Last Updated on November 20, 2025 by Ugurkan Demir
At Liv Hospital, we know how complex Acute Lymphoblastic Leukemia (ALL) is. It’s a cancer that affects the blood and bone marrow. It’s the most common cancer in kids, making up about 25% of all childhood cancers in the U.S. Discover risk factors for all, including genetic and environmental contributors to acute lymphoblastic leukemia.
We believe knowing what causes ALL is key to treating it early and well. Our focus on patient care and advanced medicine means we give the best treatment for leukemia.
It’s important to know about Acute Lymphoblastic Leukemia (ALL) to understand its causes and risk factors. We’ll explore what this condition is, how common it is, and why knowing its risk factors is key.
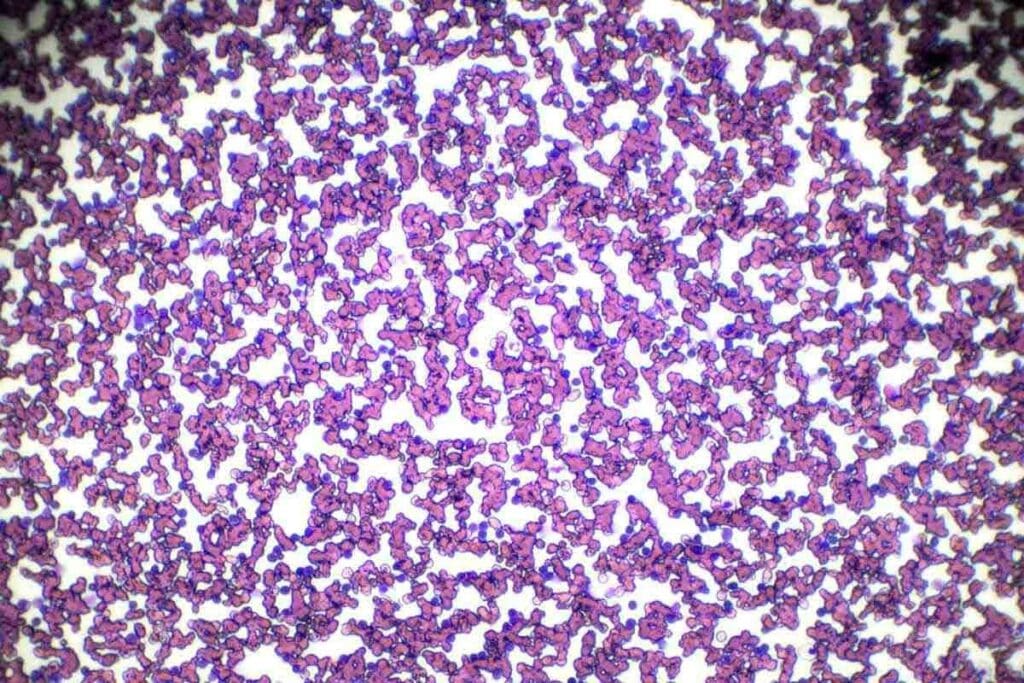
ALL happens when the bone marrow makes too many stem cells. These cells turn into lymphoblasts, which are not fully developed white blood cells. They don’t grow into B or T lymphocytes, causing a buildup of leukemia cells.
This buildup stops the bone marrow from making normal blood cells. This leads to health problems.
ALL is the top cancer in kids, but it can also hit adults. Its occurrence changes with age and other factors. Kids under 5 face the biggest risk, with boys slightly more likely to get it than girls.
Some genetic conditions, like Down syndrome, raise the risk of ALL.
Finding out who’s at risk for ALL is vital for catching it early. While we don’t always know why ALL happens, knowing the risk factors helps. These can include genetic issues, exposure to harmful chemicals, and past radiation therapy.
Knowing these factors helps in creating ways to prevent it and tailor treatments.

Acute Lymphoblastic Leukemia (ALL) is linked to genetic predispositions and inherited disorders. Knowing these genetic factors is key. It helps identify those at higher risk and guides treatment choices.
Down syndrome, caused by an extra chromosome 21, raises the risk of ALL. Kids with Down syndrome are 20-30 times more likely to get ALL than others.
Other genetic syndromes also increase the risk of ALL. These include:
These syndromes have genetic instability. This instability can lead to a higher risk of leukemia.
| Genetic Syndrome | ALL Risk Increase | Characteristics |
| Down Syndrome | 20-30 times | Extra copy of chromosome 21 |
| Bloom Syndrome | High | Genomic instability, short stature |
| Fanconi Anemia | High | Congenital abnormalities, bone marrow failure |
| Neurofibromatosis Type 1 | Moderate | Multiple neurofibromas, café-au-lait spots |
| Ataxia-Telangiectasia | High | Progressive ataxia, telangiectasias |
Knowing how these genetic syndromes relate to ALL risk is important. It helps in early detection and management of the disease.
Ionizing radiation is linked to a higher risk of blood cancer, like ALL. Being exposed to it, or to chemotherapy, during childhood increases this risk. We’ll look at how radiation exposure affects the risk of ALL, focusing on ionizing, medical, and environmental sources.
Ionizing radiation has enough energy to remove tightly bound electrons from atoms. This creates ions. Types of ionizing radiation include X-rays, gamma rays, and some ultraviolet light. High levels of this radiation can cause genetic mutations that lead to leukemia.
Key effects of ionizing radiation include:
Medical radiation, from procedures like CT scans and radiation therapy, adds to our total radiation dose. While these procedures are often necessary, it’s important to reduce exposure when possible.
Some key points about medical radiation exposure include:
Environmental radiation sources include cosmic rays, radon gas, and radiation from industrial or nuclear accidents. Everyone is exposed to background radiation daily. But, some groups face higher risks due to their environment or job.
Notable environmental radiation sources include:
Knowing about radiation sources and risks helps us develop ways to reduce exposure. This protects public health.
Chemotherapy is a lifesaver but can also raise the risk of secondary Acute Lymphoblastic Leukemia (ALL) in some patients. This risk is linked to specific types of chemotherapy agents.
Research has found certain chemotherapy drugs that increase the risk of secondary leukemias, including ALL. These include:
These drugs damage DNA, which can cause leukemia. The risk grows with higher doses and longer exposure.
The time between chemotherapy and secondary ALL can vary. Studies show:
It’s important to keep an eye on patients who have had chemotherapy, even those treated as kids.
Secondary leukemias, including ALL, are a known side effect of chemotherapy. They happen due to genetic mutations from the drugs. Early detection and monitoring are critical for managing this risk.
Improving cancer treatment while understanding secondary leukemia risks is key. Finding the right balance between treatment benefits and long-term risks is a big challenge in oncology.
A study in a top medical journal said, “The risk of secondary leukemia after chemotherapy is a significant concern, necessitating careful patient monitoring and follow-up.”
“The development of secondary leukemia after chemotherapy is a complex process involving multiple genetic and environmental factors.”
By knowing these risks and keeping a close eye on patients, we can try to lower the number of secondary ALL cases.
Exposure to environmental toxins and industrial pollutants is a big risk for Acute Lymphoblastic Leukemia (ALL). We find that some chemicals and pollutants are key in causing this disease.
Benzene is known to increase the risk of ALL. Occupational exposure to benzene in industries like petroleum and chemical manufacturing is linked to leukemia. Other chemicals, like solvents and pesticides, might also cause ALL, but more research is needed.
These chemicals harm our bodies in different ways. Benzene, for instance, damages the bone marrow, causing genetic mutations that can lead to leukemia. Knowing how these chemicals work is key to preventing and treating the disease.
Pesticides and agricultural chemicals are also linked to an increased risk of ALL. Epidemiological studies show that exposure to these chemicals, often in rural areas or through work in agriculture, may lead to leukemia.
The ways pesticides affect ALL risk are complex. But, it’s thought that they can cause genetic damage and disrupt cell function, leading to leukemia.
Living near industrial sites is a risk factor for ALL. Communities near industrial areas face exposure to chemicals and toxins, including benzene and carcinogens, through pollution in the air and water.
Studies show that people living near industrial sites face a higher risk of ALL. This underlines the need for stricter rules on industrial emissions and better protection for nearby communities.
Pediatric ALL is a complex condition influenced by multiple risk factors. These include age, sex, and race. Understanding these factors is key to identifying children at higher risk. It also helps in developing targeted interventions.
Age is a significant risk factor for ALL in children. The incidence of ALL peaks between the ages of 1 and 4 years. This makes it the most common cancer in young children.
After this peak, the incidence declines. There is a slight increase again in adults over 50 years old.
Table: Age Distribution of ALL Incidence
| Age Group | Incidence Rate |
| 1-4 years | High |
| 5-9 years | Moderate |
| 10-14 years | Low |
| 50+ years | Moderate to High |
Sex differences are another critical aspect of ALL epidemiology. Research shows that boys are slightly more likely to develop ALL than girls. The reasons for this disparity are not entirely clear.
Further studies are needed to understand the underlying causes of this sex difference.
Race and ethnicity also play a role in the incidence of ALL. Studies have shown that children of European descent have a higher incidence of ALL. This is compared to children of African descent.
Understanding these racial and ethnic differences can provide insights into genetic and environmental factors contributing to ALL.
By examining the interplay of age, sex, and race/ethnicity, we can better understand the risk factors for ALL in children. This knowledge helps in developing more effective prevention and treatment strategies.
Parental age and reproductive history are key in understanding Acute Lymphoblastic Leukemia (ALL) risk. Research shows a complex link between genetics and environment. This includes the role of parental age and reproductive history.
Advanced parental age, over 40, is linked to ALL. Studies show older parents might have a higher risk of having a child with ALL. “The association between advanced paternal age and the risk of ALL in offspring has been observed in several epidemiological studies,” highlighting the need for further research into the underlying mechanisms.
According to a study published in a reputable medical journal,
“Advanced paternal age was associated with an increased risk of ALL, suggesting that genetic mutations in older fathers may contribute to leukemogenesis.”
This finding shows why paternal age is a risk factor.
Maternal reproductive history is also linked to ALL risk. Factors like the mother’s age at menarche, parity, and history of miscarriages or fetal losses are studied. These factors might affect ALL risk.
Prenatal exposures, like maternal exposure to toxins or infections, are studied for their role in ALL. Maternal nutrition and health during pregnancy are critical. They may influence fetal development and ALL risk.
Research on prenatal exposures and ALL risk is ongoing. Some studies suggest maternal infection during pregnancy may increase ALL risk in children. More research is needed to understand these associations.
Research shows that birth characteristics and early life factors might affect Acute Lymphoblastic Leukemia (ALL) development.
Looking into these factors helps us understand the risks and how ALL starts. We’ll focus on high birth weight, birth order, and early childhood development.
Studies link high birth weight to a higher risk of ALL. This means that how a baby grows might affect leukemia risk.
The birth order of a child might also play a role in ALL risk. Being the firstborn or having a higher birth order could slightly increase risk. But, not all studies agree on this.
Early childhood development includes many factors. These include infections, vaccinations, and health during the early years. Research looks into how these might shape the immune system and affect ALL risk.
By studying birth characteristics and early life factors, we gain insights into the complex mix of genetics and environment in ALL development.
Certain viral infections can harm the immune system, raising the risk of Acute Lymphoblastic Leukemia (ALL). We will look into how these infections and immune system factors lead to ALL.
Research shows some viruses increase the risk of ALL. For example, the human T-cell lymphoma/leukemia virus-1 (HTLV-1) causes certain leukemias. Knowing these viral links is key to spotting higher risk groups.
Other viruses, like Epstein-Barr Virus (EBV), are linked to lymphoproliferative disorders. This suggests they might play a part in ALL’s development. We’ll dive into how these viruses might lead to leukemia.
The immune system fights off infections and cancers. But, some viral infections can weaken it, raising ALL risk. Immune problems can come from long-term infections or how the immune system reacts to viruses.
We’ll explore how immune system issues, caused by viruses or other factors, might lead to ALL. This includes looking at the role of immune cells and their interactions with viruses.
Early childhood is key for the immune system’s growth. Infections during this time can greatly affect immune system development. Infection patterns in early childhood might affect ALL risk.
We’ll discuss how early childhood infections might be linked to ALL risk. This includes looking at the hygiene hypothesis and its effects on immune system development.
Whether ALL leukemia is hereditary is a complex issue. Most ALL cases aren’t caused by genes, but some are. Family patterns and genetic predispositions can influence these cases.
Studies have found that having a close relative with ALL or leukemia slightly raises your risk. But the risk is not very high.
Key Findings on Familial ALL:
Understanding the causes of ALL involves looking at both genes and environment. Genes are important, but so are environmental factors.
| Factor | Genetic Influence | Environmental Influence |
| ALL Risk | Genetic syndromes (e.g., Down Syndrome) | Exposure to ionizing radiation |
| Familial Patterns | Inherited genetic mutations | Shared environmental exposures |
When assessing risk for family members, both genes and environment matter. For most, the risk is low. But, for those with a strong family history, screening might be advised.
It’s essential for families to discuss their specific situation with healthcare providers to understand their risks and the appropriate steps to take.
Research into Acute Lymphoblastic Leukemia (ALL) is growing. New risk factors are being studied. This helps us understand how to prevent and treat ALL better.
Some studies look at if electromagnetic fields (EMF) increase ALL risk. EMF comes from many things like power lines and phones. Some research suggests a link, but it’s not clear yet.
More research is needed. We need to know how EMF might affect ALL risk. This will help us understand better.
Diet might play a role in ALL. Eating lots of fruits and veggies might lower risk. But eating too much processed meat might raise it.
Nutrition during pregnancy and early childhood is key. For example, folate in pregnancy might protect against ALL in kids.
| Dietary Factor | Potential Effect on ALL Risk |
| High intake of fruits and vegetables | Reduced risk |
| High consumption of processed meats | Increased risk |
| Folate intake during pregnancy | Potential protective effect |
Socioeconomic status (SES) and healthcare access are also being studied. Kids from wealthier families might be more likely to get ALL. This could be because they don’t get exposed to infections early on.
Getting diagnosed with ALL can be affected by healthcare access. Those with less access might get diagnosed later. This can affect treatment outcomes.
Studying these risk factors is important. It helps us understand ALL better. This knowledge can lead to better prevention and early detection.
It’s key to know the risks of Acute Lymphoblastic Leukemia (ALL) to prevent and treat it well. Healthcare providers can tailor care by understanding genetic, environmental, and demographic factors. This helps in giving each patient the right care.
At Liv Hospital, we use the newest methods and team care to fight ALL. We aim to give top-notch healthcare, including support for international patients. By tackling ALL risk, we aim to better patient outcomes and life quality.
Handling ALL risk means spotting risk factors early, diagnosing fast, and treating right. We focus on personalized care for each patient. This ensures they get the best treatment for ALL.
Acute Lymphoblastic Leukemia (ALL) is a blood and bone marrow cancer. It happens when there’s too many immature white blood cells.
Risk factors for ALL include genetic predisposition and radiation exposure. Also, previous chemotherapy, environmental toxins, and viral infections play a role.
ALL is not strictly hereditary. While genetics can play a part, environmental factors also contribute to the risk.
People with Down syndrome are at higher risk for ALL. This is likely due to genetic factors linked to the condition.
Yes, high levels of ionizing radiation can increase the risk of ALL.
Certain chemotherapy treatments can raise the risk of ALL. This often happens after a certain period of time.
Exposure to toxins like benzene and pesticides can increase the risk of ALL.
Yes, children are more at risk for ALL. Some age groups and demographics are more affected than others.
Advanced parental age and certain maternal reproductive factors may increase the risk of ALL in children.
High birth weight and certain early childhood patterns may raise the risk of ALL.
Yes, viral infections that affect the immune system may increase the risk of ALL.
Socioeconomic status can impact healthcare access. It may affect the risk and outcomes of ALL, mainly in certain groups.
The link between electromagnetic field exposure and ALL risk is not clear. The evidence is emerging and controversial.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!