time.” – A prostatectomy patient.
Following our post-operative instructions is key to a smooth recovery. Regular check-ups help us monitor healing and address any concerns.
Knowing the recovery timeline after robotic prostatectomy is key for patients. It helps them set realistic goals and manage their recovery. The journey to full recovery has several stages, each with its own milestones.
The first 24-48 hours after surgery are very important. Patients often feel discomfort, fatigue, and some pain. They need medication to manage these feelings. Having a caregiver to help with daily tasks is also important.
In the first week, patients should rest and avoid hard activities. Most go home 1-2 days after surgery. It’s important to manage pain, eat well, and drink plenty of water.
Weeks 2-4 are when patients can start to get more active. They might feel tired and uncomfortable, but these feelings should lessen. It’s important to keep up with doctor’s appointments during this time.
Recovering from a robotic prostatectomy can take months. Patients will see big improvements in 3-6 months. It can take up to a year or more for full recovery, including getting back to normal with urination and sex.
Understanding the recovery timeline helps patients prepare for their journey. It makes the recovery process smoother and more effective.
After robotic prostate surgery, it’s key to follow proper care for a smooth recovery. The time after surgery is very important. Good care can greatly affect your recovery time.
Catheter management is a big part of care right after surgery. A catheter helps with urination. It’s important to follow your doctor’s advice on how to care for it. This helps avoid infections and ensures it’s removed when needed, usually in a couple of weeks.
Wound care is also very important. Even though robotic surgery makes smaller cuts, it’s important to keep the area clean. Watch for signs of infection like redness, swelling, or discharge.
Going to follow-up appointments is key. These visits help check on your healing and address any issues. They also let your doctor remove any remaining stitches and check how you’re doing with urination and sex.
Medication management is another important part. You’ll get meds for pain, infection prevention, and other symptoms. It’s important to take your meds as directed and tell your doctor about any side effects.
By focusing on these care aspects, patients can improve their recovery after robotic prostate surgery. This can help avoid complications and make life better overall.
Understanding and managing side effects after robotic prostatectomy can greatly improve patient outcomes. Patients may face certain side effects that can affect their quality of life. We will discuss how to manage these side effects for a smoother recovery.
Urinary incontinence is a common side effect after robotic prostatectomy. Pelvic floor exercises, also known as Kegel exercises, can strengthen the muscles that control urination. We suggest starting these exercises a few weeks before surgery and continuing afterward.
As one patient reported, “Doing Kegel exercises really helped me regain control over my bladder much faster than I expected.” This proactive approach can significantly reduce the duration of urinary incontinence.
Erectile dysfunction (ED) is another possible side effect after robotic prostatectomy. Fortunately, there are effective ways to manage ED and maintain sexual health. Nerve-sparing techniques during surgery can help preserve erectile function.
| Strategy | Description |
| Nerve-Sparing Surgery | Preserves the nerves around the prostate that control erection. |
| Medication | Phosphodiesterase type 5 inhibitors (e.g., sildenafil) can help manage ED. |
| Penile Rehabilitation | A program that includes medication and devices to aid in recovery. |
According to a study published in a leading urology journal, “Nerve-sparing robotic prostatectomy significantly improves the chances of recovering erectile function.” Early intervention with medication and other therapies can enhance recovery.
Pain after robotic prostatectomy is managed with a mix of medications and other strategies. We use a multimodal approach to pain management to minimize discomfort and reduce the risk of complications.
“Effective pain management is key to recovery. We tailor our approach to each patient’s needs, using a combination of opioids and non-opioid medications, as well as alternative methods like nerve blocks.”
The goal is to keep pain under control while minimizing the use of opioids. Other strategies include:
By understanding and proactively managing these common side effects, patients can improve their recovery experience and outcomes after robotic prostatectomy.
Recovering well from prostatectomy means taking care of your diet, staying active, and looking after your mental health. We’ll share key tips and practices to help you heal smoothly and successfully.
Eating right is key after prostatectomy. Eat foods full of nutrients like fruits, veggies, whole grains, and lean proteins. Drinking plenty of water is also important. Try to drink at least eight glasses a day to help your body heal.
Nutritional Tips:
Starting with gentle exercises can help a lot. Begin with short walks and slowly increase the time and effort. Avoid heavy lifting and hard activities early on.
Activity Guidelines:
Keeping your mind healthy is just as important as keeping your body. Stay close to loved ones, do things you love, and seek help if you need it.
Tips for Mental Well-being:
Knowing when to call your doctor is important. If you have severe pain, heavy bleeding, or signs of infection, reach out right away.
| Symptom | Action |
| Severe pain not managed with medication | Contact your doctor immediately |
| Heavy bleeding or clots | Seek emergency care |
| Signs of infection (fever, chills, redness) | Contact your doctor |
By following these tips and practices, you can improve your recovery and get back to your normal life with confidence.
Exercises after prostatectomy are key to getting strong again and controlling urine better. They help the body heal faster and let patients get back to their daily lives sooner.
Strengthening the pelvic floor muscles is vital after prostate surgery. These muscles help keep the bladder and urethra in place. Kegel exercises are a great way to make these muscles stronger.
Slowly getting back into physical activities is important for a full recovery. This helps improve heart health, strength, and flexibility. Walking is a good start because it’s easy on the body and can be done slowly.
| Activity | Initial Duration | Progression |
| Walking | 10-15 minutes | Increase by 5 minutes every 2 days |
| Light Stretching | 5-10 minutes | Add new stretches every 3 days |
Getting help from a physical therapist can make a big difference. They can create a workout plan just for you. This ensures you’re doing exercises safely and effectively.
Working with a physical therapist offers many benefits:
Thanks to new surgical techniques, prostatectomy patients are seeing better results. Minimally invasive surgeries, like robotic prostatectomy, offer many advantages. These benefits make recovery smoother and faster.
Minimally invasive prostatectomy means less scarring and tissue damage. Unlike old-school open surgery, robotic-assisted methods use smaller cuts. This leads to less pain and fewer complications after surgery.
Robotic prostatectomy speeds up recovery. It causes less tissue damage and offers a more precise surgery. This means patients can leave the hospital sooner and get back to their lives faster.
Patients can move around more easily after a minimally invasive prostatectomy. Smaller cuts and less damage mean less pain. This helps prevent complications and speeds up getting back to normal.
When it comes to prostatectomy, knowing the differences between robotic and traditional surgery is key. The choice of surgery affects recovery, cancer control, and quality of life.
Both robotic and traditional prostatectomies have high cancer control rates. Robotic surgery might offer better results in some cases. Robotic prostatectomy has been linked to lower positive surgical margins, which is key for cancer control.
A study in a top medical journal found robotic-assisted laparoscopic prostatectomy is a top choice. It offers better cancer outcomes and less harm.
“The da Vinci Surgical System has changed urologic surgery. It lets surgeons do complex tasks with more precision and less harm.”
Quality of life after prostatectomy is a big deal for patients. Robotic surgery is less invasive, leading to less damage and quicker healing. Patients often feel less pain and have fewer problems, making it easier to get back to normal.
Patient happiness is linked to their surgery experience and results. Robotic prostatectomy is often preferred because it’s less invasive and leads to quicker recovery. Surveys show patients are happier with robotic surgery because of less pain and fewer issues.
The data shows robotic prostatectomy has many benefits over traditional surgery. These include better cancer control, survival rates, quality of life, and patient satisfaction. As technology advances, understanding these differences will be vital for patients and doctors.
Choosing the right surgeon for robotic prostatectomy is key. It affects your surgery and recovery. Look at several important factors for a good outcome.
A surgeon’s experience and certification matter a lot. Find a surgeon certified by a trusted board, like the American Board of Urology. They should have lots of experience with robotic prostatectomies.
Ask about their complication rates and how they handle problems. This shows their skill and readiness.
When talking to a surgeon, ask the right questions. Ask about their experience with robotic systems and their approach to surgery. Also, ask about recovery.
The hospital’s facilities and support services matter too. Choose a hospital with top-notch robotic technology and a great post-op care team. Ask about physical therapy, counseling, and nutrition help.
Also, check the hospital’s infection control and patient satisfaction. A hospital focused on care and safety helps with a smoother recovery.
By looking at these factors and asking the right questions, you can choose wisely. This careful choice can lead to a great outcome and a smooth recovery.
Robotic prostate surgery is a cutting-edge method that brings many advantages over traditional surgery. It uses systems like the Da Vinci Surgical System. This leads to more precise surgery, less blood loss, and less damage to tissues.
This results in a quicker and more comfortable recovery for patients. The robotic prostate surgery approach allows for a more detailed and nuanced operation. This can lead to better cancer control and fewer side effects.
The recovery time for robotic prostatectomy is generally shorter. Many patients can return to their normal activities within a few weeks. Whether robotic prostate surgery is “better” depends on individual patient needs and circumstances.
We recommend that patients consult with their healthcare providers. They should determine the most appropriate surgical approach based on their specific condition and medical history.
Robotic prostate surgery, also known as robotic-assisted prostatectomy, is a new way to remove the prostate. It uses the Da Vinci Surgical System for better control. This method is less invasive, leading to less blood loss, smaller scars, and a quicker recovery.
Robotic prostate surgery usually lasts from 2 to 4 hours. This time can vary based on the case’s complexity and the surgeon’s skill.
Recovery from robotic prostatectomy can take 2 to 4 weeks for most people. It may take several months to fully recover, including regaining urinary control and sexual function.
Robotic-assisted prostatectomy has many benefits. It leads to less blood loss, less pain, and shorter hospital stays. It also allows for a quicker return to daily activities. Plus, it offers better precision and visualization, which can improve cancer control and reduce complications.
Managing side effects after robotic prostatectomy involves lifestyle changes and exercises. For urinary incontinence, pelvic floor exercises are recommended. For erectile dysfunction, treatments may include medication or lifestyle changes, as advised by a healthcare provider.
When choosing a surgeon, consider their experience and certification in robotic surgery. Look at their prostatectomy outcomes and the hospital’s quality. Ask about their approach, complication rates, and postoperative care.
Minimally invasive prostatectomy recovery, like robotic prostatectomy, has many benefits. It results in less scarring, less tissue damage, shorter hospital stays, and a quicker return to daily activities. These advantages make the recovery smoother and more comfortable.
To aid in recovery, follow guidelines on nutrition and hydration. Engage in physical activities and pelvic floor exercises. Maintain mental health through stress management. It’s also important to follow the surgeon’s postoperative care instructions and attend follow-up appointments.
Long-term outcomes for robotic prostatectomy are generally good. Studies show it has similar cancer control and survival rates as traditional methods. It may also improve quality of life, including better urinary and sexual function. But results can vary from person to person.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!