
At Liv Hospital, we know that dealing with chronic pain needs a full plan. Radiofrequency ablation (RFA) is a small procedure that might help with long-term back pain.
Explore the risk of burning nerves in lower back during radiofrequency ablation, pros, and cons.
RFA aims to stop pain signals by targeting certain nerves. It’s a method that could work, but it’s important to look at both sides. Our team is here to help you decide what’s best for you.
Thinking about RFA? It’s key to know its good points and not-so-good points. By looking at the pros and cons of nerve burning, you can choose wisely.
Key Takeaways
- Radiofrequency ablation is a minimally invasive procedure for managing chronic lower back pain.
- RFA targets specific nerve endings to disrupt pain signals to the brain.
- Understanding the pros and cons of RFA is key for making a smart choice.
- Liv Hospital’s experts offer personalized advice during treatment.
- RFA might be a good option for those with chronic pain.
What is Radiofrequency Ablation?
Radiofrequency ablation is a medical procedure that helps manage chronic pain. It uses high-frequency electrical currents to heat up a specific area, usually a nerve. This heat disrupts pain signals sent to the brain.
Definition and Basic Procedure
Radiofrequency ablation (RFA) is a minimally invasive method. It uses electrical currents to generate heat around a targeted nerve. This heat damages the nerve, stopping it from sending pain signals to the brain.
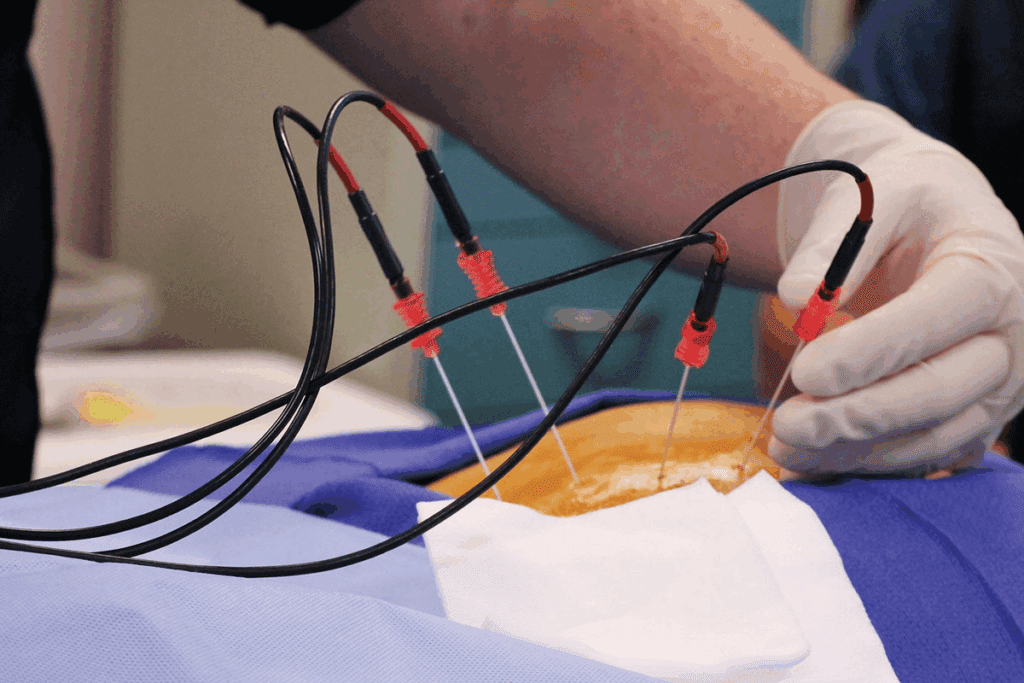
The procedure involves a specialized needle or electrode. It is guided to the targeted area using imaging technologies like fluoroscopy or CT scans.
The basic steps of the RFA procedure include:
- Preparation: The patient is positioned on an examination table, and the skin is cleaned and sterilized.
- Anesthesia: Local anesthesia is administered to numb the area where the needle will be inserted.
- Needle Placement: A needle or electrode is carefully guided to the targeted nerve under imaging guidance.
- Ablation: The radiofrequency energy is applied to heat the nerve, creating a lesion that disrupts pain signal transmission.
History and Development of RFA
The idea of using heat to ablate nerves for pain relief has been around for decades. Early versions of this technique were developed in the 1970s and 1980s. These early methods were not very precise.
Over time, technology has improved RFA. Today, it is a precise and effective treatment for chronic pain. It is used for conditions like facet joint pain and certain types of lower back pain.
| Year | Development |
| 1970s | Initial development of nerve ablation techniques |
| 1980s | Introduction of radiofrequency energy for nerve ablation |
| 2000s | Advancements in imaging guidance and needle design |
As we learn more about RFA, it’s important to consider if it’s right for each patient. The success of RFA depends on the condition being treated and the patient’s health.
How Radiofrequency Ablation Works
Understanding RFA is key for those thinking about it for chronic pain. This treatment uses electrical currents to heat up nerves. This heat stops pain signals from reaching the brain.
The Science Behind Nerve Burning
RFA works by making a lesion on nerve tissue. When radiofrequency energy is applied, it creates a controlled heat lesion. This interrupts pain signals to the brain, giving relief.
The process involves several key steps:
- Insertion of a specialized needle or electrode near the targeted nerve under imaging guidance.
- Administration of local anesthesia to minimize discomfort.
- Application of radiofrequency energy to generate heat around the nerve.
- Creation of a lesion on the nerve tissue, disrupting pain signal transmission.
Types of RFA Procedures
There are many RFA procedures, each for different pain conditions. The main difference is in the technique and the body area treated.
| Type of RFA | Description | Common Applications |
| Conventional RFA | Uses continuous radiofrequency energy to create a lesion. | Facet joint pain, sacroiliac joint pain. |
| Pulsed RFA | Applies intermittent radiofrequency energy, potentially reducing nerve damage risk. | Chronic pain conditions where nerve preservation is desired. |
| Cooled RFA | Utilizes a cooled electrode to create larger lesions. | More extensive pain areas, such as larger facet joints. |
Each RFA procedure has its own use and benefits. The choice depends on the patient’s condition and the doctor’s judgment.
Common Conditions Treated with RFA
Radiofrequency Ablation (RFA) is a key treatment for many spinal issues. It helps those with chronic pain who haven’t seen results from other treatments.
Facet Joint Pain
Facet joint pain is a common issue treated with RFA. These small joints help stabilize the spine. When they get inflamed, it can cause a lot of pain.
RFA can effectively reduce facet joint pain by blocking the pain signals from these joints.
“RFA is a game-changer for patients with facet joint pain who have not found relief with other treatments,” says Medical Expert, a leading pain management specialist. “By targeting the specific nerves responsible for pain transmission, we can significantly improve the quality of life for these patients.”
Other Spinal Conditions
RFA is also used for sacroiliac joint pain and some types of chronic lower back pain. Its ability to treat various conditions makes it a good choice for many patients.
We consider RFA for those with chronic spinal pain after thorough tests. This helps us see if RFA is right for them.
It’s important to know RFA’s benefits and possible downsides. These include temporary relief and side effects. We talk about these with our patients to help them make informed choices.
The Procedure: What to Expect
Understanding the RFA procedure is key. Knowing what happens before, during, and after can ease worries. It prepares people for what’s to come.
Before the Procedure
First, patients get checked to see if they’re right for RFA. This includes looking at their health history and doing tests. It’s important to tell your doctor about any medicines you’re taking, like blood thinners.
Before the procedure, you might be told to:
- Stop taking certain medicines that could affect the procedure or recovery
- Not eat or drink for a while before the procedure
- Have someone drive you home after it’s done
During the Procedure
The RFA procedure uses fluoroscopy to guide a needle to the right nerve. Fluoroscopy helps place the needle exactly, making the treatment more effective. After the needle is in, a local anesthetic numbs the area. Then, the RFA is done.
A doctor said, “RFA’s precision, thanks to fluoroscopy, makes it a great choice for chronic pain.” This shows how important it is to place the needle correctly.
After the Procedure
Right after RFA, patients are watched for any quick problems. Some might feel pain or soreness where the needle was, but this can be helped with over-the-counter pain meds. It’s common to feel numb or weak in the treated area, but this usually goes away by itself.
To recover well, patients should:
- Rest for the rest of the day
- Avoid hard activities for a few days
- Follow any special instructions from their doctor
The full effects of RFA might not show right away. It can take weeks for the treated nerve to fully respond.
5 Key Benefits of Radiofrequency Ablation
Radiofrequency ablation is becoming more popular for pain management. It offers many benefits, including effective pain relief. This makes it a top choice for those with chronic pain.
Effective Pain Relief
RFA is great at providing effective pain relief. It targets specific nerves that carry pain. This can greatly reduce or even stop chronic pain for many patients.
“Radiofrequency ablation has been a game-changer for my patients with chronic pain,” says a leading pain management specialist. “It’s a highly effective treatment that can greatly improve their quality of life.”
Minimally Invasive Nature
RFA is a minimally invasive procedure. It only needs a small cut and doesn’t harm much of the surrounding tissue. This lowers the chance of complications and speeds up healing compared to bigger surgeries.
Reduced Medication Dependency
RFA can help patients need less pain medication. This is very important during the opioid crisis. It gives a non-drug way to manage chronic pain.
Quick Recovery Time
Patients usually get better fast after RFA. They can get back to their usual activities quickly. This is a big plus compared to longer recovery times from more invasive surgeries.
In summary, radiofrequency ablation is a great choice for chronic pain. It’s effective, minimally invasive, can lower medication use, and has a quick recovery. These reasons make it very popular in pain management.
5 Major Drawbacks and Risk of Burning Nerves in Lower Back
Radiofrequency Ablation (RFA) can help with chronic back pain. But, it’s important to know its limits. It’s a procedure that offers relief but also has its own set of risks and drawbacks.
Temporary Nature of Relief
RFA’s pain relief is often short-lived. Studies show it can last from 6 to 12 months. This means patients might need more treatments to keep feeling better.
| Duration of Relief | Percentage of Patients |
| Less than 6 months | 20% |
| 6-12 months | 50% |
| More than 1 year | 30% |
Muscle Weakness Concerns
RFA can also lead to muscle weakness. This happens because nerves are ablated, affecting nearby muscles. This is a big worry for those who need these muscles for daily tasks.
Muscle weakness can make daily life harder. But, in many cases, it’s temporary and goes away by itself.
Increased Risk of Disc Degeneration
RFA might also raise the risk of disc degeneration. By easing pain, it can make the spine more mobile. This extra movement can stress the spinal discs over time.
Potential for Neuropathic Pain
Lastly, RFA can lead to neuropathic pain. This pain comes from nerve damage and is hard to treat. It’s a big worry because it can be worse than the original pain.
In summary, RFA can help with chronic back pain but has its downsides. These include temporary relief, muscle weakness, increased disc degeneration risk, and neuropathic pain. It’s key for patients to know these risks.
Potential Side Effects and Complications
Radiofrequency Ablation (RFA) is a top choice for chronic pain relief. Yet, it’s key to know the possible side effects and complications. Knowing these can help patients make better choices about their health.
Common Side Effects
Most people who get RFA face some side effects, but they’re usually mild and short-lived. Common issues include:
- Pain Flare: Some might feel more pain right after, but it usually goes away in a few days.
- Bruising: Minor bruising at the needle site is common and usually heals on its own.
- Temporary Numbness: Numbness or feeling different in the treated area can happen but is usually short-term.
Dealing with these side effects is often easy. Applying ice to reduce swelling or taking over-the-counter pain meds can help. Most of the time, these effects don’t last long and don’t get in the way of daily life.
Rare but Serious Complications
While rare, serious problems can happen with RFA. These include:
- Infection: As with any invasive procedure, there’s a risk of infection, which can be treated with antibiotics if caught early.
- Nerve Damage: Though RFA aims for specific nerves, there’s a small chance of damaging nearby nerves, leading to new or worse pain.
- Burning Sensation: Some might feel a burning sensation, which is usually temporary but can last longer in rare cases.
It’s vital for patients to know about these possible complications and talk to their healthcare provider about any worries. Understanding the risks and benefits helps in deciding if RFA is right for them.
By knowing the possible side effects and complications of RFA, patients can make better choices about their treatment. They can also work closely with their healthcare providers to handle any problems that come up.
Recovery and Long-term Outcomes
When you think about RFA for pain management, recovery and long-term effects are important. We’ll help you know what to expect after the treatment.
Typical Recovery Timeline
Most people can get back to normal in a few days after RFA. But, how fast you recover depends on several things. These include the area treated and your overall health.
Here’s what you might go through during recovery:
- You might feel some mild pain or discomfort, which can be eased with over-the-counter meds.
- You could also feel numbness or tingling, but these usually go away by themselves.
- You’ll need to see your doctor again to check how well the treatment worked and to talk about any issues.
Managing Expectations
It’s key to have the right expectations for RFA to work well. While it can help a lot with pain, it’s not a promise against all future pain. How well it works depends on several things. These include the condition being treated, how accurate the procedure was, and your own health.
To get a better idea of what to expect long-term, look at this table:
| Outcome | Short-term (0-3 months) | Long-term (6-12 months) |
| Pain Relief | Most people see a big drop in pain | Results vary; some keep feeling better, others might see pain come back |
| Activity Level | You’ll start to get back to normal activities slowly | Most people stay active or even get more active |
| Medication Use | You might need less pain meds | Many people keep needing less pain meds |
Knowing these things helps you set realistic goals and make smart choices about your care.
Facet Joint Ablation: Specific Considerations
Facet joint ablation is a medical procedure that helps manage facet joint pain. It has become popular in the medical world. This is because it offers hope to those with chronic pain from facet joints.
Facet joint pain affects many people, making their lives harder. It happens when the facet joints in the spine get inflamed or irritated. This can be due to arthritis, injury, or wear and tear. The goal of facet joint ablation is to block pain signals from these joints.
Success Rates for Facet Joint Pain
Research shows that facet joint ablation can be very effective. The success depends on several things. These include how accurate the diagnosis is, the skill of the doctor, and the method used.
- High Success Rates: Many people find a lot of relief from their pain after the procedure.
- Variable Outcomes: Results can differ based on the patient and the procedure details.
- Long-term Relief: Some people may feel pain-free for a long time, but it varies.
Unique Risks and Benefits
Facet joint ablation has its own set of risks and benefits. It’s important for patients to know these before deciding on the treatment.
Benefits:
- It’s a minimally invasive procedure, which means less recovery time.
- It can offer significant and lasting pain relief.
- It may help reduce the need for pain medication.
Risks:
- There might be temporary discomfort or pain at the site of the procedure.
- There’s a small chance of nerve damage or other complications.
- The pain might come back over time.
In summary, facet joint ablation is a promising treatment for facet joint pain. While it has risks, the benefits make it a good option for many. It’s important for patients to talk to their doctor about their situation and what they hope to achieve.
Burning Nerves in the Neck vs. Lower Back
When we talk about radiofrequency ablation, knowing the difference between the neck and lower back is key. These areas have different structures, which changes how RFA works.
Anatomical Differences
The neck has a complex network of nerves that control many body functions. The lower back, on the other hand, carries a lot of weight and stress. This means RFA needs different methods for each area.
“The cervical spine is more mobile and has a different curvature compared to the lumbar spine,” notes a study on spinal anatomy.
“This difference in mobility and structure affects how RFA is applied and its efficacy in treating pain.”
Outcome Variations
RFA results can vary between the neck and lower back. This is because of the anatomy and the specific pain issues. For example, treating neck facet joint pain requires more precise nerve targeting.
In the lower back, RFA is used for facet joint pain and other lumbar spine issues. The success and how long pain relief lasts can change based on the anatomy and condition. Knowing these differences helps manage patient hopes and achieve better results.
When using RFA in different spinal areas, a customized approach is essential. By understanding the unique features of the neck and lower back, doctors can provide better care.
Patient Selection: Who Should Consider RFA?
Finding the right patients for RFA is key to its success. We look at each patient’s health to see if RFA is a good fit.
Ideal Candidates
People with chronic pain that hasn’t gotten better with other treatments are good candidates. This includes those with facet joint pain or other spinal issues. We also check their overall health, including any other health problems.
Those who have had a successful diagnostic block are likely to benefit from RFA. It’s also important for patients to understand what the procedure can do. This helps them make better choices about their treatment.
Contraindications
Not everyone is a good fit for RFA. This includes those with active infections, bleeding disorders, and severe psychological conditions. These can make it hard for the patient to follow instructions during the procedure.
People with pacemakers or other implanted electrical devices need extra care. RFA might affect these devices. We also check if the patient’s body is suitable for the procedure.
It’s important to know the downsides of nerve ablation. While it’s usually safe, it’s not a guarantee of long-term pain relief. We talk to our patients about these risks to set realistic expectations.
Conclusion: Is Radiofrequency Ablation Right for You?
As we wrap up our talk on Radiofrequency Ablation (RFA), it’s key to think if it’s right for you. We’ve looked at the good and bad sides of RFA. This includes how well it works for chronic pain, its easy procedure, and possible dangers.
Think about your health and how bad your symptoms are. Weigh the good and bad of spinal nerve ablation. This helps you decide based on your health history and what RFA could do for you.
Talk to your doctor about if RFA might work for you. Knowing the possible results and risks helps you decide if it’s the best choice. So, is it worth it for you? It really depends on your situation and how you react to the treatment.
In the end, RFA could be a good choice for chronic pain. By thinking about your options and talking to a doctor, you can decide if RFA is right for you.
FAQ
What is Radiofrequency Ablation (RFA) and how does it work?
Radiofrequency Ablation is a procedure that uses heat to treat pain. It works by burning the nerve endings. This stops pain signals from reaching the brain. We use it to help with chronic pain, like what happens in the facet joints.
What are the benefits of Radiofrequency Ablation?
RFA offers many benefits. It can greatly reduce pain, is less invasive, and doesn’t rely on medication. Plus, recovery is quick. Many patients see a big improvement in their life after RFA.
What are the possible downsides of Radiofrequency Ablation?
While RFA is safe, there are some downsides. Relief might not last forever, and there’s a chance of muscle weakness. There’s also a risk of disc problems and neuropathic pain. We do our best to minimize these risks for each patient.
What is the difference between burning nerves in the neck and lower back?
The main difference is where the nerves are and which ones we target. We consider each area’s unique needs for the best results.
What are the common side effects of Radiofrequency Ablation?
Side effects include pain, bruising, and numbness. We watch over patients closely to manage these. If you need to see a doctor, we’ll tell you when.
Are nerve ablations worth it?
For many, RFA is a good choice. It can greatly reduce pain and improve life quality. We carefully decide if RFA is right for each patient.
What is the recovery time for Radiofrequency Ablation?
Recovery times vary, but most can get back to normal in a few days to a week. We help each patient understand what to expect and how to recover.
Can Radiofrequency Ablation be used to treat facet joint pain?
Yes, RFA is often used for facet joint pain. We’ve seen it work well for many patients, giving them long-term relief.
Who is a good candidate for Radiofrequency Ablation?
Good candidates have chronic pain that hasn’t gotten better with other treatments. We look at each patient’s health and condition to see if RFA is right.
Are there any contraindications for Radiofrequency Ablation?
Yes, some conditions like bleeding disorders or infections might not be good for RFA. We check each patient’s health to see if RFA is safe for them.
What are the risks associated with burning nerves in the lower back?
Risks include muscle weakness, disc problems, and neuropathic pain. We work hard to avoid these and ensure the best results.
How long does the pain relief from Radiofrequency Ablation last?
Relief can last months to a year or more. We help patients understand what to expect and plan for future treatments if needed.
References
National Center for Biotechnology Information. (2025). 5 Key Pros and Cons of Burning Nerves. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34609551/
Facchini, G., Spinnato, P., Guglielmi, G., Albisinni, U., & Bazzocchi, A. (2017). A comprehensive review of pulsed radiofrequency in the treatment of pain associated with different spinal conditions. BMC Musculoskeletal Disorders, 18, 287. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5605093/






