Last Updated on December 1, 2025 by Bilal Hasdemir

Finding rhabdomyosarcoma early is key to successful treatment. This rare cancer often shows up with vague symptoms. This makes it hard to catch it on time.
About 350 kids in the U.S. get this cancer each year. This shows why doctors and everyone else need to know about it.
Knowing the symptoms of rhabdomyosarcoma and using the right diagnostic tests are important. They help get a quick and correct rhabdomyosarcoma diagnosis.
Key Takeaways
- Early detection of rhabdomyosarcoma improves treatment outcomes.
- Symptoms of rhabdomyosarcoma can be non-specific and vary by location.
- Diagnostic tests play a critical role in accurately diagnosing the condition.
- Awareness among healthcare providers is essential for timely diagnosis.
- Understanding diagnostic approaches is vital for effective patient care.
Understanding Rhabdomyosarcoma: An Overview
Rhabdomyosarcoma is a rare cancer that starts in muscle cells. It’s a big worry in kids’ cancer care. This aggressive cancer can happen at any age but hits kids and teens the hardest.
Definition and Types of Rhabdomyosarcoma
Rhabdomyosarcoma is a cancer that comes from muscle cells. It’s a type of soft tissue sarcoma. There are different kinds, each with its own look and treatment needs.
- Embryonal rhabdomyosarcoma is the most common type. It usually affects kids under 10.
- Alveolar rhabdomyosarcoma is more common in older kids and teens.
- Spindle cell/sclerosing rhabdomyosarcoma is rare. It has unique features.
Each type looks different under a microscope. They also have different chances of recovery.
Epidemiology and Risk Factors
Rhabdomyosarcoma is a big deal in kids’ cancer. It makes up about 3-5% of all childhood cancers. It’s one of the top soft tissue sarcomas in kids.
It’s more common in younger kids for one type and older kids for another. Some kids might be at higher risk because of their genes or because of things they’ve been exposed to.
Common Signs and Symptoms of Rhabdomyosarcoma
Knowing the signs and symptoms of Rhabdomyosarcoma is key to getting help quickly. This cancer can show up in different parts of the body. The symptoms depend on where the tumor is.
Location-Specific Symptoms
The symptoms of Rhabdomyosarcoma change based on the tumor’s location. For example, tumors in the head and neck might cause swelling, pain, or trouble swallowing. Tumors in the genitourinary tract can lead to blood in the urine or trouble peeing.
Common location-specific symptoms include:
- Swelling or a mass in the affected area
- Pain or discomfort
- Difficulty moving the affected limb or area
- Protrusion or bulging in the case of orbital (eye socket) tumors
Being aware of these symptoms helps with early detection.
Systemic Symptoms
Rhabdomyosarcoma can also cause symptoms that affect the whole body. These include:
- Fever
- Weight loss
- Fatigue or feeling weak
These symptoms can be hard to spot early. But, when combined with location-specific symptoms, they help doctors diagnose the cancer.
To better understand the variety of symptoms associated with Rhabdomyosarcoma, let’s examine the following summary table:
| Tumor Location | Common Symptoms |
| Head and Neck | Swelling, pain, difficulty swallowing |
| Genitourinary Tract | Hematuria, difficulty urinating |
| Limbs | Swelling, pain, limited mobility |
Spotting these symptoms is the first step to early detection and treatment of Rhabdomyosarcoma. If you or someone you know has any of these symptoms, seek medical help right away.
When to Seek Medical Attention
Knowing the warning signs of rhabdomyosarcoma is key to early detection. Spotting these signs early can greatly improve treatment outcomes.
Warning Signs That Require Immediate Evaluation
Some symptoms point to rhabdomyosarcoma and need quick medical check-ups. These include:
- Rapid tumor growth: A quickly growing lump or swelling can be a sign of rhabdomyosarcoma.
- Severe pain: Persistent and severe pain, often with a lump or swelling, needs medical help.
- Neurological symptoms: Numbness, tingling, or weakness in body parts can mean nerve issues.
- Difficulty swallowing or breathing: Tumors in the head and neck can cause these symptoms, needing fast evaluation.
Risk Factors That Increase Suspicion
Knowing the risk factors for rhabdomyosarcoma helps spot high-risk individuals. These include:
- Genetic predisposition: Certain genetic conditions, like Li-Fraumeni syndrome, raise the risk.
- Family history: A family history of cancer, mainly soft tissue sarcomas, increases risk.
- Previous radiation exposure: Those who had radiation therapy for other cancers face higher risk.
If you or someone you know shows these warning signs or has risk factors, seek medical help right away. Early detection and diagnosis are vital for effective treatment.
The Initial Clinical Evaluation
Spotting rhabdomyosarcoma begins with a detailed first check-up. This key step collects all the info needed about the patient’s health. It involves a deep dive into their medical past and a careful physical check.
Medical History Assessment
Understanding a patient’s medical past is key. We look for signs and risks linked to rhabdomyosarcoma. We ask about past health issues, treatments, and surgeries. We also check the family’s health history for genetic clues.
We pay close attention to the patient’s current symptoms. We want to know how long they’ve had them, how bad they are, and what makes them better or worse. This helps us figure out if rhabdomyosarcoma is likely and what tests to run next.
Physical Examination Techniques
A detailed physical check is also vital. We use different methods to see how the patient is doing and find any signs of rhabdomyosarcoma.
We look closely at the affected area for swelling, pain, or stiffness. We also check the lymph nodes for any growth, which could mean the cancer has spread. Plus, we do a full body check for any other symptoms that might point to rhabdomyosarcoma.
By combining what we learn from the medical history and physical exam, we decide if more diagnostic tests for rhabdomyosarcoma are needed. Then, we create a care plan for the patient.
Rhabdomyosarcoma Diagnosis: The Complete Process
Getting a correct diagnosis for rhabdomyosarcoma needs a detailed and team-based method. This process involves many tests and steps.
Diagnostic Pathway Overview
The first step is a detailed medical history and physical check-up. Imaging studies are key to finding the tumor and seeing how big it is.
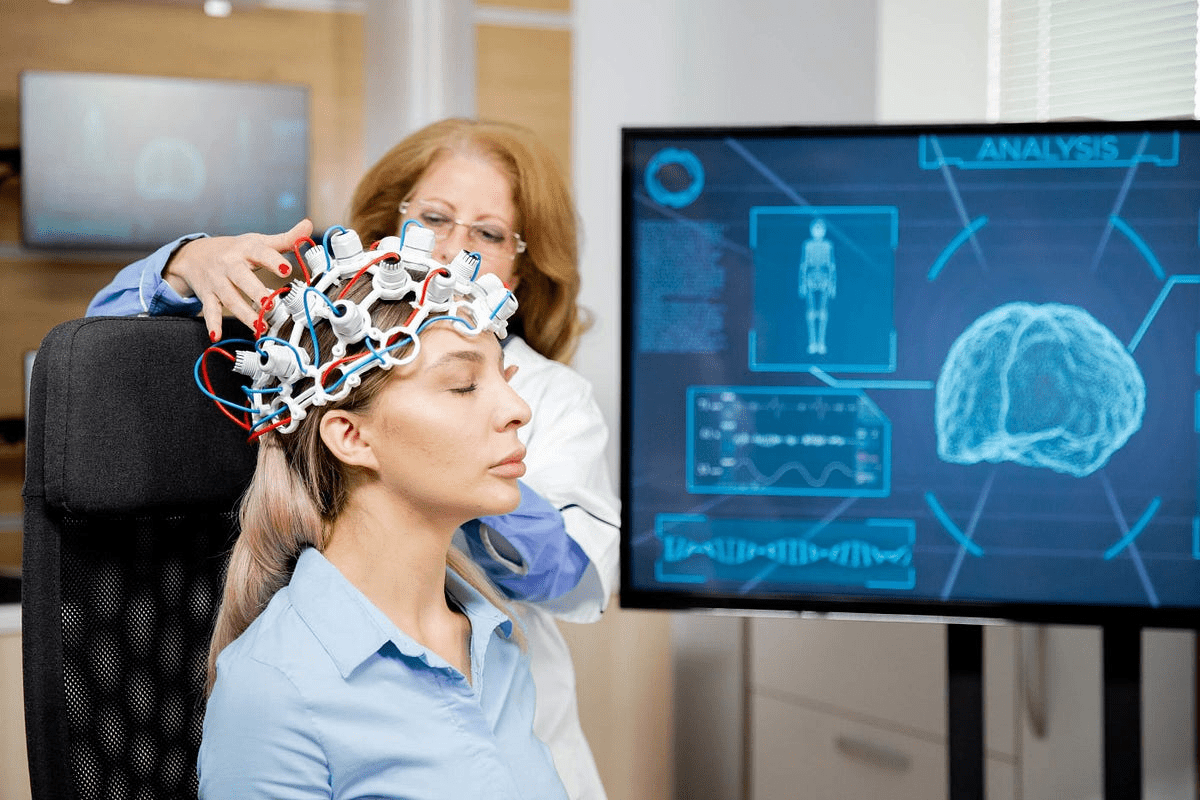
We use MRI, CT scans, and ultrasound to see the tumor. Each method gives us different info, helping us understand the tumor better.
Multidisciplinary Approach to Diagnosis
Working together is key to a correct diagnosis of rhabdomyosarcoma. This means radiologists, pathologists, surgeons, and oncologists all play a part. They make sure every detail is looked at.
“A precise diagnosis is the cornerstone of effective treatment planning for rhabdomyosarcoma patients.” -Expert Opinion
Teamwork is vital in finding the right diagnosis. It brings together different views and skills, leading to a more accurate diagnosis.
- Integration of imaging studies and biopsy results
- Collaboration among specialists
- Comprehensive assessment of tumor characteristics
By using a team effort and a detailed diagnostic path, we make sure patients get the right diagnosis and treatment.
Imaging Techniques for Detecting Rhabdomyosarcoma
Imaging techniques are key in finding and managing rhabdomyosarcoma. They help spot the tumor, see how big it is, and plan the best treatment.
Magnetic Resonance Imaging (MRI)
MRI is great for soft tissue tumors like rhabdomyosarcoma. It shows the tumor’s size, where it is, and how it affects nearby areas. MRI is best for tumors in tricky spots, like the head and neck or pelvis.
We use MRI to see how far the tumor has spread. It helps us plan surgery and check if we can remove the tumor.
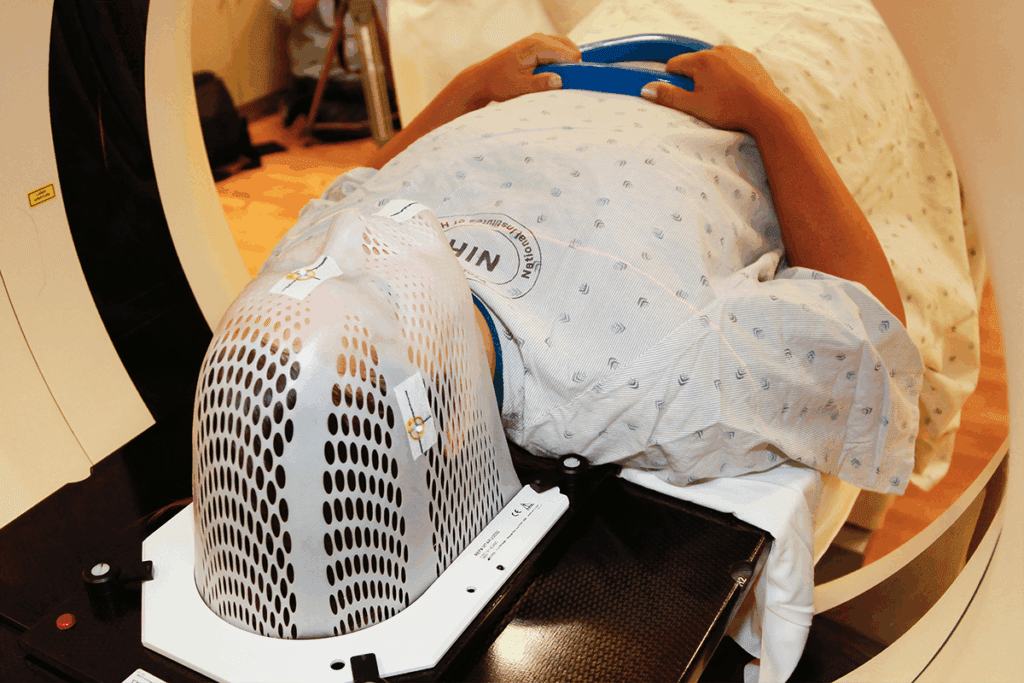
Computed Tomography (CT) Scans
CT scans are also very important for diagnosing rhabdomyosarcoma. They show soft tissues and bones well, helping find tumors and see how they affect bones.
CT scans are great for the chest and abdomen. They help find tumors and check for cancer spread to lymph nodes or other organs.
Ultrasound Applications
Ultrasound is useful, too, for tumors that are easy to reach or for biopsies. It’s safe because it doesn’t use radiation. It’s good for first checks or watching how treatment works.
We use ultrasound for tumors in easy-to-get-to places, like arms or the belly. It shows what’s happening in real time, helping us see blood flow and guide treatments.
Advanced Imaging Methods
Advanced imaging techniques are key in diagnosing and staging rhabdomyosarcoma. They give insights into tumor biology. This helps doctors understand how far the disease has spread and plan the best treatment.
PET Scans for Metabolic Activity
PET (Positron Emission Tomography) scans help see how active tumors are. They spot areas where cancer cells are growing fast. This is important for knowing how aggressive the cancer is and if treatment is working.
Bone Scans for Metastatic Disease
Bone scans find cancer that has spread to bones. They use a small amount of radioactive material to show where cancer is. Finding cancer early in bones is key to better treatment and outcomes.
Whole-Body MRI Protocols
Whole-body MRI gives a full view of tumors and possible spread without radiation. It’s great for kids and tracking disease changes. MRI shows the main tumor and any spread, helping in accurate treatment planning.
Using these advanced imaging methods together helps doctors understand rhabdomyosarcoma better. This leads to more tailored treatments and better chances of recovery.
Biopsy Procedures: The Gold Standard for Diagnosis
Diagnosing rhabdomyosarcoma often starts with a biopsy. This is because biopsies are seen as the top choice for cancer diagnosis. They involve taking tissue or cells from the body for a microscope check. This is key to finding out if cancer is present and what type it is.
Types of Biopsies Used
There are many biopsy types for diagnosing rhabdomyosarcoma. Each has its own use and benefits. Here are a few:
- Incisional Biopsy: This involves taking a part of the tumor.
- Excisional Biopsy: This means removing the whole tumor.
- Core Needle Biopsy: A less invasive method using a needle to get tissue samples.
- Fine-needle Aspiration Biopsy: Uses a thin needle to collect cell samples.
The right biopsy type depends on the tumor’s size, location, and the patient’s health.
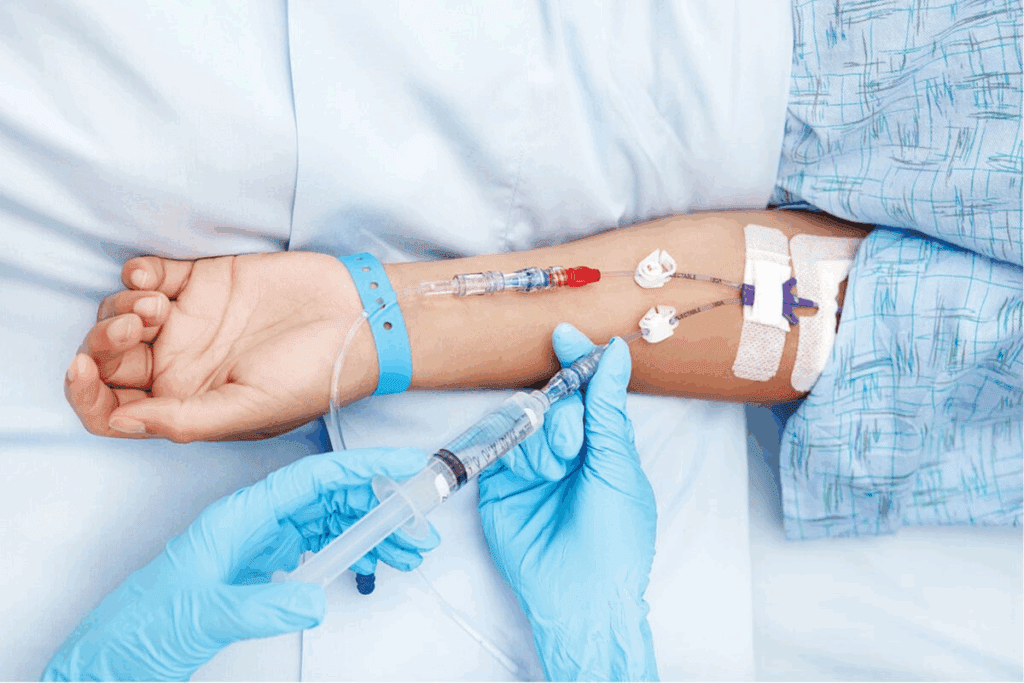
Biopsy Planning and Execution
Planning and doing biopsies well is key for accurate results. This means:
- Picking the best biopsy method for the tumor.
- Making sure the patient is ready and knows what’s happening.
- Using tools like ultrasound or CT scans to help get the right tissue.
Good planning and doing biopsies right helps avoid problems. It also makes sure the samples are good for testing.
Sample Handling and Processing
How biopsy samples are handled and processed is very important. This includes:
- Proper Fixation: Using the right fixatives to keep the tissue good.
- Histological Processing: Preparing the tissue for examination.
- Molecular Testing: Doing tests to look at the genetic makeup of the tumor.
Doing these steps right helps get the best possible samples. This makes it easier to examine the tissue and do genetic tests.
Histopathological Examination
The diagnosis of rhabdomyosarcoma heavily relies on histopathological examination. This step involves a detailed analysis of tumor tissue. It’s key to understanding the tumor’s characteristics and planning the right treatment.
Microscopic Features
Rhabdomyosarcoma has unique microscopic features. The cells can look different, from small and round to larger and irregular. The presence of rhabdomyoblasts, with distinct cross-striations, is a key sign of this tumor.
Histological Classification
Rhabdomyosarcoma is divided into subtypes based on its histological features. The main types are embryonal, alveolar, and pleomorphic. Each subtype has unique characteristics that help in diagnosis and treatment. The embryonal subtype is most common in children, while the alveolar subtype often has a worse prognosis.
| Subtype | Histological Features | Prognosis |
| Embryonal | Small, round, blue cells; rhabdomyoblasts | Variable, generally better in children |
| Alveolar | Large, irregular cells; alveolar pattern | Generally worse |
| Pleomorphic | Highly irregular, pleomorphic cells | Poor |
Small-Blue-Round-Cell Tumor Differentiation
Distinguishing rhabdomyosarcoma from other small-blue-round-cell tumors is tricky. Immunohistochemical staining and molecular genetic testing are key in making this distinction. For example, rhabdomyosarcoma usually shows muscle-specific markers like myogenin and MyoD1.
Immunohistochemistry in Rhabdomyosarcoma Diagnosis
Immunohistochemistry is a key tool for diagnosing rhabdomyosarcoma. It uses antibodies to find specific proteins in tissue samples. This helps confirm if a tumor is rhabdomyosarcoma.
Key Markers: Myogenin, MyoD1, and Desmin
Proteins like myogenin, MyoD1, and desmin are used to spot rhabdomyosarcoma cells. Myogenin and MyoD1 are important in muscle cell growth. Desmin is found in muscle cells but is less specific than myogenin or MyoD1.
These markers can show different things in different types of rhabdomyosarcoma. For example, alveolar subtype tumors often have strong myogenin and MyoD1 staining. But, the staining in embryonal subtype tumors can vary.
Interpretation of Immunohistochemical Results
Understanding immunohistochemical results is important. A positive result for myogenin or MyoD1 strongly suggests rhabdomyosarcoma. This is because these markers are very specific for this tumor.
| Marker | Specificity for Rhabdomyosarcoma | Typical Staining Pattern |
| Myogenin | High | Nuclear |
| MyoD1 | High | Nuclear |
| Desmin | Moderate | Cytoplasmic |
Knowing how these markers work is key for accurate diagnosis. The table above shows the main points about these markers in diagnosing rhabdomyosarcoma.
Pathologists use clinical findings, imaging, and immunohistochemistry to diagnose rhabdomyosarcoma. This detailed approach helps create a treatment plan that fits the patient’s needs.
Molecular and Genetic Testing
Advances in molecular and genetic testing are changing how we diagnose and treat rhabdomyosarcoma. These tests give us key information about the tumor’s genetics. This info is vital for making effective treatment plans.
Fusion Gene Detection
Fusion genes, like PAX3-FOXO1 and PAX7-FOXO1, are genetic mistakes that happen when two genes merge. These are common in alveolar rhabdomyosarcoma, a type of the disease. Finding these genes is key for diagnosis and understanding the disease’s outlook.
Tests like fluorescence in situ hybridization (FISH) and reverse transcription polymerase chain reaction (RT-PCR) can spot PAX3-FOXO1 or PAX7-FOXO1 fusion genes. These tests help figure out the rhabdomyosarcoma subtype. Knowing this is important for planning treatment and predicting the disease’s course.
| Fusion Gene | Detection Method | Clinical Significance |
| PAX3-FOXO1 | FISH, RT-PCR | Associated with alveolar rhabdomyosarcoma, often indicates a poorer prognosis |
| PAX7-FOXO1 | FISH, RT-PCR | Also associated with alveolar rhabdomyosarcoma, may have a slightly better prognosis than PAX3-FOXO1 |
Next-Generation Sequencing Applications
Next-generation sequencing (NGS) is a powerful tool for analyzing many genes at once. In rhabdomyosarcoma, NGS can find genetic changes that other tests miss. This info helps tailor treatments to each patient’s genetic makeup.
NGS can also track how well treatments work and find new targets for therapy. Its use in rhabdomyosarcoma is growing, with more applications expected in the future.
Genetic Alterations in Different Subtypes
Different types of rhabdomyosarcoma have unique genetic changes. For example, embryonal rhabdomyosarcoma often has changes in TP53 and MDM2 genes. Alveolar rhabdomyosarcoma, on the other hand, has PAX3-FOXO1 or PAX7-FOXO1 fusion genes.
Knowing these genetic changes is key for creating targeted treatments. Research is ongoing to find new genetic targets and develop therapies that target these changes.
Pediatric Considerations in Rhabdomyosarcoma Detection
Rhabdomyosarcoma is most common in kids and teens. It needs special ways to be diagnosed. Doctors use clinical checks, imaging, and tissue tests, all tailored for kids.
Age-Specific Diagnostic Approaches
Diagnosing rhabdomyosarcoma in kids means knowing the different types. For example, embryonal rhabdomyosarcoma is common in the young. Alveolar rhabdomyosarcoma is more seen in older kids and teens.
When checking a child for rhabdomyosarcoma, age matters. Some tests are better for certain ages. Young kids might need special care for imaging, like sedation. This shows the need for a team that includes experts in pediatric care.
Special Considerations for Children
Children are not just small adults. Their care must be special. Diagnosing rhabdomyosarcoma in kids must think about how it might affect their growth and development.
Pediatric patients need a special approach. This includes using kid-friendly imaging and having pediatric oncologists on the team. It’s also important to think about how treatments might affect their growth and development in the long run.
Challenges and Pitfalls in Rhabdomyosarcoma Diagnosis
Diagnosing rhabdomyosarcoma is tough and can affect patient results. This disease is rare and can show up in many ways, making it hard to diagnose correctly.
There are many reasons why diagnosing rhabdomyosarcoma is hard. It can appear in different parts of the body, each with its own symptoms and challenges. Also, it can look like other diseases, making diagnosis even harder.
Common Diagnostic Errors
There are several ways to make mistakes when diagnosing rhabdomyosarcoma. One big issue is misreading images. For example, radiologists might find it hard to tell rhabdomyosarcoma apart from other soft tissue tumors on MRI or CT scans. To fix this, we suggest:
- Using advanced imaging like PET scans to check metabolic activity.
- Doing whole-body MRI scans to find metastatic disease.
- Improving image reading by working together with different experts.
Another big problem is correctly reading biopsy samples. It takes a lot of skill to tell rhabdomyosarcoma apart from other small-blue-round-cell tumors. We stress the need for:
- Using immunohistochemistry to find key markers like myogenin, MyoD1, and desmin.
- Doing molecular and genetic tests to find specific fusion genes.
- Getting expert pathologists to confirm the diagnosis.
Strategies to Improve Diagnostic Accuracy
To beat the challenges, we support a team effort that includes clinical checks, advanced imaging, and detailed histopathological methods. By using these methods together, we can make diagnoses much more accurate.
Important strategies include:
- Improving imaging with MRI, CT, and PET scans.
- Getting better at biopsies with precise handling and processing.
- Working together among radiologists, pathologists, and doctors for full care.
By following these strategies, we can lower mistakes in diagnosing rhabdomyosarcoma and help patients get better care.
Multidisciplinary Tumor Boards and Consultation
Multidisciplinary tumor boards are key in improving diagnosis and treatment for rhabdomyosarcoma patients. They gather experts like oncologists, radiologists, and surgeons. Together, they review cases and create detailed care plans.
Role of Expert Review
Expert review is vital in these boards. Experts examine images, slides, and data to lower diagnostic errors. A leading oncologist says, “Collaboration among specialists is key to providing the best possible outcomes for patients with complex cancers like rhabdomyosarcoma.”
The benefits of expert review include:
- Enhanced diagnostic accuracy through collective expertise
- Development of personalized treatment plans tailored to individual patient needs
- Access to cutting-edge treatments and clinical trials
Second Opinion Considerations
Getting a second opinion is key for rhabdomyosarcoma patients. It can offer new insights and treatment options. A patient advocacy group notes, “A second opinion can be a critical step in ensuring that patients receive the most appropriate care for their specific condition.”
When looking for a second opinion, patients should seek:
- Centers of excellence with experience in treating rhabdomyosarcoma
- Specialists with expertise in sarcoma and pediatric oncology
- Comprehensive review of all diagnostic materials and clinical data
By using multidisciplinary tumor boards and expert consultation, we can better diagnose and treat rhabdomyosarcoma. This teamwork is essential for top-notch care for this complex disease.
Conclusion: Ensuring Accurate and Timely Diagnosis
Finding rhabdomyosarcoma needs a detailed plan. This includes knowing its signs, using the right tests, and getting a correct diagnosis fast. We’ve covered how to spot rhabdomyosarcoma, from first checks to detailed scans and tissue tests.
Getting the diagnosis right is key for good treatment and better health for patients. A team effort, with experts working together, is vital for handling this tough disease. Catching rhabdomyosarcoma early is also key to success, making quick diagnosis very important.
Knowing how vital accurate and fast diagnosis is, we can help patients get better. We stress the need for teamwork among doctors to give patients the best care.
FAQ
What are the common signs and symptoms of rhabdomyosarcoma?
Signs include swelling or masses, pain, and trouble swallowing. Other symptoms are fever and weight loss.
How is rhabdomyosarcoma diagnosed?
Doctors use MRI, CT scans, and ultrasound to find tumors. They then take a biopsy and examine it under a microscope.
What is the role of imaging in detecting rhabdomyosarcoma?
Imaging helps find and understand tumors. It also checks how well treatment is working.
What are the different types of biopsies used to diagnose rhabdomyosarcoma?
There are fine-needle, core needle, and surgical biopsies. Each is chosen based on the situation to get an accurate diagnosis.
How is histopathological examination used in rhabdomyosarcoma diagnosis?
It looks at the tumor’s microscopic features. This helps doctors tell rhabdomyosarcoma apart from other tumors.
What is the significance of immunohistochemistry in rhabdomyosarcoma diagnosis?
It uses markers like myogenin to confirm rhabdomyosarcoma. This helps doctors make the right diagnosis.
How is molecular and genetic testing used in rhabdomyosarcoma diagnosis?
Tests look for genetic changes specific to rhabdomyosarcoma. This helps in diagnosis and planning treatment.
What are the challenges in diagnosing rhabdomyosarcoma in children?
Diagnosing in kids requires special approaches. The disease can show up differently in children.
How can diagnostic accuracy be improved in rhabdomyosarcoma?
Using advanced techniques and teamwork helps. Getting second opinions is also important.
What is the role of multidisciplinary tumor boards in rhabdomyosarcoma diagnosis?
Tumor boards ensure accurate diagnosis and treatment. They bring together experts for case review and guidance.
When should I seek medical attention for suspected rhabdomyosarcoma?
See a doctor right away for severe pain, swallowing trouble, or other signs. Risk factors like family history also matter.
What are the benefits of PET scans in rhabdomyosarcoma diagnosis?
PET scans show tumor activity and detect spread. They help in planning treatment and checking its success.
References:
- Skapek, S. X., Ferrari, A., Gupta, A. A., Lupo, P. J., Butler, E., Shipley, J., & Barr, F. G. (2019). Rhabdomyosarcoma. Nature Reviews Disease Primers, 5(1), 1–19. Retrieved from https://www.nature.com/articles/s41572-018-0051-2
- Linardic, C. M. (2008). Raas pathways in rhabdomyosarcoma: Targets and therapeutic prospects. Sarcoma, 2008, Article 956285. Retrieved from https://pubmed.ncbi.nlm.nih.gov/18437259/