Last Updated on December 1, 2025 by Bilal Hasdemir
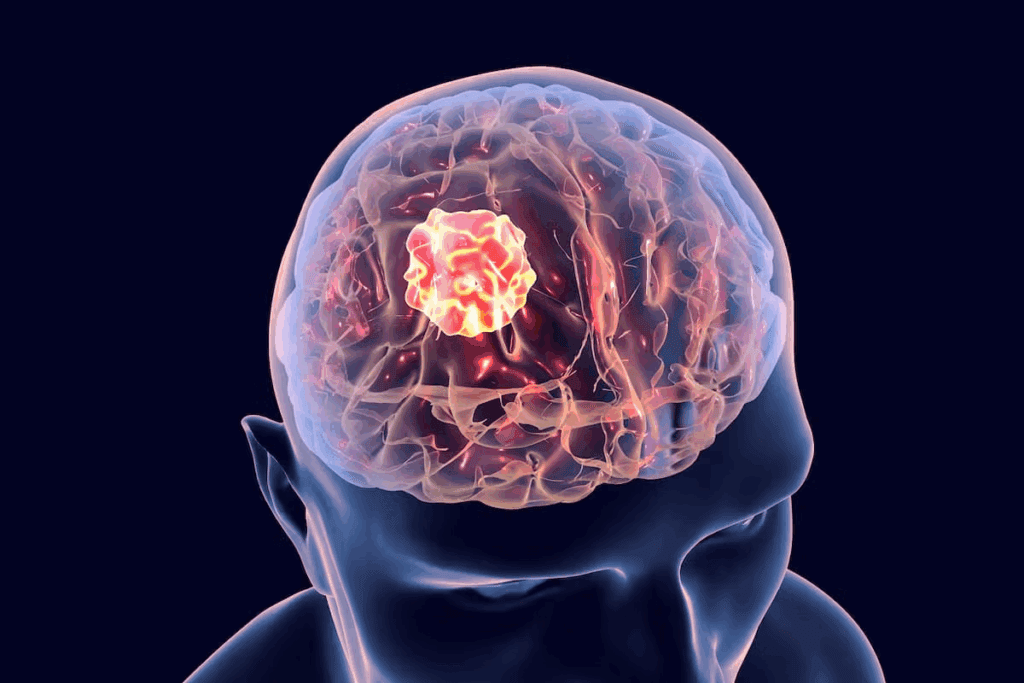
Rhabdomyosarcoma is a rare cancer that mainly affects kids. It can spread to different parts of the body. A big worry is that it might go to the brain, causing serious problems.
There’s a lot of interest in pediatric cancer research to figure out why this happens. Studies show that brain metastasis in rhabdomyosarcoma patients is rare but very tough to handle.
It’s important to understand how Rhabdomyosarcoma Brain Metastasis works in tumor progression. This knowledge helps us find better ways to treat it. We aim to make this complex issue clearer.
Key Takeaways
- Rhabdomyosarcoma can metastasize to the brain, posing serious health risks.
- Pediatric cancer research is key to understanding how metastasis works.
- Brain metastasis in rhabdomyosarcoma patients is rare but hard to treat.
- Knowing how brain tumors progress is vital for effective treatments.
- More research is needed to help patients better.
Understanding Rhabdomyosarcoma: A Complete Overview
Rhabdomyosarcoma is a cancer that affects soft tissues, mainly in children. It’s important to know what it is, how it’s classified, and its genetic makeup.
Definition and Classification of Rhabdomyosarcoma
Rhabdomyosarcoma starts in muscle cells and grows quickly. It can spread to other parts of the body. It’s divided into three main types: embryonal, alveolar, and pleomorphic.
“We recognize that rhabdomyosarcoma is not a single disease entity but a range of cancers with unique traits,” says Dr. [Last Name], a top oncologist. “Knowing these differences helps us find better treatments.”
Cellular and Genetic Characteristics
The cells and genes of rhabdomyosarcoma are complex. Scientists have found certain genetic changes that help the cancer grow. For example, PAX3-FOXO1 or PAX7-FOXO1 genes are key in alveolar rhabdomyosarcoma.
New tools in molecular biology have given us a better look at rhabdomyosarcoma. This knowledge is helping us create new treatments.
Historical Context and Research Evolution
Research on rhabdomyosarcoma has a long history. Early studies focused on its symptoms and how it looks under a microscope. But, our understanding has grown a lot thanks to new science and technology.
As we keep learning about rhabdomyosarcoma, we see how much we’ve accomplished. “The progress we make in understanding cancer shows our creativity and dedication to finding answers,” a leading researcher said.
Epidemiology of Rhabdomyosarcoma in the United States
The study of rhabdomyosarcoma in the U.S. gives us important insights. It shows how common this rare cancer is and who it affects most. This cancer is aggressive and hard to diagnose and treat.
Incidence and Prevalence Statistics
Rhabdomyosarcoma is rare in adults but common in kids. Pediatric cancer statistics show it affects about 4.5 kids per million under 20. It’s most common in kids under 10, with a peak between 2 and 5 years old.
The number of cases hasn’t changed much in years. But, thanks to better medical research methodology and treatments, more kids are surviving.
Age and Demographic Distribution
Rhabdomyosarcoma’s age pattern shows two peaks: in early childhood and late teens. Embryonal rhabdomyosarcoma mainly hits young kids. Alveolar rhabdomyosarcoma is more common in older kids and teens.
More boys get rhabdomyosarcoma than girls. The disease also affects different ethnic groups differently. Caucasians tend to have a higher rate than others.
Trends in Diagnosis and Detection
New cancer diagnostic approaches have changed how we find and treat rhabdomyosarcoma. Better imaging like MRI and PET scans help us diagnose and plan treatment better.
Thanks to better awareness and molecular tests, we can catch rhabdomyosarcoma earlier. This leads to more tailored and effective treatments.
Types and Subtypes of Rhabdomyosarcoma
Rhabdomyosarcoma is a complex cancer with many types and subtypes. These are based on the cancer cells and their genetic makeup. Knowing these differences is key for diagnosis, treatment, and research.
Embryonal Rhabdomyosarcoma
Embryonal Rhabdomyosarcoma is the most common type in kids. It often appears in the head, neck, or genitourinary tract. It looks like embryonic muscle cells.
This subtype varies in how mature the cells are. They can range from very primitive to almost muscle-like.
Alveolar Rhabdomyosarcoma
Alveolar Rhabdomyosarcoma is another important type. It’s found in the arms, legs, and trunk. It has a unique cell arrangement and specific genetic changes.
This type is more aggressive than embryonal Rhabdomyosarcoma. It tends to grow faster and be more challenging to treat.
Pleomorphic and Other Rare Subtypes
Pleomorphic Rhabdomyosarcoma is rare and aggressive. It’s more common in adults. It has very abnormal cells.
Other rare types include spindle cell/sclerosing Rhabdomyosarcoma. This type has spindle-shaped cells and a specific background.
Classifying Rhabdomyosarcoma into subtypes helps with diagnosis and treatment. Knowing the exact subtype is vital for choosing the right treatment.
Research is ongoing to understand these subtypes better. This could lead to targeted treatments that target each subtype’s weaknesses.
Primary Sites and Common Locations of Rhabdomyosarcoma
Knowing where rhabdomyosarcoma often starts is key for early treatment. This soft tissue cancer can pop up in many places, with some spots more common than others.
Head and Neck Regions
The head and neck are top spots for rhabdomyosarcoma, mainly in kids. Tumors can show up around the eye, near the brain, or in the nasal cavity or neck. Doctors face big challenges here, like keeping important parts working while removing the tumor.
Genitourinary Tract
The genitourinary tract is another big area for rhabdomyosarcoma. This includes the bladder, prostate, vagina, and areas around the testicles. Symptoms can vary, like trouble with urine or sex, based on where the tumor is. Spotting it early is super important to avoid serious problems and get better results.
- Bladder and prostate tumors can block or hold urine.
- Vaginal tumors might cause bleeding or discharge.
- Paratesticular tumors can lead to testicle pain or swelling.
Extremities and Other Sites
Rhabdomyosarcoma can also appear in arms and legs, and less often in the trunk or chest. Tumors in arms and legs might have a different outlook than others. Being able to remove the tumor completely is a big factor in how well a patient does.
- Extremity tumors need careful planning to keep the limb working.
- Tumors in the trunk or chest can be hard to get to and might need more than one treatment.
In short, where rhabdomyosarcoma starts really matters for treatment and how well a patient does. Doctors need to know these common spots to plan the best care for each patient.
The Metastatic Process: How Cancer Spreads
Metastasis is when cancer cells move from the main tumor to other parts of the body. It’s a complex process with several steps. Knowing these steps helps us find better treatments for cancers like rhabdomyosarcoma.
Mechanisms of Cancer Cell Migration
Cancer cell migration is key in metastasis. It’s how cancer cells move from the main tumor to other areas. This happens through changes in how cells stick together and move, and by breaking down the tissue around them.
Research shows that Ras transformation in human cells is important for this migration. When Ras proteins are active, cells can move and spread more easily.
Common Metastatic Pathways
Cancer cells can spread through the lymphatic system or the bloodstream. The path they take depends on the cancer type and where the tumor is. For rhabdomyosarcoma, common places for metastasis are the lungs, bone marrow, and bones.
The spread of cancer is not random. It follows certain patterns based on how cancer cells interact with their surroundings. Knowing these patterns helps us predict where cancer will spread and develop targeted treatments.
Factors Influencing Metastatic Potentia
Many things can affect how likely cancer cells are to spread. These include genetic changes, the environment around the tumor, and the immune system. For example, some genetic changes can make cells more likely to invade and spread.
The environment around the tumor also matters. It can send signals that help or hinder cell migration and invasion. The immune system can also play a role by fighting cancer cells or helping them grow.
Understanding how cancer cells migrate, the common paths they take, and what influences their spread is key. This knowledge is vital for creating effective treatments and improving outcomes for patients with rhabdomyosarcoma.
Rhabdomyosarcoma Brain Metastasis: Incidence and Patterns
Brain metastasis in rhabdomyosarcoma patients is a big challenge in cancer treatment. It’s important to look at how often it happens and its patterns. Rhabdomyosarcoma is a fast-growing cancer that can spread to different parts of the body, including the brain.
Frequency of Brain Involvement
Brain involvement in rhabdomyosarcoma is not as common as in other cancers. But when it does happen, it makes treatment harder and can change patient outcomes. Research shows that how often brain metastasis occurs depends on the type and where the tumor starts.
Embryonal rhabdomyosarcoma and alveolar rhabdomyosarcoma have different chances of spreading to the brain. Knowing this helps doctors plan the best treatment for each patient.
Risk Factors for CNS Spread
Several things can increase the chance of CNS spread in rhabdomyosarcoma patients. These include where the tumor is, the type of tumor, and if there’s already metastasis at diagnosis. Tumors in the head and neck area might be more likely to spread to the brain.
- Primary tumor site
- Histological subtype
- Presence of metastatic disease at diagnosis
Finding out these risk factors early can help doctors keep a closer eye on patients. This might help stop CNS spread before it starts.
Comparison with Other Metastatic Sites
Rhabdomyosarcoma can spread to places like the lungs, bones, and lymph nodes. Looking at how brain metastasis compares to these sites can give us clues about the disease. The ways it spreads to the brain might be different from how it spreads to other parts of the body.
Knowing these differences is key to creating treatments that can fight brain metastasis in rhabdomyosarcoma patients.
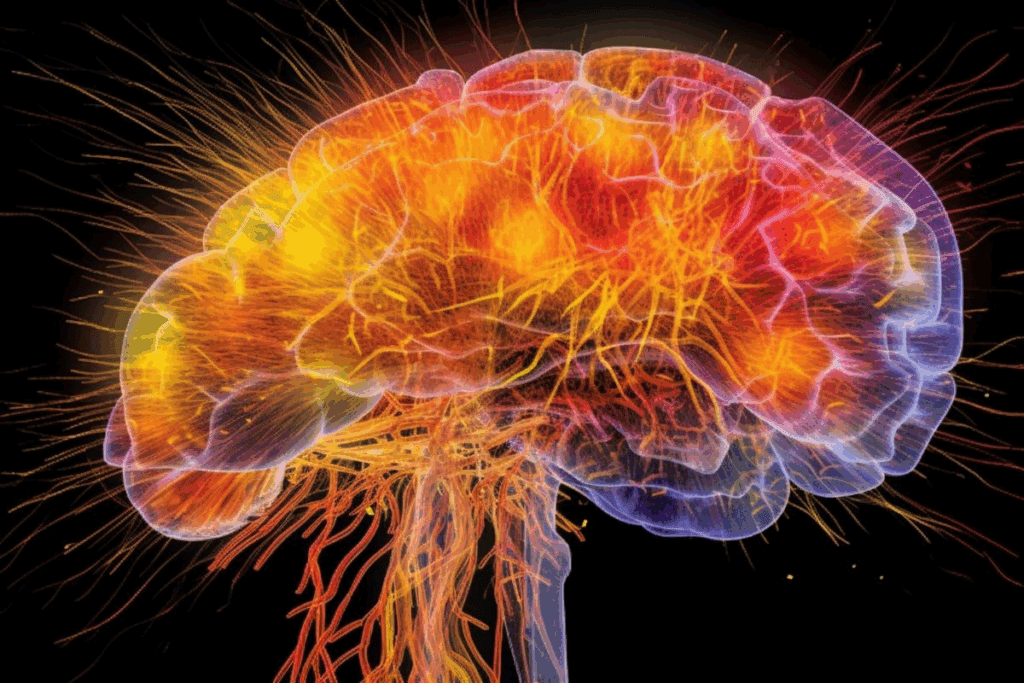
Pathophysiology of Brain Metastasis in Rhabdomyosarcoma
The study of brain metastasis in rhabdomyosarcoma is complex. It involves the blood-brain barrier, molecular mechanisms, and the tumor microenvironment. Knowing these details is key to finding effective treatments.
Blood-Brain Barrier Considerations
The blood-brain barrier (BBB) is vital in brain metastasis. It controls what enters the brain from the bloodstream. Cancer cells must get past this barrier to spread to the brain. The BBB’s integrity is key to stopping CNS invasion, but breaking it lets metastatic cells in.
“The blood-brain barrier is not just a physical block; it’s a dynamic interface,” says recent research. “Cancer cells must navigate it to colonize the brain.”
Molecular Mechanisms of Brain Invasion
Brain invasion by cancer cells involves many molecular steps. Adhesion molecules, proteases, and signaling pathways help cells stick to, invade, and survive in the brain. Specific molecular signatures are linked to brain metastasis in rhabdomyosarcoma.
- Adhesion molecules help cancer cells attach to the BBB.
- Proteases break down the extracellular matrix, allowing invasion.
- Signaling pathways support cancer cell survival and growth in the CNS.
Tumor Microenvironment in the CNS
The CNS tumor microenvironment is key in supporting or blocking metastatic rhabdomyosarcoma growth. Astrocyte interactions, immune responses, and nutrient and oxygen availability affect cancer cell growth in the brain.
As we learn more about the CNS microenvironment, we might find new treatment targets. “Understanding the complex CNS microenvironment is essential for new brain metastasis treatments,” says recent research.
Clinical Presentation and Symptoms of Brain Metastasis
It’s important to know the symptoms of brain metastasis in rhabdomyosarcoma. This happens when cancer cells spread to the brain. It causes various neurological symptoms.
Neurological Manifestations
The symptoms of brain metastasis in rhabdomyosarcoma can differ. Common signs include headaches, seizures, and confusion. These happen due to increased pressure in the brain or the tumor touching brain tissue.
These symptoms greatly affect a patient’s quality of life. They are part of cancer neurological involvement.
| Symptom | Frequency | Clinical Implication |
| Headaches | 60% | Increased intracranial pressure |
| Seizures | 30% | Direct tumor invasion or irritation |
| Confusion | 40% | Cognitive impairment due to tumor or treatment effects |
Differences Between Pediatric and Adult Presentations
The symptoms of brain metastasis vary between kids and adults. Kids might show irritability or lethargy, making it harder to diagnose. Adults often have more specific symptoms related to the tumor’s location.
Pediatric diagnostic methods need to be able to catch these differences early.
Early Warning Signs and Symptoms
Spotting brain metastasis early is key to better outcomes. Look out for signs like persistent headaches, visual disturbances, or changes in mental status. Using medical screening techniques like MRI or CT scans can help catch it early.
In conclusion, brain metastasis symptoms in rhabdomyosarcoma are complex. Understanding these symptoms and using the right diagnostic tools can improve patient care and quality of life.
Diagnostic Approaches for Detecting Brain Metastasis
Finding brain metastasis early is key for good treatment and care. Doctors use advanced tech and methods to spot it in rhabdomyosarcoma patients.
Imaging Techniques and Their Efficacy
Imaging is vital for spotting brain metastasis. Magnetic Resonance Imaging (MRI) is top-notch because it’s very sensitive and shows soft tissues well. It helps find where, how big, and how many metastases are, which is important for planning treatment.
Computed Tomography (CT) scans are used too, mainly in urgent cases. They’re quicker and more common than MRI. But, they’re not as good at finding small brain metastases as MRI is.
- MRI is highly sensitive for detecting brain metastases.
- CT scans are useful in emergency situations.
- Other imaging techniques like PET scans can provide additional information on metabolic activity.
Laboratory and Pathological Assessments
Lab and pathological tests are key to confirming brain metastasis. Lumbar puncture (LP), or spinal tap, checks cerebrospinal fluid for cancer cells. This helps spot leptomeningeal metastasis.
Looking at tissue samples from biopsies or surgeries is the best way to confirm brain metastasis. Immunohistochemistry helps find specific tumor markers.
- Lumbar puncture helps diagnose leptomeningeal metastasis.
- Histopathological examination confirms the diagnosis.
- Immunohistochemistry identifies specific tumor markers.
Emerging Diagnostic Technologies
New tech is making it easier to find brain metastasis. Liquid biopsy analyzes tumor DNA in blood or CSF. It might spot metastasis sooner and track how well treatments work.
Other new things include artificial intelligence (AI) in imaging. It can make diagnoses more accurate and faster.
- Liquid biopsy can detect metastasis earlier.
- AI applications improve diagnostic accuracy.
- Emerging technologies enhance treatment monitoring.
Treatment Strategies for Rhabdomyosarcoma with Brain Involvement
Dealing with rhabdomyosarcoma that has spread to the brain is complex. We use many treatment methods to fight this disease. We’ll look at the best and latest ways to treat it.
Surgical Interventions
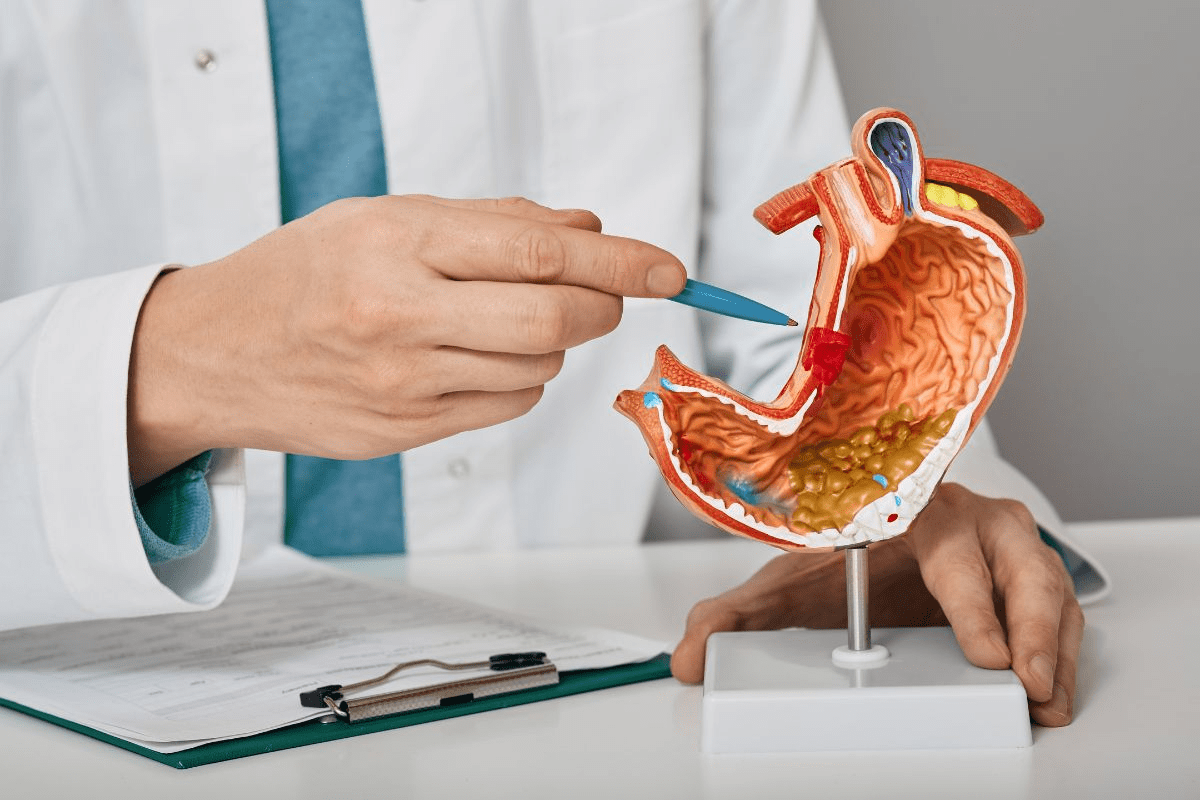
Surgery is key for treating rhabdomyosarcoma, mainly for tumors that are in one place. But, when the cancer reaches the brain, surgery is harder and depends on each case.
We check if surgery is possible based on the tumor’s location, size, and the patient’s health. Sometimes, surgery helps by easing symptoms or shrinking the tumor.
Radiation Therapy Approaches
Radiation therapy is very important for treating rhabdomyosarcoma that has spread to the brain. We use advanced methods like IMRT and proton therapy. These methods aim to hit the tumor hard while protecting healthy tissues.
Choosing the right radiation therapy depends on how much the brain is involved and the patient’s past treatments. We work with radiation oncologists to create a treatment plan that fits each patient.
Systemic Chemotherapy Protocols
Chemotherapy is a big part of treating rhabdomyosarcoma, even more so when it has spread. We use different chemotherapy mixes to attack the cancer better.
Choosing the chemotherapy depends on the patient’s age, the type of tumor, and what treatments they’ve had before. We keep an eye on how the patient responds to adjust the treatment as needed.
Targeted Therapies and Immunotherapies
Targeted therapies and immunotherapies are new and promising ways to fight rhabdomyosarcoma. We look into treatments that target specific tumor molecules and immunotherapies that use the body’s immune system against cancer.
As we learn more about rhabdomyosarcoma, we can make treatment plans that are more tailored to each patient. This means using the best strategies for each person’s case.
| Treatment Modality | Key Considerations | Potential Benefits |
| Surgical Interventions | Tumor location, patient health | Symptom relief, tumor reduction |
| Radiation Therapy | Tumor extent, previous treatments | Precise tumor targeting, minimized side effects |
| Chemotherapy | Patient age, tumor histology | Effective against metastatic disease, combination regimens |
| Targeted & Immunotherapies | Molecular targets, immune system modulation | Personalized treatment, potentially better outcomes |
Prognosis and Survival Rates for Patients with Brain Metastasis
Brain metastasis in rhabdomyosarcoma patients greatly affects their survival chances. Knowing what influences prognosis is key to creating effective treatment plans.
Prognostic Factors and Indicators
Several factors are key in assessing prognosis for patients with brain metastasis. These include:
- Tumor size and location: Larger tumors or those in critical areas may have a worse prognosis.
- Patient age and overall health: Younger patients or those with fewer health issues may have better survival rates.
- Response to initial treatment: Patients who respond well to initial therapy may have a better prognosis.
- Presence of extracranial disease: The extent of disease outside the brain can affect overall survival.
Long-term Survival Statistics
Long-term survival rates for patients with brain metastasis vary. This depends on several factors, including those mentioned above. Recent studies in pediatric oncology research have shed light on survival trends.
| Patient Group | 1-Year Survival Rate | 5-Year Survival Rate |
| Pediatric Patients | 60% | 30% |
| Adult Patients | 40% | 15% |
These statistics show the survival rate difference between pediatric and adult patients.
Quality of Life Considerations
In addition to survival rates, quality of life is vital for patients with brain metastasis. Factors like neurological function, symptom management, and psychological support are key to patient outcomes.
We understand that keeping quality of life is essential for patients with brain metastasis. This involves not just medical criteria but also full supportive care.
Current Clinical Trials and Research Directions
Ongoing clinical trials are key in improving our fight against Rhabdomyosarcoma, even when it spreads to the brain. These efforts are at the heart of medical progress. They bring new hope and treatments to patients and their families.
Significant strides are being made in treating children with cancer. This is thanks to thorough research and clinical trials. The goal is not just to cure the cancer but also to enhance the patient’s quality of life.
Promising Investigational Therapies
Several new therapies are showing great promise in treating Rhabdomyosarcoma with brain metastasis. These include:
- Targeted therapies that focus on specific genetic mutations
- Immunotherapies that harness the body’s immune system to fight cancer
- Advanced radiation techniques that minimize damage to surrounding brain tissue
Table: Emerging Therapies in Rhabdomyosarcoma
| Therapy Type | Description | Potential Benefits |
| Targeted Therapy | Focuses on specific genetic mutations driving the cancer | Reduced side effects, improved efficacy |
| Immunotherapy | Harnesses the immune system to recognize and attack cancer cells | Potential for long-term cancer control, fewer side effects |
| Advanced Radiation | Precise radiation delivery to minimize damage to surrounding tissue | Reduced risk of neurological complications |
Participation Opportunities and Eligibility
Clinical trials give patients access to new treatments not available elsewhere. The criteria for joining vary by trial. They often look at age, health, and cancer specifics.
We urge patients and families to talk with their doctors about clinical trials. Joining clinical trials helps advance medical science. It also offers patients cutting-edge treatments.
Breakthrough Discoveries in Pediatric Oncology
Recent years have brought major breakthroughs in treating children’s cancer. We now understand more about Rhabdomyosarcoma’s genetics. And we have treatments that are more effective and less harsh.
These advances show the strength of teamwork in research. They highlight the commitment of the medical and scientific fields to better outcomes for kids with cancer.
Supportive Care and Management of Neurological Complications
Managing brain metastasis complications needs a detailed plan. Rhabdomyosarcoma in the brain is tough to handle. Good supportive care is key to better patient outcomes.
Symptom Management Approaches
Managing symptoms is vital for patients with brain metastasis. We use many ways to ease symptoms like headaches and seizures. Each patient gets care that fits their needs.
Pharmacological interventions include steroids for swelling and pain meds. Palliative care aims to improve life quality for patients and their families.
Rehabilitation Strategies
Rehabilitation helps patients regain lost abilities. We create individualized rehabilitation plans for each patient. This may include physical and speech therapy.
Rehab helps patients adjust to their new situation. Our team works with patients and families to set and meet goals.
Psychosocial Support for Patients and Families
Brain metastasis affects patients and families deeply. We offer psychosocial support to help them cope.
Our support includes counseling and educational resources. We aim to improve the well-being of patients and their families.
Conclusion: The Future Landscape of Rhabdomyosarcoma Brain Metastasis Management
Rhabdomyosarcoma brain metastasis is a big challenge in pediatric oncology. We need to understand how it spreads, improve diagnosis, and find better treatments. This is key to helping patients.
Recent studies have helped us understand rhabdomyosarcoma and its brain spread. More research is finding new ways to treat it. Working together is important to make progress in treating rhabdomyosarcoma brain metastasis.
Looking ahead, we must keep innovating and funding research on rhabdomyosarcoma. This will help increase survival rates and improve life quality for those affected. By learning more about this disease, we can find better ways to manage it and help patients.
FAQ
What is rhabdomyosarcoma and how does it spread to the brain?
Rhabdomyosarcoma is a cancer that starts in soft tissues, like muscles. It can reach the brain through the blood or lymph system. The exact ways it spreads are complex and involve many molecular and cellular processes.
What are the different subtypes of rhabdomyosarcoma?
There are three main types: embryonal, alveolar, and pleomorphic. Each type has its own traits and genetic makeup. These differences affect how doctors diagnose and treat the cancer.
How common is brain metastasis in rhabdomyosarcoma patients?
Brain metastasis is rare in rhabdomyosarcoma patients. It mostly happens in advanced or recurring cases. The chance of brain involvement depends on the tumor’s type and where it started.
What are the symptoms of brain metastasis in rhabdomyosarcoma?
Symptoms include headaches, seizures, confusion, weakness, and vision or speech changes. The symptoms vary based on the metastasis’s location and size.
How is brain metastasis diagnosed in rhabdomyosarcoma patients?
Doctors use MRI or CT scans, lab tests, and pathology to diagnose. New technologies like molecular and genetic testing are also used.
What are the treatment options for rhabdomyosarcoma with brain metastasis?
Treatments include surgery, radiation, chemotherapy, and targeted or immunotherapies. The choice depends on the disease’s extent, the patient’s age, and health.
What is the prognosis for patients with rhabdomyosarcoma brain metastasis?
Prognosis varies based on disease extent, treatment response, and overall health. Long-term survival and quality of life are key in patient care.
Are there any ongoing clinical trials for rhabdomyosarcoma with brain metastasis?
Yes, there are trials for new treatments, including for brain metastasis. These trials test promising therapies and encourage patient participation.
What supportive care measures are available for patients with neurological complications?
Supportive care includes managing symptoms, rehabilitation, and psychosocial support. It’s vital for the complex needs of these patients.
How can patients and families access information about rhabdomyosarcoma and brain metastasis?
Information is available from cancer organizations, medical journals, and healthcare providers. Staying updated with research and treatments is important.
What are the current research directions in pediatric oncology for rhabdomyosarcoma?
Research focuses on new targets, better diagnostics, and effective treatments. Breakthroughs in pediatric oncology are continually evolving the field.
References:
- Abdelhafeez, A. H. (2025). Evidence-Based Surgical Guidelines for Treating Children With Rhabdomyosarcoma. Pediatric Blood & Cancer. https://pubmed.ncbi.nlm.nih.gov/39870584/