For many, IVF (In Vitro Fertilization) is a ray of hope for starting a family. But, it can face a hurdle with ectopic pregnancy. This is when the embryo grows outside the uterus. It’s a worry for 1.4 to 5.4 percent of IVF cycles.
An ectopic pregnancy isn’t inherited through genes—it usually happens due to medical factors like damaged fallopian tubes or hormonal imbalances. Understanding these causes helps in finding effective prevention methods. At Liv Hospital, we provide full support to IVF patients and work to minimize the risk of ectopic with IVF through careful monitoring and personalized treatment plans.
Key Takeaways
- Ectopic pregnancy affects 1.4 to 5.4 percent of IVF cycles.
- Understanding the causes of ectopic pregnancy is key to preventing it.
- Medical factors play a big role in the risk of ectopic pregnancy.
- Proven methods can help reduce the risk of ectopic pregnancy.
- Comprehensive care and support are vital for IVF patients.
Understanding Ectopic Pregnancy in IVF Treatment
Ectopic pregnancy is a risk with IVF treatment. It’s when a fertilized egg implants outside the uterus. We’ll look into what causes it and how it’s defined.
What is an Ectopic Pregnancy?
An ectopic pregnancy happens when a fertilized egg implants outside the uterus. This usually occurs in a fallopian tube. But it can also happen in the ovary, cervix, or abdominal cavity. American Society for Reproductive Medicine (ASRM) says it’s a big worry with IVF.
Symptoms can be like a normal pregnancy, like missed periods and nausea. But they can also include severe pain and vaginal bleeding. Women going through IVF should know these signs and get help right away if they happen.
Why Does an Ectopic Pregnancy Happen?
Ectopic pregnancies aren’t passed down in families. They’re caused by problems in the reproductive system. Damage to the fallopian tubes, from surgery or infection, can raise the risk. IVF’s embryo transfer process might also play a part, but it’s not fully understood.
“The exact cause of ectopic pregnancy is often multifactorial, involving a combination of factors that affect the normal implantation process.” –
Reproductive Medicine Expert
Several things can make a woman more likely to have an ectopic pregnancy. These include:
- Having had an ectopic pregnancy before
- Fallopian tube damage or surgery
- Pelvic infections like PID
- Endometriosis
- Previous pelvic surgery
Risk Factor | Description | Impact on Ectopic Pregnancy Risk |
Previous Ectopic Pregnancy | History of ectopic pregnancy in the past | Increased risk |
Fallopian Tube Damage | Damage to the fallopian tubes due to surgery, infection, or other conditions | Significantly increased risk |
Pelvic Inflammatory Disease (PID) | Infection of the female reproductive organs | Increased risk due to possible tubal damage |
Knowing about these risk factors and causes is key to managing IVF risks. Healthcare providers can take steps to lower the chance of an ectopic pregnancy by identifying these factors.
The Risk of Ectopic with IVF: Facts and Statistics
IVF is a common choice for those facing infertility. Yet, it raises the risk of ectopic pregnancy more than natural conception. It’s key to know this risk if you’re thinking about fertility treatments.
Comparing IVF vs. Natural Conception Ectopic Rates
Research shows IVF increases ectopic pregnancy risk over natural conception. A study in the Journal of Assisted Reproduction and Genetics found IVF’s ectopic rate at 2.1%. Natural conception’s rate is about 1.3%.
Here’s a table comparing ectopic pregnancy rates between IVF and natural conception:
Conception Method | Ectopic Pregnancy Rate (%) |
IVF | 2.1 |
Natural Conception | 1.3 |
The Impact of Multiple Embryo Transfer on Risk
Transferring multiple embryos in IVF raises ectopic pregnancy risk. The American Society for Reproductive Medicine advises against it. They say it increases the risk of multiple gestations and ectopic pregnancies.
This is because more embryos mean a higher chance of implanting outside the uterus.
Single embryo transfer is advised to lower this risk. It makes IVF safer for those seeking fertility help.
Healthcare providers should talk about the risks of multiple embryo transfer. They should also highlight the benefits of single embryo transfer. This helps patients make better choices about their fertility treatment.
Is Ectopic Pregnancy Hereditary or Genetic?
Ectopic pregnancy is a big worry in IVF, but it’s not caused by genes. It’s linked to other factors. People worried about hereditary or genetic links to ectopic pregnancy in IVF need to know the truth.
First, let’s talk about what ectopic pregnancy is. It happens when the embryo grows outside the uterus, often in the fallopian tube. The reasons for this are many and not because of genes or family history.
Debunking Common Misconceptions
Some think ectopic pregnancy runs in families. But, medical experts say it’s not hereditary or genetic. It’s more about past surgeries, infections, or issues with the fallopian tubes.
Another myth is that a family history of ectopic pregnancy raises your risk. While it’s a worry, your actual risk is tied to your own health history and conditions.
The True Causes of Ectopic Implantation
The reasons for ectopic implantation are many:
- Damage to the fallopian tubes
- Previous ectopic pregnancy
- Pelvic surgery
- In vitro fertilization (IVF) itself, if many embryos are transferred
- Uterine or fallopian tube shape issues
To grasp the risks, let’s look at IVF and natural conception risks:
Risk Factor | IVF Conception | Natural Conception |
Previous Tubal Surgery | Higher Risk | Higher Risk |
Pelvic Inflammatory Disease | Increased Risk | Increased Risk |
Multiple Embryo Transfer | Significantly Higher Risk | N/A |
Knowing these causes and risks helps us understand IVF ectopic pregnancy chances. We can then take steps to lower these risks.
Who is at Risk of Ectopic Pregnancy During IVF?
The risk of ectopic pregnancy during IVF varies among individuals. This is due to several key factors. Knowing these factors is key to identifying who might need closer monitoring or different treatment.
Age-Related Risk Factors
Advanced maternal age is a big risk factor for ectopic pregnancy in IVF patients. Women over 35 years old face a higher risk. This is because egg quality declines and the uterine environment may change. Older patients should talk to their healthcare provider about their risk.
Previous Tubal or Pelvic Conditions
Patients with a history of tubal damage or pelvic surgery are at higher risk. Conditions like tubal ligation or previous ectopic pregnancies can increase risk. We suggest patients with such histories get a thorough evaluation before starting IVF.
Decreased Ovarian Reserve Considerations
Women with decreased ovarian reserve may face a higher risk of ectopic pregnancy. This is because of possible changes in hormonal environments and uterine receptivity. Careful monitoring and personalized treatment can help reduce this risk.
By understanding these risk factors, we can make IVF treatment plans more effective. This helps lower the chance of ectopic pregnancy and improves treatment success rates.
Why Do Ectopic Pregnancies Occur in IVF Cycles?
It’s important to know why ectopic pregnancies happen in IVF. These pregnancies are rare but can be dangerous for the mother and the IVF treatment’s success.
Mechanical Factors in Embryo Transfer
The way embryos are transferred in IVF can lead to ectopic pregnancies. The technique used can greatly affect the risk of ectopic implantation.
- The depth and location of embryo placement in the uterus can impact the risk of ectopic pregnancy.
- Proper catheter placement is key to lower the risk of ectopic pregnancy.
- The type and volume of media used for transfer also play a role in the risk.
IVF Tubal Pregnancy: Causes and Mechanisms
Tubal pregnancies are a big worry in IVF, more so for women with tubal damage or past ectopic pregnancies. The reasons behind IVF tubal pregnancy involve complex interactions between the embryo and the tubal environment.
Key factors include:
- Reversal of tubal damage in cases where tubal function is compromised.
- The presence of underlying tubal pathology that may lead to ectopic implantation.
- The chance of embryo migration into the fallopian tubes during or after transfer.
Physiological Factors Affecting Implantation
Physiological factors are also key in ectopic pregnancies during IVF. These include hormonal effects, uterine receptivity, and the embryo’s implantation ability.
Some critical physiological factors are:
- Hormonal preparation of the uterus for implantation.
- The receptivity of the uterine lining and its ability to support implantation.
- The quality and developmental stage of the embryo at transfer time.
Understanding these factors helps us see why ectopic pregnancies happen in IVF. It also shows how we can reduce these risks.
10 Effective Strategies to Prevent Ectopic Pregnancy in IVF
[Add image here]
IVF patients can lower their ectopic pregnancy risk with several strategies. Understanding and using these methods can improve IVF success rates.
Comprehensive Pre-IVF Assessment
A detailed pre-IVF check is key to spotting ectopic pregnancy risks. This includes:
- Evaluating tubal health through hysterosalpingography (HSG) or laparoscopy
- Checking uterine anatomy and spotting any issues
- Screening for hormonal imbalances or other health problems
By tackling these issues before IVF, doctors can create a tailored plan to lower ectopic pregnancy risk.
Optimal Embryo Transfer Techniques
The embryo transfer method greatly affects ectopic pregnancy risk. Optimal embryo transfer techniques include:
- Using ultrasound for precise placement
- Avoiding deep or forceful transfers
- Choosing the right catheter size and type
Optimizing embryo transfer can lower ectopic implantation chances.
Hormonal Preparation Protocols
Hormonal prep is vital for IVF success. Tailored hormonal protocols create the best uterine environment, lowering ectopic pregnancy risk. This may involve:
- Customizing estrogen and progesterone doses
- Monitoring hormone levels during the IVF cycle
- Adjusting protocols based on patient response
Lifestyle Modifications
Medical interventions aren’t the only way to reduce ectopic pregnancy risk. Lifestyle modifications also play a role. These include:
- Keeping a healthy weight and eating well
- Avoiding smoking and drinking too much alcohol
- Managing stress with relaxation techniques
By making these lifestyle changes, individuals can boost their chances of a successful IVF.
The Role of Single Embryo Transfer in Avoiding Ectopic Pregnancy
Single embryo transfer is key in preventing ectopic pregnancies during IVF. It’s a major step to lower the risk of ectopic pregnancy for those trying IVF.
Statistical Evidence for Safety
Research shows single embryo transfer cuts down ectopic pregnancy risk. The latest figures show a big drop in ectopic pregnancy rates with this method.
Embryo Transfer Type | Ectopic Pregnancy Rate |
Single Embryo Transfer | 2.4% |
Multiple Embryo Transfer | 4.8% |
This data highlights the safety of single embryo transfer in lowering ectopic pregnancy risk.
Balancing Success Rates with Ectopic Prevention
Single embryo transfer lowers ectopic pregnancy risk but affects IVF success rates. New embryo culture and selection methods have made single embryo transfer more effective for many.
When Multiple Embryo Transfer May Be Considered
In some cases, like advanced maternal age or failed IVF attempts, multiple embryo transfer might be considered. But, it’s a careful decision, balancing benefits against higher risks of ectopic pregnancy and multiple births.
We look at each patient’s situation and use the latest IVF techniques. This way, we aim for success while keeping risks low.
Advanced IVF Techniques for Reducing Ectopic Risk
[Add image here]
IVF has evolved, leading to new techniques that lower ectopic pregnancy risk. These advancements are making fertility treatments more successful for patients.
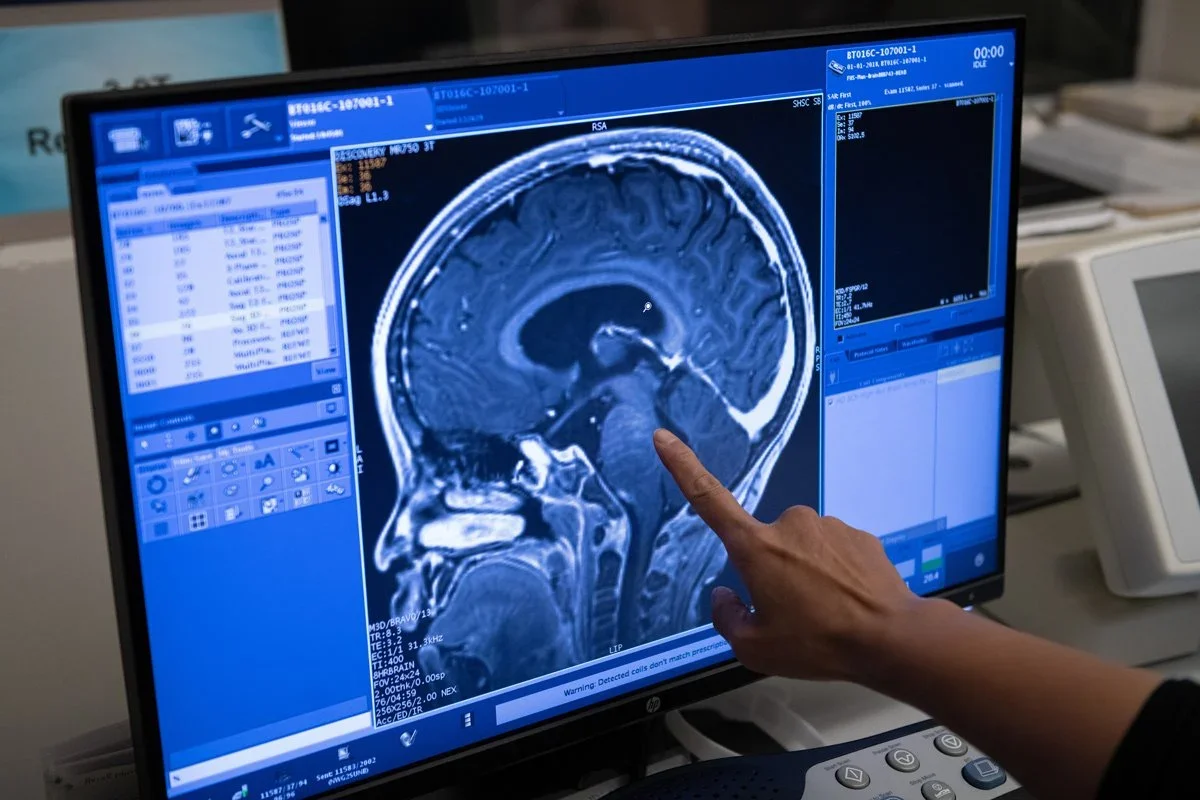
Ultrasound-Guided Embryo Transfer
Ultrasound-guided embryo transfer is a big step forward in IVF. It ensures the embryo is placed correctly in the uterus, cutting down ectopic pregnancy risk. Research shows this method boosts success rates and lowers risks.
“Ultrasound during embryo transfer has changed IVF,” notes Medical Expert, a top fertility expert. “It’s a major leap in reducing ectopic pregnancy risk and boosting success rates.”
Blastocyst vs. Cleavage Stage Transfer
The timing of embryo transfer is also key. Blastocyst transfer, done 5-6 days post-fertilization, has a lower ectopic risk than cleavage-stage transfer. This is because blastocysts are more developed and likely to implant well.
- Blastocyst transfer helps pick the best embryos.
- It matches the embryo transfer with the uterine environment.
- It lowers the chance of multiple pregnancies with single embryo transfer.
The Promise of PGT-A Testing
Preimplantation Genetic Testing for Aneuploidy (PGT-A) checks embryos for chromosomal issues before transfer. PGT-A enhances IVF success by picking embryos likely to implant and lead to healthy pregnancies.
Using these advanced methods—ultrasound-guided transfer, blastocyst transfer, and PGT-A testing—we can greatly lower ectopic pregnancy risk. This improves IVF treatment success rates.
Medical Management to Minimize Ectopic Pregnancy Risk
We can lower the risk of ectopic pregnancy with careful medical management. This includes treating underlying conditions and making the uterus more receptive. A detailed approach makes IVF safer and more effective.
Treating Underlying Conditions Before IVF
It’s key to treat any conditions that might raise ectopic pregnancy risk before starting IVF. This includes tubal damage, endometriosis, and pelvic inflammatory disease. “Treating these conditions can significantly improve the chances of a successful IVF outcome,” says Medical Expert, a leading fertility specialist.
We suggest a thorough check-up, including imaging and tests, to find any issues. Fixing these problems early on helps lower ectopic pregnancy risks.
Medication Protocols to Improve Uterine Receptivity
Medications are vital in making the uterus ready for embryo transfer. This reduces ectopic pregnancy risk. We follow proven protocols to get the uterus in the best shape for implantation.
We use hormonal therapies and other meds to create a healthy uterine environment. This boosts the chances of a successful pregnancy and lowers ectopic implantation risk.
Managing Previous Ectopic Pregnancy History
For those with a history of ectopic pregnancy, we create a special plan. We look at the patient’s medical history, past treatments, and current health. This helps us tailor the IVF plan to their needs.
Understanding what led to the previous ectopic pregnancy helps us craft a safe and effective IVF plan. Our aim is to help patients have a healthy pregnancy.
Key Takeaways:
- Treating underlying conditions before IVF is key.
- Medication protocols can improve uterine receptivity.
- Managing previous ectopic pregnancy history is vital for risk reduction.
By using these strategies in our IVF protocols, we can lower ectopic pregnancy risk. This improves IVF success rates overall.
Early Detection: Monitoring After IVF to Identify Ectopic Pregnancy
The journey through IVF doesn’t end with embryo transfer. It’s important to monitor carefully to detect ectopic pregnancies. We guide patients through this critical period, stressing the need for early detection.
Beta-hCG Monitoring Protocol
Beta-hCG monitoring is a key tool in early detection. After IVF, we measure beta-hCG levels 9-11 days post-transfer. We track these levels closely to spot any issues.
A normal pregnancy shows beta-hCG levels doubling every 48 hours early on. An ectopic pregnancy might show slower or no increase. This info is vital for our next steps.
Early Ultrasound Screening Timeline
Early ultrasound screening is also critical. The first ultrasound is usually at 6 weeks (4 weeks post-transfer). It helps us find the pregnancy and check if it’s viable.
For IVF patients, the ultrasound timeline can change based on risk factors. If there’s concern about ectopic pregnancy, we might do an earlier scan.
Warning Signs to Watch For
Monitoring is key, but knowing the warning signs of ectopic pregnancy is also important. Symptoms include abdominal pain, vaginal bleeding, dizziness, or shoulder pain. If you experience these, seek medical help right away.
“Ectopic pregnancy can be life-threatening if not caught early. Knowing the warning signs is essential for quick detection and treatment.”
Medical Expert, Fertility Specialist
By using beta-hCG monitoring, early ultrasound, and knowing warning signs, we can spot ectopic pregnancies early in IVF patients. This approach helps us act fast and improve outcomes for fertility treatment.
Conclusion: Balancing IVF Success with Ectopic Prevention
To balance IVF success and prevent ectopic pregnancies, we need careful planning and monitoring. We’ve talked about ways to lower ectopic pregnancy risks. These include thorough pre-IVF checks, the best embryo transfer methods, and hormone prep plans.
Knowing the risks and using these strategies can greatly lower ectopic pregnancy chances. Choosing single embryo transfer is key. It helps avoid ectopic pregnancies while keeping success rates high.
Using advanced IVF methods like ultrasound-guided transfers and PGT-A tests boosts success rates and lowers risks. Early detection through beta-hCG tests and ultrasounds is also critical. It helps spot problems early.
By taking these steps and tailoring IVF treatment to each patient, we can increase success rates safely. Preventing ectopic pregnancies is essential for IVF success. We must keep improving our methods to give patients the best results.
FAQ
Are ectopic pregnancies hereditary?
No, ectopic pregnancies are not passed down through genes. They happen due to issues like fallopian tube damage or blockage, not because of family history.
Why does an ectopic pregnancy happen during IVF?
An ectopic pregnancy during IVF occurs when the embryo implants outside the uterus. This can happen due to the way the embryo is placed during transfer or because of issues with implantation.
Is ectopic pregnancy genetic?
No, ectopic pregnancy is not caused by genes. The risk is linked to medical history, fallopian tube condition, and other non-genetic factors.
How to prevent an ectopic pregnancy with IVF?
To prevent ectopic pregnancy with IVF, start with a thorough pre-IVF check-up. Use the best embryo transfer methods and follow hormone preparation plans. Also, making healthy lifestyle choices can help.
Can you have an ectopic pregnancy with IVF?
Yes, ectopic pregnancy can happen with IVF. This is more likely if there’s damage or blockage in the fallopian tubes.
What is the risk of ectopic pregnancy with IVF?
The risk of ectopic pregnancy with IVF is higher than with natural conception. This is true, even more so with transferring multiple embryos. But, transferring just one embryo can lower this risk.
How does multiple embryo transfer affect the risk of ectopic pregnancy?
Transferring more than one embryo increases the risk of ectopic pregnancy. Transferring just one embryo is safer and keeps IVF success rates high.
Who is at risk of ectopic pregnancy during IVF?
Older women, those with past tubal or pelvic issues, and those with low ovarian reserve are at higher risk of ectopic pregnancy during IVF.
Why do ectopic pregnancies occur in IVF cycles?
Ectopic pregnancies in IVF cycles are caused by both mechanical and physiological factors. This includes the embryo transfer process and the patient’s individual characteristics.
What are the benefits of single embryo transfer in reducing ectopic pregnancy risk?
Single embryo transfer lowers the risk of ectopic pregnancy while keeping IVF success rates high. It’s a good choice for many patients.
How can advanced IVF techniques reduce the risk of ectopic pregnancy?
Advanced techniques like ultrasound-guided embryo transfer, transferring embryos at the blastocyst stage, and PGT-A testing can reduce ectopic pregnancy risk.
What role does medical management play in minimizing ectopic pregnancy risk?
Medical management is key in reducing ectopic pregnancy risk. This includes treating underlying conditions and using medications to improve uterine receptivity.
How can early detection help in identifying ectopic pregnancy after IVF?
Early detection is vital. It involves monitoring beta-hCG levels, early ultrasound screenings, and recognizing warning signs. This allows for timely action to address the issue.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4315158/