Last Updated on November 25, 2025 by Ugurkan Demir
After a radical cystectomy, many patients are curious about how they will urinate. The good news is that there are several options to help manage this change. Our team is dedicated to supporting you through this transition. We provide the care and guidance you need to adapt to your new circumstances. After removal of bladder operation, how do patients urinate? We explain urinary diversion procedures like neobladder and conduits.
Understanding Radical Cystectomy
Radical cystectomy is a complex surgery. It involves removing the bladder. This is often done to treat bladder cancer that hasn’t responded to other treatments.
Reasons for the Procedure
The main reason for this surgery is to remove cancer cells from the bladder. This helps stop the cancer from spreading.
Patients should get ready for a long recovery. They will need to manage their urinary diversion or ostomy during this time.
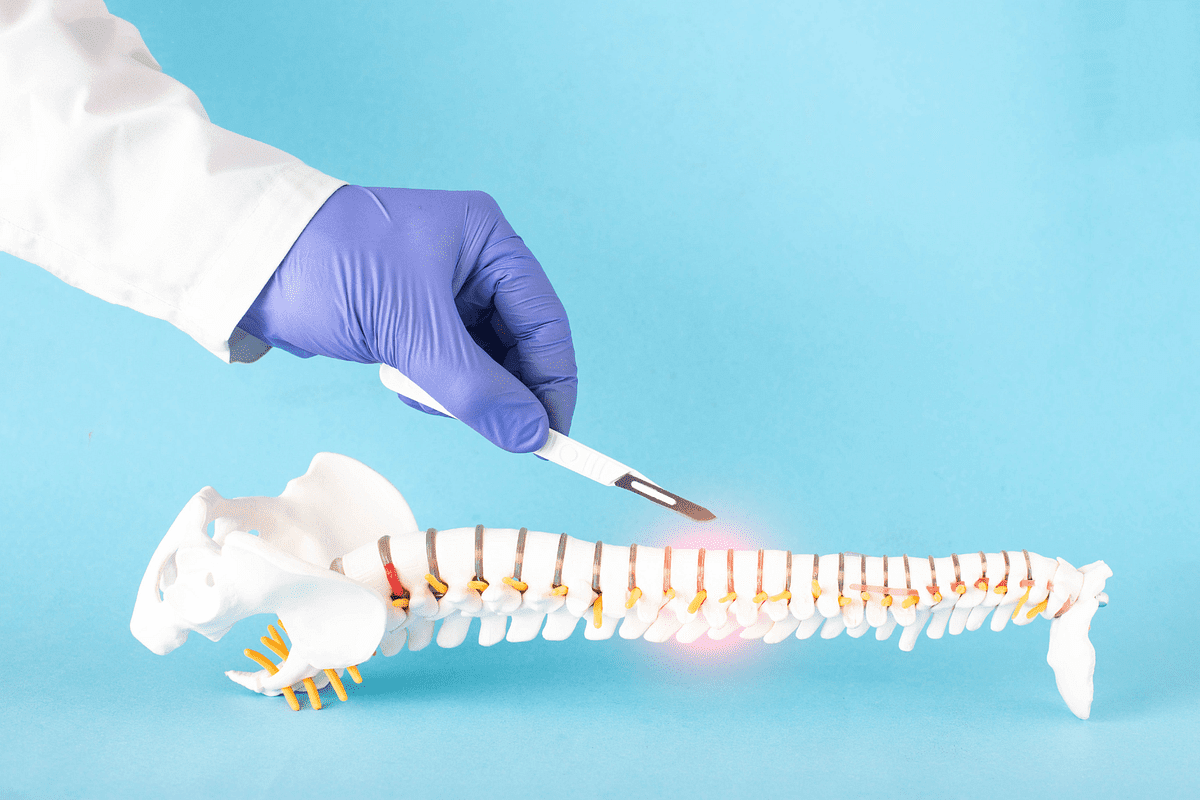
The Removal of Bladder Operation: Surgical Process

Radical cystectomy is a complex surgery that removes the bladder. It’s often done to treat bladder cancer or other bladder issues.
Preoperative Preparation
Before the surgery, patients are told to stop smoking and avoid certain medicines. They also have blood tests and imaging studies. This is to make sure they’re ready for the surgery.
The surgeon makes an incision in the abdomen to reach the bladder and nearby tissues. The bladder and affected lymph nodes are then removed.
Patients are under general anesthesia during the surgery. It usually takes several hours to finish.
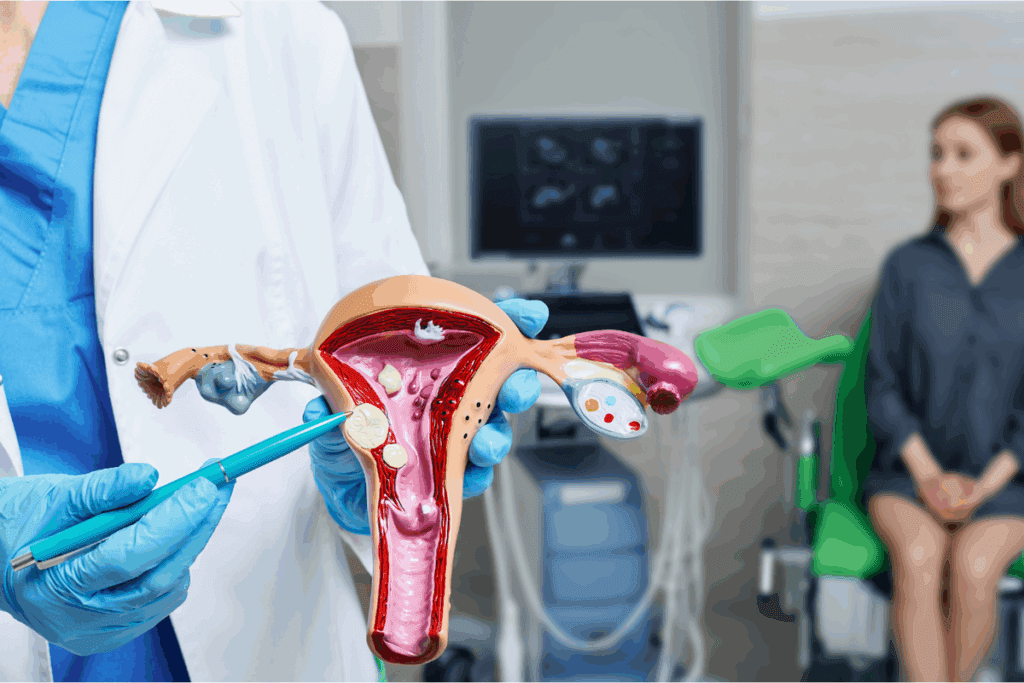
Types of Urinary Diversion Methods

After a cystectomy, patients have several options for urinary diversion. The choice of diversion method depends on various factors, including overall health and personal preferences.
Ideal Conduit
A ileal conduit is a common method. It uses a segment of intestine to divert urine from the kidneys to an external collection device.
Neobladder Reconstruction
Neobladder reconstruction creates a new bladder from a segment of intestine. This allows for more natural urination.
Continent Urinary Diversion
Continent urinary diversion involves creating a reservoir to store urine. It is then drained through a catheterizable stoma.
Each method has its benefits and drawbacks. The choice of diversion method depends on individual patient needs.
Daily Life with an Ileal Conduit
Living with an ileal conduit means making some changes. But with the right care, people can live active and happy lives. After surgery, it’s key to learn how to take care of the ostomy site and manage the appliance.
First, patients need to know how to change and clean their ostomy appliance. This includes removing the old one, cleaning the skin around the stoma with mild soap and water, and putting on a new one. It’s also important to regularly check the stoma and skin for any problems.
People should also know about possible complications like skin irritation or appliance issues. By being proactive and preventing these problems, individuals can live a normal life.
By following these guidelines and taking the necessary precautions, individuals with an ileal conduit can manage their condition well. This helps them maintain a good quality of life.
Urinating with a Neobladder
Learning to urinate with a neobladder is a skill. It involves using your abdominal pressure. This helps you to urinate effectively.
To start, you need to relax and then contract your abdominal muscles. This technique is key to using your neobladder correctly. It’s important to practice regularly to get better at it.
Self-Catheterization Techniques
After bladder removal surgery, a new way to handle urine is needed. Self-catheterization is key for this. Patients with surgical removal of the bladder due to cancer must learn this skill.
Catheter Types and Selection
There are many catheter types, each suited for different needs. Common ones include:
- Intermittent catheters, used several times a day and thrown away after each use.
- Indwelling catheters, used for longer but not for self-catheterization.
- Hydrophilic catheters, designed for comfort and less friction.
Doctors will help pick the best catheter for each patient’s situation and lifestyle.
Step-by-Step Catheterization Process
Self-catheterization involves several steps for safety and cleanliness:
- Wash your hands well with soap and water.
- Get ready the catheter and any needed supplies.
- Choose a comfortable position, sitting or standing.
- Put the catheter in the urethra or stoma until urine flows.
- Let the bladder drain fully.
- Take out the catheter and clean it as the maker says.
Hygiene and Infection Prevention
Keeping clean is key to avoid infections during self-catheterization. Patients should:
- Wash hands before and after touching the catheter.
- Clean the catheter after each use.
- Store catheters in a clean, dry spot.
Good hygiene lowers the risk of urinary tract infections, a risk after bladder removal.
Troubleshooting Common Issues
Patients might face problems like hard catheter insertion or pain. It’s important to:
- Ask healthcare providers for help with these issues.
- Keep a record of catheter use to spot patterns or problems.
Learning self-catheterization and keeping clean can help patients manage their urine after remove bladder surgery. This way, they can live well despite their surgery.
Post-Surgery Recovery Timeline
Recovery after a radical cystectomy has several stages. First, patients are watched closely in the hospital to handle any quick issues. Once they go home, they follow a care plan that includes looking after their wound and managing pain. As they get better, they will see improvements in their health and happiness.
It’s key to know about the recovery process for a good outcome. Patients must follow their doctor’s advice and keep a healthy lifestyle. This helps ensure a smooth recovery.
Lifelong Follow-up Care
After bladder removal surgery, lifelong follow-up care is key. It helps keep you healthy and catches problems early. Regular visits to your healthcare provider are essential.
Follow-up care includes regular check-ups and watching for any complications. It also means changing treatment plans if needed. This approach helps you stay healthy and live better.
Conclusion
Remember, your healthcare team is always there to support you. They will help you through every step of bladder removal surgery. Together, you can overcome challenges and improve your life quality.
FAQ
What is bladder removal surgery?
Bladder removal surgery, also known as cystectomy, is a surgical procedure to remove the bladder. It’s often performed to treat bladder cancer.
What are the types of urinary diversion methods available after bladder removal?
There are several types, including ileal conduit, neobladder reconstruction, and continent urinary reservoirs.
How do I manage my ostomy appliance after ostomy surgery?
Proper care involves regularly cleaning the stoma and appliance. Ensure a proper fit and manage any skin irritation.
What is the difference between an ileal conduit and a neobladder?
An ileal conduit involves diverting urine to a bag outside the body. A neobladder is a surgically created bladder that stores urine inside the body.
How long does it take to recover from bladder removal surgery?
Recovery times vary, but most patients can expect to spend several weeks recovering at home.
Will I need to use a catheter after bladder removal surgery?
It depends on the type of surgery and urinary diversion method used. Some patients may need to use intermittent catheterization.
How do I manage urinary incontinence after bladder removal?
Managing incontinence involves using protective garments, practicing good hygiene, and making lifestyle adjustments.
What are the risks and complications associated with bladder removal surgery?
As with any surgery, there are risks of infection, bleeding, and complications related to anesthesia.
How will bladder removal surgery affect my quality of life?
Your quality of life may be affected in various ways. But with proper care and management, many people lead active lives after surgery.
Can I still have a normal life after bladder removal surgery?
While bladder removal surgery can be life-changing, many people adapt and lead fulfilling lives with some adjustments.
How often will I need to follow up with my doctor after bladder removal surgery?
Follow-up appointments will be necessary to monitor your condition and address any complications.
Are there any dietary restrictions after bladder removal surgery?
You may need to make some dietary adjustments to manage your condition and prevent complications.
Can I still exercise after bladder removal surgery?
Yes, but you should discuss the type and intensity of exercise with your doctor to ensure it’s safe for your specific condition.
How will I know if I have a complication after bladder removal surgery?
You should be aware of the signs of possible complications, such as infection or urinary tract problems. Seek medical attention if you experience any unusual symptoms.
Can I still have a normal sex life after bladder removal surgery?
Yes, but it may require some adjustments and discussions with your partner and healthcare provider.
Are there any support groups for people who have undergone bladder removal surgery?
Yes, there are support groups and online resources available to help you cope with the emotional and practical aspects of bladder removal surgery.
References:
Radical cystectomy: a review of techniques, developments and controversies, ncbi – https://pmc.ncbi.nlm.nih.gov/articles/PMC7807330/