Last Updated on November 18, 2025 by Ugurkan Demir

At Liv Hospital, we know choosing between reverse shoulder arthroplasty (RSA) and total shoulder arthroplasty (TSA) is a big decision. It depends on each patient’s unique body and needs.
We focus on our patients and offer care that’s respected worldwide. This helps patients make choices that lead to better results. Knowing the benefits and considerations of each procedure is key.
RSA is often chosen when rotator cuff function is compromised. TSA is usually recommended for those with intact rotator cuffs and primary osteoarthritis. By understanding these differences, we can tailor care to meet our patients’ specific needs.
Key Takeaways
- Understanding the differences between RSA and TSA is critical for making informed decisions.
- RSA is preferred for patients with compromised rotator cuff function.
- TSA is generally best for patients with intact rotator cuffs and primary osteoarthritis.
- Liv Hospital provides cutting-edge protocols and world-class outcomes for international patients.
- Personalized care is essential for achieving the best possible outcomes.
Understanding Shoulder Arthroplasty: An Overview

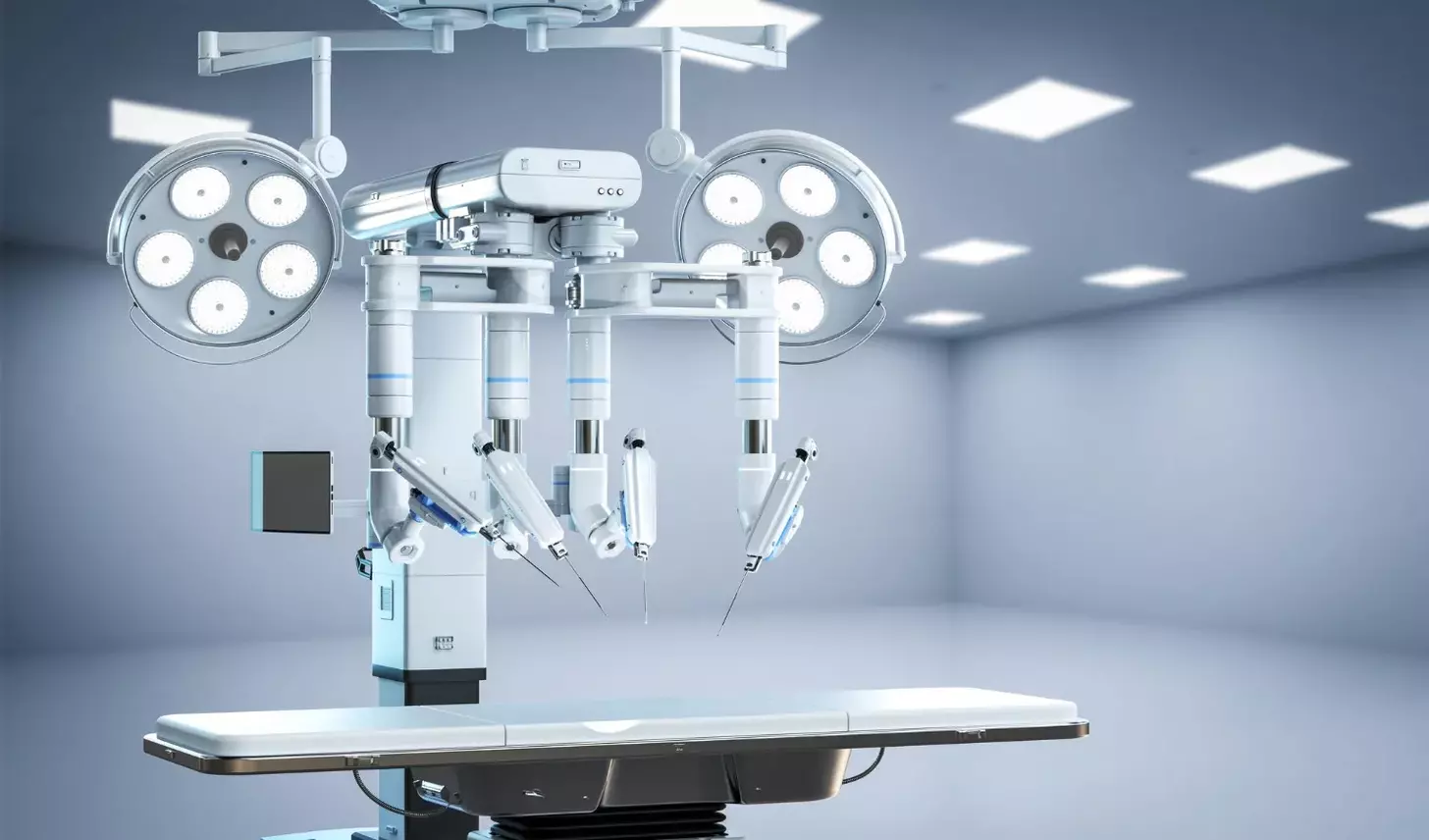
Medical technology has made shoulder arthroplasty procedures more advanced. This has brought new hope to those with shoulder problems. Shoulder arthroplasty is a surgery to replace or repair the shoulder joint. It has changed a lot over the years, focusing more on fixing function and easing pain.
The Evolution of Shoulder Replacement Surgery
Shoulder replacement surgery started in the early 20th century. Back then, technology was limited, leading to mixed results. But, with better materials and techniques, total shoulder arthroplasty (TSA) and reverse shoulder arthroplasty (RSA) have improved a lot. Now, they’re key in treating many shoulder issues, like arthritis and fractures.
Reverse shoulder arthroplasty has been a big step forward. It helps patients with damaged rotator cuffs by changing the shoulder’s anatomy. This makes it a great option for those with complex shoulder problems.
The Growing Prevalence of Shoulder Arthroplasty Procedures
More people are getting shoulder arthroplasty surgeries worldwide. This is because more people are living longer and getting shoulder problems. Studies show that the number of these surgeries has gone up over the years. It’s likely to keep going up as more people need them.
Several things are making shoulder arthroplasty more common. These include:
- More older people
- More sports injuries and accidents
- Better surgery methods and implants
- More people knowing about shoulder issues
As more people need shoulder arthroplasty, it’s key to know the differences between TSA and RSA. Understanding their uses, benefits, and risks helps us help our patients better. This way, we can offer the best treatments available.
What is Total Shoulder Arthroplasty (TSA)?

For those with severe shoulder arthritis, Total Shoulder Arthroplasty (TSA) is a good option. It replaces the damaged joint. We’ll cover the anatomy, biomechanics, and who’s a good fit for TSA. We’ll also talk about its parts and how they’re designed.
Anatomy and Biomechanics of a Traditional TSA
Total Shoulder Arthroplasty replaces the arthritic shoulder joint with a prosthetic one. It aims to restore the joint’s natural anatomy and function. This helps reduce pain and improve movement.
The shoulder joint, or glenohumeral joint, is a ball-and-socket joint. It allows for a wide range of motion. The TSA procedure resurfaces the humeral head and replaces the glenoid with a prosthetic.
The humeral component is usually made of metal, and the glenoid is made of plastic or polyethylene. Proper positioning and alignment of these components are key for success.
Ideal Candidates for Total Shoulder Arthroplasty
TSA is often recommended for those with primary glenohumeral osteoarthritis and an intact rotator cuff. It’s also suitable for those with post-traumatic arthritis, avascular necrosis of the humeral head, or inflammatory arthropathies. The decision to have TSA depends on the patient’s health, the severity of their condition, and their surgery expectations.
| Condition | Description | Ideal for TSA |
|---|---|---|
| Glenohumeral Osteoarthritis | Wear and tear of the joint cartilage | Yes |
| Post-Traumatic Arthritis | Arthritis following a traumatic injury | Yes |
| Avascular Necrosis | Death of bone tissue due to lack of blood supply | Yes |
| Inflammatory Arthropathies | Conditions like rheumatoid arthritis causing joint inflammation | Yes |
Components and Implant Design in TSA
TSA implant design has improved a lot. It focuses on durability, functionality, and better patient outcomes. The components include the humeral stem, humeral head, and glenoid component.
Modern implants are designed to match the natural anatomy of the shoulder. This allows for a more natural range of motion and reduces complications. The implant design and components are chosen based on the patient’s needs and anatomy.
What is Reverse Shoulder Arthroplasty (RSA)?
Reverse Shoulder Arthroplasty (RSA) is a new way to fix complex shoulder problems. It changes the shoulder’s structure to help those with damaged rotator cuffs or fractures. This surgery offers hope for better arm function.
The Reversed Ball-and-Socket Design
The RSA implant has a special design. The ball is on the scapula, and the socket is on the humerus. This setup lets the deltoid muscle lift the arm better, helping those with weak rotator cuffs.
This change in design makes moving the arm easier. It helps patients with damaged rotator cuffs move their arms again.
How RSA Compensates for Rotator Cuff Deficiency
RSA uses the deltoid muscle to make up for a weak rotator cuff. This helps patients move their shoulders better and feel less pain.
- The reversed design stabilizes the shoulder joint.
- It enhances the deltoid’s role in arm elevation.
- RSA reduces the reliance on the damaged rotator cuff.
Evolution of Reverse Shoulder Implant Technology
Over time, RSA implants have gotten better. Today’s implants are more durable and work better. They have new materials and are placed more carefully.
These updates have led to better results for patients. Now, RSA can help more people with shoulder issues.
Reverse Shoulder Arthroplasty vs Total Shoulder Arthroplasty: 7 Key Differences
Choosing between RSA and TSA for shoulder surgery is key for the best results. Both have changed how we treat shoulder problems. But they meet different needs and have unique features.
1. Anatomical Configuration: Natural vs. Reversed Geometry
The main difference is in how they shape the shoulder. TSA keeps the natural ball-and-socket shape. RSA flips this, with the ball on the scapula and the socket on the humerus.
2. Biomechanical Principles: Muscle Dependency Differences
How RSA and TSA work is quite different. TSA needs a strong rotator cuff to function well. RSA, on the other hand, works around rotator cuff issues by changing force directions.
3. Patient Selection: Age and Activity Considerations
Who gets which surgery matters a lot. TSA suits younger, active folks with a good rotator cuff. RSA is better for older patients or those with serious rotator cuff damage.
4. Surgical Technique: Procedural Variations
The way RSA and TSA surgeries are done also differs. RSA needs more access and special handling of the deltoid and rotator cuff.
| Characteristics | RSA | TSA |
|---|---|---|
| Anatomical Configuration | Reversed geometry | Natural ball-and-socket |
| Rotator Cuff Dependency | No | Yes |
| Typical Patient Profile | Older patients, rotator cuff damage | Younger, more active patients, intact rotator cuff |
| Surgical Complexity | More extensive exposure | Standard shoulder arthroplasty technique |
Knowing these differences helps both doctors and patients make better choices. It’s all about finding the right fit for each person’s needs.
Clinical Indications for Total Shoulder Arthroplasty
Total Shoulder Arthroplasty (TSA) is a key option for treating severe shoulder conditions. We choose TSA for patients with specific conditions that make it the best treatment.
Primary Glenohumeral Osteoarthritis
Primary glenohumeral osteoarthritis is a main reason for TSA. It damages the cartilage and bone in the shoulder, causing pain and stiffness. TSA is very effective in fixing these problems and easing pain for those who haven’t gotten better with other treatments.
Post-Traumatic Arthritis with Intact Rotator Cuff
Post-traumatic arthritis happens after a serious shoulder injury, like a fracture. If the rotator cuff is okay, TSA can help. We check the rotator cuff and arthritis level to see if TSA is right.
Avascular Necrosis of the Humeral Head
Avascular necrosis is when bone tissue dies because of blood loss. If the humeral head is badly affected, TSA might be needed. Early treatment is important to stop the problem from getting worse.
Inflammatory Arthropathies
Inflammatory arthropathies, like rheumatoid arthritis, can severely damage the shoulder. TSA is considered for those with severe damage who haven’t improved with medicine. The goal is to improve function, reduce pain, and enhance life quality.
In short, TSA is for many shoulder issues, including osteoarthritis, post-traumatic arthritis, avascular necrosis, and inflammatory diseases. Choosing the right patients and doing a detailed check before surgery are key to success.
- Primary glenohumeral osteoarthritis
- Post-traumatic arthritis with intact rotator cuff
- Avascular necrosis of the humeral head
- Inflammatory arthropathies
Knowing these reasons helps us find the right candidates for TSA. This way, we can offer the best treatment options.
Clinical Indications for Reverse Shoulder Arthroplasty
Reverse Shoulder Arthroplasty is a promising solution for those with severe shoulder problems. It’s for people who haven’t found relief with other treatments. We’ll look at why RSA is a good choice for complex shoulder issues.
Rotator Cuff Tear Arthropathy
One main reason for RSA is rotator cuff tear arthropathy. This is when the rotator cuff is badly damaged, causing arthritis. This makes the shoulder very painful and hard to move. RSA changes the shoulder’s anatomy to help with this problem.
Complex Proximal Humerus Fractures in Elderly Patients
Elderly patients with complex fractures of the upper arm bone can benefit from RSA. These fractures are hard to fix with usual methods because of the patient’s age and health. RSA makes the shoulder stable, allowing for quick recovery and rehabilitation.
Failed Previous Shoulder Arthroplasty
When a previous shoulder replacement doesn’t work, RSA can be a good option. Revision surgery is complex and needs careful planning. RSA can fix problems like loosening or mechanical failure from the failed surgery.
Massive Irreparable Rotator Cuff Tears
People with big rotator cuff tears can also get help from RSA. These tears cause a lot of shoulder pain and dysfunction. RSA changes the shoulder’s anatomy to improve function and reduce pain, making life better for the patient.
Complications and Risk Profiles
It’s key for surgeons and patients to know about the possible problems with Total Shoulder Arthroplasty (TSA) and Reverse Shoulder Arthroplasty (RSA). We need to look at the risks and how they compare.
Common Complications in Total Shoulder Arthroplasty
TSA is mostly safe but can have some issues. These include:
- Implant loosening or failure
- Infection
- Nerve damage
- Instability or dislocation
Implant loosening is a big worry, often needing a second surgery. Infection is serious and might need long antibiotic treatment or more surgery.
Common Complications in Reverse Shoulder Arthroplasty
RSA has its own set of problems, some like TSA’s, others unique because of its design. Common issues are:
- Scapular notching
- Dislocation
- Infection
- Acromial or scapular fractures
Scapular notching is a big issue with RSA, caused by the humeral component rubbing against the scapular neck.
Infection Rates and Management in Both Procedures
Infection is a big problem for both TSA and RSA.
“The management of infection in shoulder arthroplasty requires a thorough approach, including antibiotics and possibly more surgery.”
It’s vital to use strict sterile methods during surgery and watch patients closely after to lower this risk.
Choosing the right patient and doing the surgery carefully can help avoid problems. Knowing these risks helps set realistic hopes and improve results.
Rehabilitation Protocols and Recovery Expectations
Rehabilitation is key to the success of shoulder surgeries like Total Shoulder Arthroplasty (TSA) and Reverse Shoulder Arthroplasty (RSA). A good rehab plan helps patients get back to normal and recover smoothly.
Early Postoperative Care: Similarities and Differences
Right after surgery, both TSA and RSA patients need careful care. While they share some early care steps, each has its own special needs. For example, managing pain is a top priority for both, using medicine and local anesthesia.
“The early care goal is to lessen pain, reduce swelling, and start gentle movement to avoid stiffness,” say orthopedic rehab experts.
TSA Rehabilitation Timeline and Milestones
The TSA rehab plan has several phases:
- Phase 1 (0-6 weeks): Focus on pain control, gentle exercises, and isometric strength.
- Phase 2 (6-12 weeks): Start active exercises and strengthening.
- Phase 3 (3-6 months): Emphasize advanced strength and functional activities.
Knowing these milestones helps patients understand their recovery better.
RSA Rehabilitation Timeline and Milestones
RSA rehab is different because of the reversed shoulder design. The RSA rehab plan includes:
- Phase 1 (0-6 weeks): Use a sling and start passive exercises.
- Phase 2 (6-12 weeks): Do active assisted exercises and start strengthening.
- Phase 3 (3-6 months): Increase strength and functional training.
A leading orthopedic surgeon says, “RSA rehab needs patience and sticking to a plan for the best results.”
Return to Activities and Sports Considerations
Going back to activities and sports is important for TSA and RSA patients. The exact time varies based on the activity and the patient. Generally, most can start with low-impact activities in 3-6 months.
Helping patients recover well depends on good surgery, a solid rehab plan, and following it.
Surgical Decision-Making: Choosing Between RSA and TSA
Choosing between Reverse Shoulder Arthroplasty (RSA) and Total Shoulder Arthroplasty (TSA) starts with a detailed check-up before surgery. We look at many things like X-rays, the patient’s age, bone health, and how active they are.
Preoperative Assessment and Imaging Considerations
Before deciding, we use special tests like X-rays, CT scans, and MRI. These help us see how damaged the joint is, if the rotator cuff is okay, and the bone’s quality. This information helps us pick the best surgery.
Imaging findings that influence our decision include:
- The presence and severity of rotator cuff tears
- The extent of glenoid bone loss or deformity
- The condition of the humeral head and its positioning
Age-Related Factors in Procedure Selection
Age is a big factor in choosing between RSA and TSA. TSA is usually for younger people with a good rotator cuff because it keeps the joint more natural. RSA is better for older folks or those with big rotator cuff problems.
Bone Quality and Glenoid Morphology Assessment
The bone’s quality and the glenoid’s shape are key in picking RSA or TSA. If the bone is weak or the glenoid is worn out, RSA might be better because it’s more stable.
Assessment of bone quality involves evaluating:
- Bone density
- Glenoid version and inclination
- The presence of any bone defects or cysts
Patient Expectations and Lifestyle Considerations
We also think about what the patient wants and their lifestyle. We look at their activity level, job, and goals to choose the right surgery for them.
By looking at all these things, we make a choice that will make the patient happy and healthy. Choosing between RSA and TSA depends on the patient’s unique situation, not just a one-size-fits-all approach.
Conclusion: The Future of Shoulder Arthroplasty
Reverse shoulder replacements last about 85% to 90% of the time for 10 years. Patients are very happy, with satisfaction rates up to 95%. As we move forward, new implants and surgical methods are making both RSA and TSA better.
The choice between reverse shoulder arthroplasty vs total shoulder depends on the patient’s needs. Knowing about TSA is important for doctors and patients. RSA is very successful, mainly for big rotator cuff tears and rotator cuff arthropathy.
The debate between RSA and TSA will keep changing. We’re dedicated to giving our international patients the latest care. This ensures they get the best results.
FAQ
What is the main difference between Reverse Shoulder Arthroplasty (RSA) and Total Shoulder Arthroplasty (TSA)?
TSA works like the natural shoulder. RSA changes the ball-and-socket setup to help with rotator cuff issues.
What conditions are typically treated with Total Shoulder Arthroplasty?
TSA treats many issues. These include osteoarthritis, post-traumatic arthritis, avascular necrosis, and inflammatory diseases.
When is Reverse Shoulder Arthroplasty preferred over Total Shoulder Arthroplasty?
RSA is better for rotator cuff tears, complex fractures, failed surgeries, and big rotator cuff tears.
What are the possible complications with TSA and RSA?
Both can face issues like infection, implant failure, and nerve damage. Proper care and selection are key to avoid these problems.
How do rehabilitation protocols differ between TSA and RSA?
Early care is similar, but recovery times and goals can differ. Knowing these differences helps in a better recovery.
What factors influence the decision between RSA and TSA?
Many things matter, like the patient’s condition, age, bone quality, and what they hope to achieve. Choosing the right surgery is important.
What is the significance of proper patient selection for shoulder arthroplasty?
Choosing the right patient is vital for good results. It means looking at the patient’s health and lifestyle carefully.
How has the technology in RSA and TSA evolved?
New materials and designs have made both surgeries better. Ongoing research keeps improving these treatments.
Can patients return to sports and activities after RSA or TSA?
Yes, but it depends on the surgery and how well the patient recovers. A good rehab plan is key for a good outcome.
What is the role of Liv Hospital in treating international patients with shoulder arthroplasty needs?
Liv Hospital offers top-notch care for international patients. Our team supports patients every step of the way.
References
- PubMed / PMC. PMC Article with ID 32897677. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32897677/