Last Updated on December 1, 2025 by Bilal Hasdemir
Retinoblastoma is a rare eye cancer that affects about 1 in 15,000 to 1 in 20,000 babies. It’s a big worry for kids’ health. The aggressive nature of this cancer means we need to act fast to stop it from getting worse. This is the only way to give kids the best chance of recovery.
We know how important it is to understand retinoblastoma aggressiveness assessment. This helps us give kids the care they need. This article will explain how serious retinoblastoma is. We’ll talk about how it affects kids and their families. And we’ll cover the important steps in managing this condition.
Key Takeaways
- Retinoblastoma is a rare but aggressive form of eye cancer in children.
- Early diagnosis is key to stopping the cancer from getting worse.
- Knowing how aggressive retinoblastoma is helps us manage it better.
- Treating pediatric cancer needs a complete plan.
- Families dealing with retinoblastoma need support and help during treatment.
Understanding Retinoblastoma: A Complete Overview
Retinoblastoma is a big worry in kids’ cancer care. We need to know a lot about it. This includes its traits and what it means for kids.
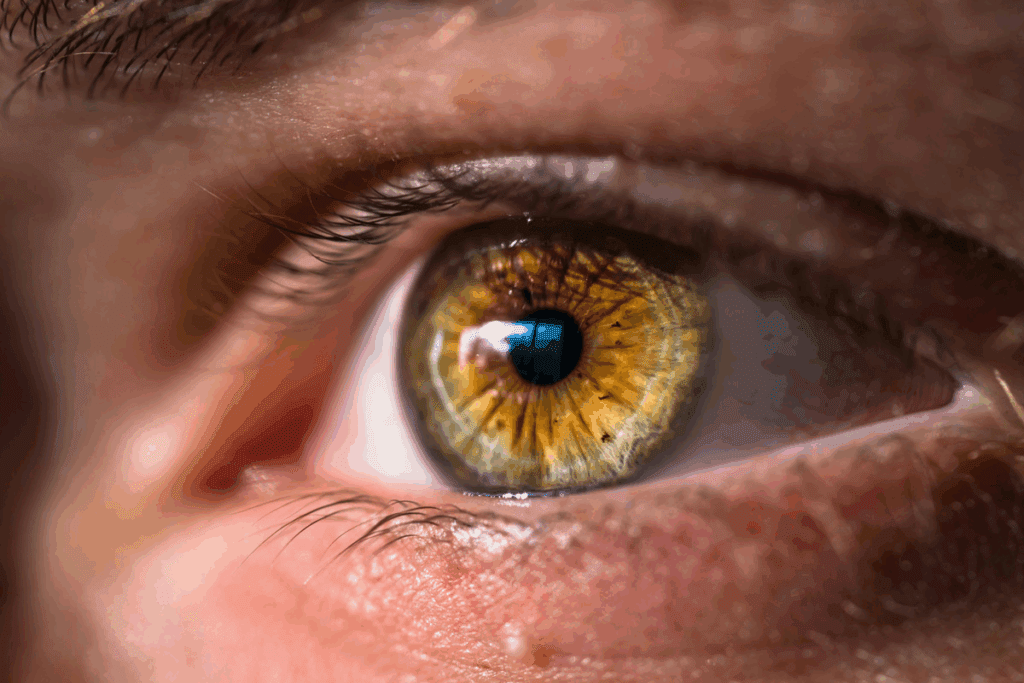
Definition and Basic Traits
Retinoblastoma is a bad tumor in the retina, the back part of the eye. It mostly hits kids under five. It happens when the RB1 gene, which controls cell growth, gets messed up.
When this happens, cells in the retina start growing too much. This forms a tumor.
Retinoblastoma can be in one eye (unilateral) or both (bilateral). Bilateral cases often run in families. Unilateral cases might be genetic or just happen by chance.
Prevalence and Demographics
Retinoblastoma is rare, making up 3% of childhood cancers. It happens in about 1 in 15,000 to 1 in 20,000 births. It’s not super common anywhere in the world.
It mostly hits kids under three. Boys and girls get it equally, so there’s no gender bias.
Types of Retinoblastoma: Unilateral vs. Bilateral
There are two main types of retinoblastoma: unilateral and bilateral. Unilateral affects one eye and is more common, making up 60-70% of cases. Bilateral affects both eyes and is linked to a genetic form of the disease.
Knowing if a child has unilateral or bilateral retinoblastoma helps doctors plan treatment. It also helps figure out the risk of the tumor spreading.
The Nature of Retinoblastoma’s Aggressiveness

Retinoblastoma is a rare eye cancer in kids. Its aggressiveness is key to understanding its severity. Knowing this helps doctors create better treatment plans and improve patient care.
Defining Aggressiveness in Pediatric Eye Tumors
Aggressiveness in retinoblastoma means the tumor grows fast, spreads, and might spread to other parts of the body. Genetic mutations, tumor size, and vitreous seeding are factors that make it aggressive. We must look at these carefully to understand the tumor’s behavior.
Studies show that certain genetic mutations affect how aggressive retinoblastoma is. For example, mutations in the RB1 gene can make tumors grow faster and spread more.
Comparing Retinoblastoma to Other Childhood Cancers
It’s important to compare retinoblastoma to other childhood cancers. Each cancer is different, and some are more aggressive. But, early treatment can greatly improve retinoblastoma outcomes.
Retinoblastoma often shows clear signs early, making it easier to catch. But, how aggressive the tumor is can change, so treatment must be customized.
Key Factors That Determine Severity
Several things determine how severe retinoblastoma is. These include the tumor’s size and where it is, if it has spread, and the patient’s age. Early treatment is key because it stops the tumor from getting too aggressive.
- Tumor size and location
- Presence of vitreous or subretinal seeding
- Extraocular extension
- Genetic mutations, like in the RB1 gene
- Age at diagnosis
Understanding these factors helps doctors create personalized treatment plans. This way, they can better meet each patient’s needs.
Cellular Behavior and Growth Patterns
The way retinoblastoma cells grow and behave is key to how the disease progresses and responds to treatment. Knowing these details helps doctors predict how severe the disease will be. It also helps them plan the best treatment.
Cancer Cell Characteristics in Retinoblastoma
Retinoblastoma cells have special traits that affect how the tumor grows. They often have a big nucleus compared to their cytoplasm. They can also form Flexner-Wintersteiner rosettes, which are signs of retinoblastoma. These rosettes show the tumor is more developed, which can guide treatment choices.
Growth Rate Analysis
The speed at which retinoblastoma grows is very important. Faster-growing tumors are more likely to spread and grow into other tissues. We track growth by looking at how the tumor changes size over time.
Research shows that chemotherapy given directly into the artery can shrink tumors in many cases. This shows how important it is to study how fast tumors grow when planning treatment. For example, a study found that this type of chemotherapy can cure retinoblastoma in about 80% of cases, without needing to remove the eye.
Tumor Doubling Time
The time it takes for a tumor to double in size is another key factor. Tumors that grow faster are more aggressive and need quick treatment. By figuring out how fast a tumor doubles, doctors can plan the best treatment.
Understanding how retinoblastoma cells grow and behave helps us predict how the disease will progress. This knowledge is vital for improving care and outcomes for patients with retinoblastoma.
Genetic Foundations of Retinoblastoma
Understanding the genetic basis of retinoblastoma is key to managing the disease. This disease is linked to mutations in the RB1 gene. This gene is a tumor suppressor that controls cell division.
The RB1 Gene Mutation
The RB1 gene mutation is central to retinoblastoma. It can happen in a hereditary or sporadic way. This affects how the disease is managed and presented.
When the RB1 gene mutates, it can’t stop tumors from forming. This leads to uncontrolled cell growth.
Hereditary vs. Sporadic Forms
Retinoblastoma can be hereditary or sporadic, each with its own genetic traits. Hereditary retinoblastoma has a germline mutation in the RB1 gene. This means the mutation is in every cell and can be passed to children.
Sporadic retinoblastoma, by contrast, has somatic mutations in the RB1 gene. These mutations happen in specific retinal cells.
Genetic Mutation Impact on Tumor Behavior
The type of RB1 gene mutation affects the tumor’s behavior. This includes how aggressive it is and its chance of spreading. Knowing this is vital for creating a treatment plan that fits the patient’s needs.
| Genetic Form | Characteristics | Implications |
| Hereditary | Germline RB1 mutation, bilateral disease common | Higher risk of secondary cancers, genetic counseling recommended |
| Sporadic | Somatic RB1 mutation, often unilateral | Lower risk of secondary cancers, but genetic evaluation is needed |
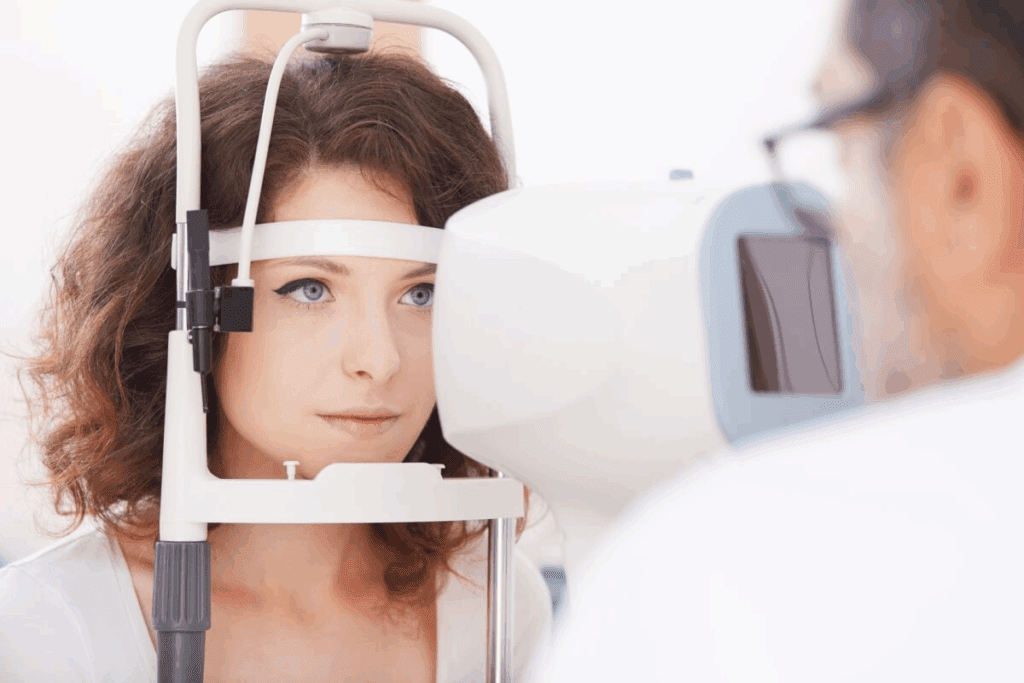
Retinoblastoma Aggressiveness Assessment: Clinical Methods
Doctors use many tools to figure out how aggressive retinoblastoma is. This helps them decide the best treatment. Assessing retinoblastoma’s aggressiveness is complex. It involves different clinical methods to understand the disease’s severity.
Diagnostic Imaging Techniques
Imaging is key in checking how aggressive retinoblastoma is. Tools like ultrasound biomicroscopy (UBM), optical coherence tomography (OCT), and magnetic resonance imaging (MRI) give detailed info.
These tools help doctors accurately stage the disease. For example, OCT shows the retina in high detail. This helps spot small changes in the tumor.
Histopathological Evaluation
Looking at the tumor under a microscope is vital. After removing the eye, doctors check the tumor’s size, how it looks, and if it’s spreading. This info is key to knowing if the tumor might spread or come back.
By studying the tumor, doctors can see if it’s high-risk. This helps them create a treatment plan that fits the patient’s needs.
Molecular and Genetic Testing
Testing the genes of the tumor is also important. It shows how the tumor might act and how it might react to treatment. This testing can also find people at risk of getting retinoblastoma early.
Genetic tests help find specific mutations that affect treatment. This is important for making treatments that work better for each patient.
Clinical Staging Systems
There are systems to classify retinoblastoma based on how bad it is. The International Classification and the American Joint Committee on Cancer (AJCC) staging system help standardize this. These systems help doctors decide the best treatment and compare results.
Doctors use these systems to sort patients by risk. This ensures each patient gets the right care for their disease.
Invasion and Spread Mechanisms
Understanding how retinoblastoma spreads is key to better treatments. This cancer’s growth depends on its ability to spread locally and to other parts of the eye or body.
Local Invasion Patterns
Retinoblastoma grows into nearby eye structures. Local invasion can move in different directions, based on where the tumor starts. It can spread into the vitreous humor or the subretinal space, causing detachment.
The tumor’s environment helps it grow. Angiogenesis and growth factors are important for this invasion.
Optic Nerve Involvement
The optic nerve is a key path for tumor spread. When the tumor reaches the optic nerve, it can move to the brain. This is linked to a worse prognosis.
How much of the optic nerve is involved matters a lot. Knowing this helps doctors plan the best treatment.
Choroidal and Scleral Invasion
Choroidal invasion is a major way retinoblastoma spreads. The choroid is a blood-rich layer between the sclera and retina. Its invasion can spread through the blood. Scleral invasion is less common but also raises the risk of spreading.
When the tumor reaches the choroid or sclera, treatment gets more intense. It often includes chemotherapy, radiation, and local treatments.
Anterior Chamber Involvement
The anterior chamber involvement is rare but serious. Tumors can reach it through the iris or the trabecular meshwork.
This can cause neovascular glaucoma. Quick and effective treatment is needed to avoid vision loss and other issues.
Metastatic Potentail and Pathways
Knowing how retinoblastoma spreads is key to treating it well. This cancer of the retina mainly hits young kids. It’s a big worry because it can spread to other parts of the body, making treatment harder and changing how well a patient does.
Common Sites of Metastasis
Retinoblastoma can spread to places like the brain, bones, bone marrow, and lymph nodes. The brain is a big worry because it’s close to where the cancer starts. Treating cancer in the brain is tough.
“The spread of retinoblastoma to the CNS represents a significant and potentially life-threatening complication,” as noted by experts in pediatric oncology.
“Early detection and aggressive treatment are key to managing CNS metastasis.”
Lymphatic vs. Hematogenous Spread
Retinoblastoma can spread through blood or lymph. Blood spread is more common and can send cancer far away. Lymph spread is less common but can happen if the tumor grows into nearby tissues.
It’s important to think about both ways cancer can spread. Hematogenous spread often means a worse outlook. So, finding cancer early and acting fast is very important.
CNS Involvement Risk
The risk of cancer reaching the brain is a big worry. Tumors that grow into the optic nerve or have certain genes are more likely to spread to the brain. Watching closely and using advanced scans are key to catching brain involvement early.
Trilateral Retinoblastoma Phenomenon
Trilateral retinoblastoma is when both eyes have cancer and there’s also a brain tumor. This is rare but serious. People with a family history of retinoblastoma are more likely to get this. So, they need to be watched closely.
In short, knowing how retinoblastoma spreads and where it goes is critical for treating it well. By understanding where cancer can go, how it spreads, and the risks of brain involvement, we can treat each patient better.
Staging and Classification Systems
Accurate staging and classification of retinoblastoma are key for choosing the right treatment. Many systems help categorize the disease by its severity and spread.
International Classification of Retinoblastoma
The International Classification of Retinoblastoma is a common system. It sorts eyes into five groups (A to E) based on tumor size and spread.
| Group | Description |
| A | Small tumors away from critical structures |
| B | Larger tumors with minimal seeding |
| C | Tumors with localized vitreous or subretinal seeding |
| D | Tumors with diffuse vitreous or subretinal seeding |
| E | Advanced disease with massive seeding or tumor destruction |
American Joint Committee on Cancer (AJCC) Staging
The AJCC staging system is another key classification. It stages retinoblastoma based on tumor size, lymph node involvement, and metastasis.
According to the AJCC, retinoblastoma is staged by tumor size, location, and invasion. This info is vital for predicting outcomes and treatment plans.
Reese-Ellsworth Classification
The Reese-Ellsworth classification is an older system. It was used to predict vision outcomes in retinoblastoma eyes. Though outdated, it’s important for understanding historical treatments.
“The Reese-Ellsworth classification system was developed to predict the visual prognosis of eyes with retinoblastoma treated with radiation therapy.”
Reese and Ellsworth, 1963
Clinical Implications of Different Staging Systems
Each staging system has its own implications. The choice depends on the patient’s needs and the doctor’s preference. Knowing each system’s strengths and weaknesses is key for the best care.
The International Classification helps guide treatment and predict outcomes. The AJCC staging system provides important info on tumor extent and metastasis.
Prognostic Indicators and Risk Stratification
Understanding the signs of retinoblastoma is key for planning treatment. These signs help us guess how well a treatment will work. They also help us find out if a child needs extra care.
Age at Diagnosis
The age a child is diagnosed with retinoblastoma matters a lot. Kids diagnosed early often face a tougher fight. This is because their disease might be more advanced.
We look at the age of diagnosis to figure out the risk. Then, we choose the best treatment for each child.
Tumor Size and Location
The size and where the tumor is located are very important. Big tumors or ones near important parts like the optic nerve are harder to treat. These factors help us predict how well a child can see and decide on treatment.
Presence of Vitreous Seeding
Vitreous seeding makes treatment harder and raises the chance of the tumor coming back. When this happens, we need to change the treatment plan. Often, we have to use stronger treatments to cover all the tumor cells.
Extraocular Extension
When the tumor spreads outside the eye, it’s a big problem. This can happen in the orbit, optic nerve, or other areas. We need to act fast and strongly to treat this.
| Prognostic Indicator | Impact on Prognosis |
| Younger Age at Diagnosis | Worse prognosis due to higher likelihood of advanced disease |
| Larger Tumor Size | Increased risk of complications and poorer visual prognosis |
| Tumor Location near Critical Structures | Higher risk of complications and challenging treatment |
| Presence of Vitreous Seeding | Higher risk of recurrence, requiring more aggressive therapy |
| Extraocular Extension | Significantly worse prognosis, requiring prompt and aggressive treatment |
By knowing and checking these signs, we can sort patients by risk. Then, we can tailor treatments to fit each child’s needs. This helps improve the chances of success for kids with retinoblastoma.
Treatment Approaches Based on Aggressiveness
Knowing how aggressive retinoblastoma is helps pick the best treatment. The disease’s severity and growth rate decide the treatment’s intensity and type.
Conservative Treatments for Less Aggressive Forms
For less aggressive retinoblastoma, doctors use conservative treatments. These aim to save vision and reduce side effects. Intra-arterial chemotherapy is a top choice, delivering medicine directly to the tumor through the eye’s artery. It’s shown great promise in shrinking tumors without harming healthy tissue.
Other treatments include focal therapies like laser treatment, cryotherapy, and brachytherapy. These methods target small tumors or leftover disease after chemotherapy. They’re designed to affect only the tumor, sparing the rest of the eye.
Aggressive Treatment Protocols for High-Risk Disease
For high-risk or advanced retinoblastoma, doctors use more aggressive treatments. Systemic chemotherapy is key, often paired with other therapies to fight the disease. When tumors spread to the optic nerve or beyond, a stronger treatment plan is needed.
High-dose chemotherapy with stem cell rescue is being explored for advanced cases. It might offer a cure for severe disease.
Emerging Targeted Therapies
New research on retinoblastoma’s genetics has led to targeted therapies. These treatments target specific genetic weaknesses in tumor cells. They offer a more precise and possibly less harmful option than traditional chemotherapy.
Studies on targeted therapies like PI3K/AKT inhibitors are showing early success. This is a promising area of research.
Enucleation: When It Becomes Necessary
Even with new treatments, enucleation is sometimes needed. This is true for advanced unilateral disease or when there’s a high risk of spread. The decision to remove the eye is made with care, weighing disease control against quality of life.
Improvements in prosthetics have made enucleation outcomes better. Patients now have more cosmetic and functional options.
Pediatric-Specific Considerations in Treatment
Pediatric patients with retinoblastoma face unique challenges. Tailored treatment approaches are needed. It’s important to consider their age, developmental stage, and health.
Age-Related Treatment Modifications
Treatment for retinoblastoma changes with the child’s age. Younger patients get treatments that avoid long-term side effects. For example, chemotherapy might be used first to shrink tumors.
Older children might get treatments more like adults. The goal is to be effective while being careful about side effects.
Anesthesia Concerns in Young Children
Young children need anesthesia for treatments like EUA or intra-arterial chemotherapy. Their safety and comfort are top priorities. Anesthesiologists must know how to care for kids.
Planning is key to reduce risks from anesthesia in this age group.
Growth and Development Impact
Treatment for retinoblastoma can affect a child’s growth and development. This is true for treatments like enucleation or radiation therapy. We must think about how to prevent growth problems.
Using adjustable orbital implants can help as the child grows.
Long-term Follow-up Requirements
Children with retinoblastoma need ongoing care. This is to watch for recurrence, manage side effects, and address late effects. This care is vital for the best outcomes.
It also means teaching families about signs of complications. And why following up is so important.
By focusing on these pediatric-specific factors, we can offer better care. This improves the chances of successful treatment for children with retinoblastoma.
Monitoring Disease Progression
Tracking how retinoblastoma grows is key to managing the disease well. We use many methods to keep an eye on it. This ensures we can act quickly when needed.
Follow-up Protocols
For retinoblastoma patients, regular check-ups are vital. These include eye exams, imaging, and sometimes exams under anesthesia. How often you need to go back depends on the tumor size, how it’s responding to treatment, and other risk factors.
Key components of follow-up protocols include:
- Regular ophthalmological examinations
- Imaging studies such as ultrasound, MRI, or CT scans
- Examinations under anesthesia for young children
- Monitoring for signs of recurrence or metastasis
Imaging Surveillance Techniques
Imaging is critical for tracking the disease. Tools like ultrasound biomicroscopy, MRI, and CT scans help us see how big the tumor is. They also help spot new tumors and check if treatment is working.
| Imaging Technique | Advantages | Limitations |
| Ultrasound Biomicroscopy | High-resolution imaging of anterior segment tumors | Limited depth penetration |
| MRI | No radiation, excellent soft tissue contrast | May require sedation in young children |
| CT Scan | Quick and widely available | Involves radiation exposure |
Molecular Monitoring Approaches
Molecular monitoring looks at genetic material to find signs of disease. This includes checking for genetic changes that might mean the disease is getting worse. Liquid biopsy is one method being explored for this purpose.
Liquid biopsy lets us analyze tumor DNA in blood. This gives us insights into the tumor without needing invasive tests.
Patient Education for Symptom Recognition
It’s important to teach patients and their families about retinoblastoma signs. Spotting changes early can lead to better outcomes. This is because we can act quickly.
Key symptoms to watch for include:
- Changes in vision or eye alignment
- New onset of leukocoria (white pupillary reflex)
- Pain or redness in the eye
- Changes in the size or shape of the eye
Recurrence Patterns and Management
Understanding how retinoblastoma comes back is key to managing the disease. When retinoblastoma comes back, it can affect treatment and care. We will look at what increases the chance of it coming back, when it’s most likely to happen, how to manage it, and its emotional impact.
Risk Factors for Recurrence
Several things can make retinoblastoma more likely to come back. These include the size and location of the first tumor, if it spread into the vitreous, and how far it went into the optic nerve. Genetic mutations, like in the RB1 gene, also play a big role. Knowing these risk factors helps doctors plan better follow-up care for those at higher risk.
Timeframe for Recurrence Risk
The risk of retinoblastoma coming back changes over time. The biggest risk is in the first few years after treatment. Regular check-ups during this time are key to catching it early. We suggest a follow-up plan that includes tests and doctor visits to watch for signs of it coming back.
Management of Recurrent Disease
Dealing with retinoblastoma that comes back needs a team effort. Treatments might include chemotherapy, laser therapy, or removing the eye, based on how bad it is and where it is. Sometimes, targeted therapies are used too. The aim is to control the disease while keeping vision and quality of life good.
Psychological Impact of Recurrence
The emotional toll of retinoblastoma coming back on patients and families is huge. It can cause more anxiety, fear, and worry about the future. Psychological support is vital to help families deal with it. We stress the need for care that meets both medical and emotional needs.
Long-term Outcomes and Survival Rates
It’s important to know about long-term outcomes and survival rates for retinoblastoma patients. This knowledge helps healthcare providers and families. Thanks to new treatments, many patients now have a better chance of survival.
Survival Statistics by Stage
Survival rates for retinoblastoma depend on the disease stage at diagnosis. Patients with early-stage disease have a better chance of survival. Those with advanced stages face tougher challenges.
| Stage at Diagnosis | 5-Year Survival Rate |
| Intraocular | 95-100% |
| Extraocular | 60-80% |
| Metastatic | 30-50% |
The table shows how survival rates change with the disease stage. Early detection is key to better outcomes.
Quality of Life Considerations
Survivors of retinoblastoma often deal with vision loss and emotional challenges. It’s important to provide care that addresses these issues. This helps improve their quality of life.
The journey for survivors doesn’t stop after treatment. It’s important to support them with ongoing care and help manage late effects.
Second Primary Malignancies Risk
Patients with hereditary retinoblastoma are at higher risk for other cancers. This includes osteosarcoma and soft tissue sarcomas. Regular check-ups are vital for early detection.
Risk factors for these cancers include the genetic mutation and radiation therapy.
Global Variations in Outcomes
Outcomes for retinoblastoma vary worldwide. This is due to differences in healthcare, diagnosis, and treatment. Working together internationally can help improve outcomes globally.
By understanding these factors and collaborating, we can enhance survival rates for retinoblastoma patients worldwide.
Recent Advances in Understanding Retinoblastoma Biology
In recent years, we’ve made big strides in understanding retinoblastoma. This has brought new insights into this complex disease. Our research has covered many areas, like molecular pathways, the tumor microenvironment, epigenetic factors, and liquid biopsy.
Molecular Pathways Research
Research into molecular pathways has been key in grasping retinoblastoma’s genetic roots. We’ve found important genes and pathways that help the disease grow and spread. For example, the RB1 gene mutation is a key player in retinoblastoma, affecting how cells grow.
Key findings in molecular pathways research include:
- Identification of novel genetic mutations associated with retinoblastoma.
- Elucidation of the role of the RB1 gene in regulating cell cycle progression.
- Discovery of possible targets for treatment within these pathways.
Tumor Microenvironment Studies
The tumor microenvironment is vital in retinoblastoma’s growth and spread. Our studies aim to understand how tumor cells interact with their surroundings.
The tumor microenvironment affects retinoblastoma in several ways:
- It provides a supportive environment for tumor growth and survival.
- It secretes growth factors and cytokines that help the tumor grow.
- It can also change how the immune system reacts to the tumor.
Epigenetic Factors
Epigenetic changes are now seen as key in retinoblastoma. These changes can affect how genes are expressed without changing the DNA itself.
“Epigenetic changes, such as DNA methylation and histone modification, play a significant role in retinoblastoma by regulating gene expression and influencing tumor behavior.”
Liquid Biopsy Applications
Liquid biopsy, analyzing DNA in bodily fluids, is a new hope for diagnosing and tracking retinoblastoma.
The advantages of liquid biopsy include:
- It’s non-invasive or minimally invasive.
- It lets us track disease and treatment response in real-time.
- It might help catch recurrence early.
Conclusion: The Evolving Understanding of Retinoblastoma Aggressiveness
Our knowledge of retinoblastoma’s aggressiveness has grown a lot. This helps doctors diagnose and treat it better. We’ve looked into its genetic roots, symptoms, and treatment options.
How aggressive retinoblastoma is depends on several things. These include genetic changes, tumor size and where it is, and if it has spread into the vitreous. Finding it early and treating it right can help patients a lot.
We’re getting better at treating retinoblastoma thanks to new research. Studies on molecular pathways, the tumor environment, and liquid biopsies are promising. They could lead to even better care for patients.
Understanding retinoblastoma better helps us support families going through it. We stress the need for full care, including mental support and ongoing check-ups. This is to meet the special needs of retinoblastoma patients and their families.
FAQ
What is retinoblastoma and how aggressive is it?
Retinoblastoma is a type of eye cancer that mainly affects kids. Its severity can vary. Some cases grow slowly, while others spread quickly.
What are the key factors that determine the severity of retinoblastoma?
The size and location of the tumor matter a lot. So does the presence of cancer cells in the eye’s fluid. Genetic changes, like in the RB1 gene, also play a big role.
How is retinoblastoma aggressiveness assessed?
Doctors use imaging, lab tests, and clinical staging to check how aggressive it is. These methods help figure out how far the cancer has spread and what treatment to use.
What are the different staging systems used for retinoblastoma?
There are a few staging systems for retinoblastoma. The International Classification, the AJCC staging, and the Reese-Ellsworth classification are the main ones. Each system helps doctors decide on the best treatment.
How does the genetic mutation impact tumor behavior in retinoblastoma?
A mutation in the RB1 gene can cause uncontrolled cell growth and tumors. Kids with a hereditary form of retinoblastoma, due to a germline RB1 mutation, often have more aggressive cancer and a higher risk of it happening in both eyes.
What are the treatment approaches for retinoblastoma based on its aggressiveness?
Treatment depends on how aggressive the cancer is. For less aggressive cases, doctors might use conservative treatments. But for more aggressive cases, they might use stronger treatments like chemotherapy, radiation, or even removing the eye.
What are the pediatric-specific considerations in the treatment of retinoblastoma?
Treating retinoblastoma in kids requires special care. Doctors consider the child’s age, the need for anesthesia, and how treatment might affect growth and development. They also need to follow up closely over time.
How is disease progression monitored in retinoblastoma?
Doctors keep an eye on how the cancer is progressing through regular check-ups and imaging. They also educate patients and families on recognizing symptoms early.
What are the patterns and management of recurrence in retinoblastoma?
Retinoblastoma can come back, and some factors increase the risk. Managing recurrence involves a team effort. It’s also important to consider the emotional impact on patients and their families.
What are the long-term outcomes and survival rates for retinoblastoma patients?
Survival rates for retinoblastoma patients depend on the cancer’s stage at diagnosis. Doctors also consider quality of life and the risk of getting cancer again in the future.
What recent advances have been made in understanding retinoblastoma biology?
Scientists have made big strides in understanding retinoblastoma. They’ve studied molecular pathways, the tumor environment, and epigenetics. They’ve also explored the use of liquid biopsy. These advances have helped us better understand the disease.
What is trilateral retinoblastoma, and how does it relate to disease aggressiveness?
Trilateral retinoblastoma is a rare condition with bilateral retinoblastoma and a brain tumor, usually in the pineal gland. It’s linked to more aggressive disease and worse outcomes.
How does retinoblastoma aggressiveness impact treatment decisions?
The aggressiveness of retinoblastoma greatly affects treatment choices. More aggressive tumors need more intense treatments, like chemotherapy, radiation, and sometimes removing the eye.
Reference
- Packer, R. J., & Vezina, G. (2008). Management of and prognosis with medulloblastoma: Therapy at the crossroad. Archives of Neurology, 65(11), 1419–1424. https://pubmed.ncbi.nlm.nih.gov/19001164/