Last Updated on December 2, 2025 by Bilal Hasdemir
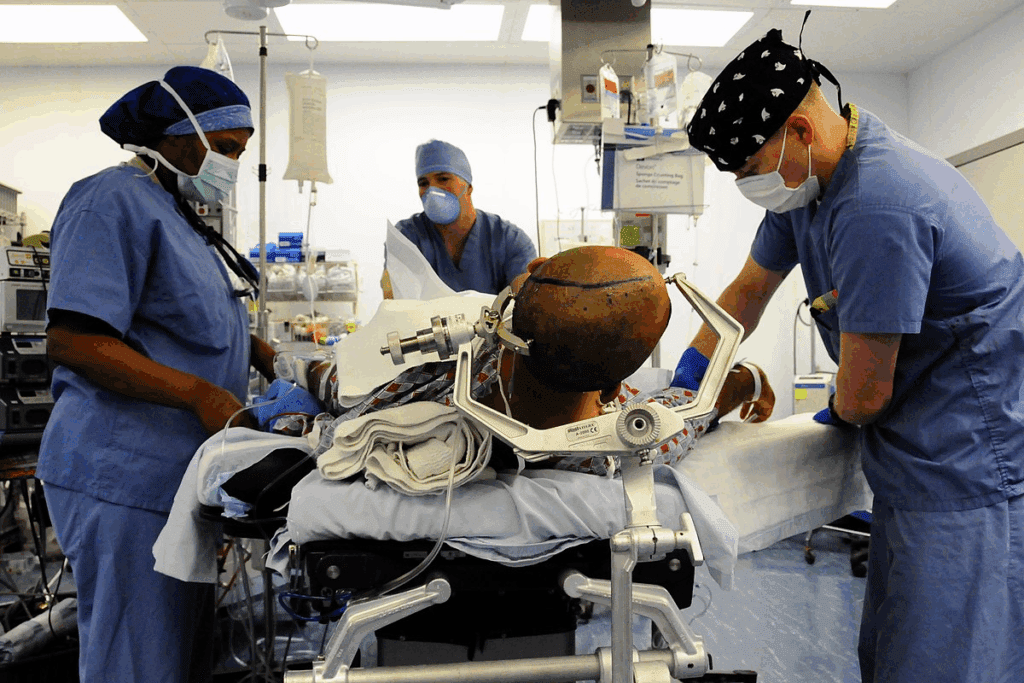
Brain stem surgery is a very complex and delicate operation. It involves the part of the brain that controls many automatic functions. These include breathing, heart rate, and blood pressure. It’s a procedure that requires utmost care and precision.
We know that undergoing such a surgery can be daunting. It’s natural to have concerns about the possible complications.
The risks associated with brain stem surgery are significant and can be life-altering. Complications can arise during or after the surgery. It’s important for patients and their families to be aware of these risks. This way, they can make informed decisions about their care.
Key Takeaways
- Understanding the complexity of brain stem surgery
- Recognizing the risks and complications
- The importance of precision and care in the procedure
- Being aware of the possible dangers and their impact
- The role of patient education in managing expectations
Understanding the Brain Stem: Anatomy and Function
It’s key to know about the brain stem’s anatomy and function. This part of our brain controls many automatic functions. It links the cerebrum to the spinal cord and handles vital life functions like breathing and heart rate.
Critical Functions Controlled by the Brain Stem
The brain stem manages several important functions, including:
- Respiratory Function: It controls breathing and how often we breathe.
- Cardiovascular Control: It manages our heart rate and blood pressure.
- Swallowing and Digestion: It helps with swallowing and other digestion steps.
- Arousal and Alertness: It keeps us conscious and alert.
Anatomical Complexity and Surgical Challenges
The brain stem’s detailed anatomy makes surgery hard. Its close location to vital areas and the thinness of nearby tissues add to the complexity.
Anatomical Feature | Surgical Challenge |
Proximity to Vital Structures | Increased risk of damage to critical areas |
Delicate Surrounding Tissues | Risk of causing unintended damage during surgery |
Complex Neural Pathways | Difficulty in preserving neural function |
Neurosurgeons must understand these complexities to tackle brain stem surgery’s challenges.
Overview of Brain Stem Surgery Procedures
It’s important to know about the different brain stem surgery procedures. This helps us understand the risks and possible results. These surgeries are complex and need careful techniques and knowledge of the brain’s structure.
These surgeries treat various conditions like tumors and blood vessel problems. The type of surgery depends on the condition’s location and the patient’s health.
Common Types of Brain Stem Operations
Brain stem operations are divided into different types based on the method used. Here are some common ones:
- Microvascular decompression: This method relieves pressure on the brain stem from blood vessels.
- Tumor resection: It involves removing tumors near or in the brain stem.
- Stereotactic surgery: A less invasive method that uses precise coordinates to target specific brain areas.
A leading neurosurgeon says, “The success of brain stem surgery depends on choosing the right approach and technique.” This shows how complex and specialized these surgeries are.
Surgical Approaches to the Brain Stem
The way to reach the brain stem during surgery varies based on the condition. Surgeons might use:
- Suboccipital approach: Used for lesions in the brain stem’s lower part.
- Retrosigmoid approach: Accesses the cerebellopontine angle and the brain stem’s lateral side.
- Orbital or supraorbital approach: Suitable for lesions in the front part.
Each method has its benefits and challenges. Choosing the right approach is key to reducing risks and achieving a good outcome.
General Risks of Brain Stem Surgery
Brain stem surgery is a complex procedure with many risks. These include problems with anesthesia, infection, and bleeding. These risks can greatly affect a patient’s recovery and quality of life.
Anesthesia-Related Complications
Anesthesia is key for brain stem surgery, making it painless. But, anesthesia-related complications can happen. These can range from mild to severe, including respiratory issues and allergic reactions. Rarely, it can lead to anaphylaxis.
To lower these risks, anesthesiologists check each patient’s health before surgery. They use advanced monitoring during the surgery to quickly spot and fix any problems.
Infection Risks
Infection is a big risk with brain stem surgery. Like any surgery, there’s a chance of infection at the site or in the brain. Infection risks can be higher if the patient’s health is poor or the surgery is complex.
To fight these risks, surgical teams follow strict infection control. They use antibiotics and focus on wound care. Patients are watched closely for signs of infection after surgery.
Bleeding and Hemorrhage
Bleeding and hemorrhage are serious risks during or after surgery. The brain stem’s blood vessels make it prone to bleeding. This can cause brain damage and other serious issues.
To reduce bleeding risks, surgeons use advanced techniques and special instruments. Patients are also closely watched for signs of bleeding after surgery.
Mortality and Morbidity Statistics
Mortality and morbidity rates are key to judging the safety and success of brain stem surgeries. These numbers help patients and doctors make smart choices about treatment.
Fatality Rates Associated with Brain Stem Procedures
Fatality rates for brain stem surgery change a lot. They depend on the surgery type, the patient’s health, and the condition being treated. Studies show the death rate can be between 5% and 20% or more for complex cases. It’s important to remember these numbers vary greatly based on each case’s details.
“The death rate for brain stem surgery is a key factor in deciding if the surgery is right for a patient,” says a top neurosurgery journal. “New surgical methods and better care before and after surgery have helped lower death rates over time.”
Long-term Morbidity Outcomes
Long-term effects of brain stem surgery are just as important as death rates. These effects can include brain damage, memory problems, and other issues that affect daily life. Research shows that 30% to 60% of patients may face long-term problems, depending on the surgery’s complexity and the patient’s health before surgery.
- Neurological Deficits: Patients might suffer from nerve damage, motor or sensory problems, or other brain issues.
- Cognitive Impairments: Some may struggle with memory, focus, or other brain functions.
- Quality-of-Life Issues: The surgery’s impact on a patient’s life can be big, needing lots of help and support.
We know these numbers might seem scary, but they’re vital for making choices. By knowing the risks, we can prepare for challenges and aim for the best results.
Neurological Complications
Brain stem surgery is delicate and can lead to neurological complications. These issues can greatly affect a patient’s life and recovery.
Cranial Nerve Damage
Cranial nerve damage is a big risk in brain stem surgery. The brain stem has nerves that control important functions like swallowing, speaking, and breathing. Damage can cause problems with these functions, leading to disabilities.
Some common issues include:
- Dysphagia (difficulty swallowing)
- Dysarthria (speech difficulties)
- Respiratory problems
Motor and Sensory Deficits
Motor and sensory deficits are possible after brain stem surgery. The brain stem controls movement and sends sensory information. Surgery can cause weakness, numbness, or paralysis in different parts of the body.
These deficits can vary based on the surgery’s location and extent. Some patients may face:
- Weakness or paralysis of limbs
- Numbness or altered sensation
- Coordination and balance problems
Seizure Development
Seizures can also be a complication after brain stem surgery. While rare, they can happen due to surgery irritation or postoperative changes.
We watch patients for seizure signs and try to prevent them. Factors that may raise seizure risk include:
- Previous history of seizures
- Extent of surgical intervention
- Postoperative brain edema or hemorrhage
Knowing about these complications helps us manage patient expectations and care. By understanding these risks, we can better support patients and their families during recovery.
Respiratory Complications After Brain Stem Surgery
Brain stem surgery can cause breathing problems and even respiratory failure. The brain stem controls our breathing. Damage during surgery can lead to serious respiratory issues.
Breathing Difficulties and Respiratory Failure
After brain stem surgery, breathing problems are common. These can be mild or severe, needing quick medical help. Respiratory failure is very serious and requires ventilatory support to keep blood and tissues oxygenated.
Several factors can increase the risk of these breathing problems. These include the surgery’s location and type, the patient’s health before surgery, and any existing respiratory conditions.
- Damage to respiratory centers: The brain stem has key centers for breathing. Damage here can affect breathing.
- Swelling and inflammation: Swelling or inflammation after surgery can press on or harm nearby brain areas, causing breathing issues.
- Pre-existing respiratory conditions: People with respiratory diseases before surgery are more likely to face breathing problems after.
Need for Ventilatory Support
When brain stem surgery severely affects breathing, patients might need ventilatory support. This can include non-invasive methods like CPAP or invasive mechanical ventilation through a tube in the throat.
“The need for ventilatory support after brain stem surgery shows how complex and risky these surgeries are. Good planning before and care after surgery are key to managing these risks.”
The choice to use ventilatory support depends on how bad the breathing problems are and the patient’s overall health. Patients often need close monitoring in an intensive care unit to quickly spot and handle any breathing issues.
Knowing the risks and complications of brain stem surgery helps healthcare providers prepare for and manage breathing problems. This can lead to better outcomes for patients.
Swallowing and Speech Impairments
Brain stem surgery can affect a patient’s ability to swallow and speak. The brain stem controls many bodily functions, including swallowing and speech. Damage to the cranial nerves during surgery can lead to impairments.
These impairments can make daily life hard. They happen because of the brain stem’s complex role in our body. It’s important for patients and doctors to know about these risks to plan for recovery.
Dysphagia Following Brain Stem Operations
Dysphagia, or trouble swallowing, is a common issue after brain stem surgery. It happens when nerves for swallowing get damaged. This can cause malnutrition and pneumonia if not treated.
Dealing with dysphagia can be tough for patients. So, it’s key to start swallowing tests and therapy early. Speech-language pathologists help patients get better at swallowing.
Dysarthria and Communication Challenges
Dysarthria, or hard-to-understand speech, can also happen after brain stem surgery. It’s caused by nerve damage to speaking muscles. This makes it hard for patients to talk clearly, leading to feelings of isolation.
It’s important to tackle dysarthria and other speech issues quickly. Speech therapy can help patients improve their speaking. With the help of speech-language pathologists, patients can get better at communicating.
In summary, swallowing and speech problems are big risks with brain stem surgery. Knowing about these risks and how to manage them can help patients recover better and live better lives.
Balance, Coordination, and Mobility Issues
Mobility issues can happen after brain stem surgery. This is because the surgery affects how our body moves. These problems can make simple tasks hard to do.
The brain stem controls many automatic functions. This includes balance and how we move. Surgery in this area can cause trouble with balance and movement.
Ataxia and Gait Disturbances
Ataxia is a condition that affects muscle coordination. It can cause problems with walking and balance. Gait disturbances also occur, making it hard to walk.
Symptoms of ataxia and gait disturbances include:
- Unsteady walking
- Difficulty with balance
- Clumsiness in hands and fingers
- Frequent falls
Long-term Rehabilitation Needs
Patients with these issues need long-term help. They might need physical therapy to get better. This therapy helps with strength, balance, and coordination.
We create a detailed plan for each patient. This plan helps them become independent again. It’s made with a team of healthcare experts.
Knowing about these issues helps us prepare patients. We can offer the right support and care.
Specific Risks of Brain Stem Surgery by Location
Brain stem surgery risks change based on the area being operated on. The midbrain, pons, and medulla oblongata each have unique features. These differences affect the surgery’s complexity and possible complications.
Midbrain Surgery Complications
The midbrain connects the forebrain and hindbrain. It’s key for processing sounds and images. Surgery here can cause specific problems, such as:
- Damage to the oculomotor nerve: This can make eye movement and pupil dilation hard.
- Impaired auditory processing: Damage can cause hearing problems.
- Motor control issues: Surgery can lead to tremors, rigidity, or other movement disorders.
Pons Surgery Risks
The pons control sleep and arousal. Surgery here can cause:
- Cranial nerve damage: This can lead to facial weakness or trouble swallowing.
- Respiratory complications: Surgery can affect breathing, leading to breathing issues.
- Sensory disturbances: Damage can cause numbness, tingling, or other sensory problems.
Medulla Oblongata Procedure Dangers
The medulla oblongata is at the brain stem’s bottom. It connects the pons and spinal cord. It’s vital for breathing, heart rate, and blood pressure. Surgery here is very challenging and can lead to:
- Life-threatening respiratory complications: Damage can cause respiratory failure, needing a ventilator.
- Cardiovascular instability: It can affect heart rate and blood pressure.
- Swallowing difficulties: Damage can cause trouble swallowing.
Knowing these risks is key for neurosurgeons and patients. It helps in planning, approach, and care after surgery. By understanding these risks, we can better help patients with brain stem surgery.
Consciousness Disorders and Cognitive Impairments
Brain stem surgery can lead to many challenges for patients. We need to understand the different disorders that can happen.
Coma and Vegetative States
One big risk of brain stem surgery is coma or vegetative states. These are serious changes in consciousness. Patients might seem awake but don’t respond or know what’s going on.
It’s important to know how brain stem surgery can affect consciousness. Sometimes, it can cause severe problems.
Locked-in Syndrome
Locked-in syndrome is another risk. Patients are awake but can’t move or talk because of total muscle paralysis. They can only move their eyes.
This shows how careful brain stem surgery needs to be. We must use precise techniques to avoid such problems.
Cognitive and Memory Deficits
Brain stem surgery can also cause cognitive and memory problems. These can be mild or severe. They can affect a patient’s life and daily tasks.
It’s key to understand these possible issues. This helps set realistic expectations and plan for recovery after surgery.
Condition | Description | Potential Impact |
Coma | A state of deep unconsciousness | Significant alteration in consciousness, lack of responsiveness |
Vegetative State | A condition of being awake but not aware | Patients appear awake but lack awareness of their surroundings |
Locked-in Syndrome | Paralysis of all voluntary muscles except for the eyes | Patients are aware but unable to move or communicate verbally |
Vascular Complications
Vascular complications, like stroke and vessel damage, are risks of brain stem surgery. The brain stem’s rich blood supply and delicate structure make surgery here very hard.
Stroke Risk During and After Surgery
Stroke is a big worry during and after brain stem surgery. This worry comes from handling blood vessels and the chance of damaging the ones near the brain stem. Stroke can happen from blood clots, blockages, or bleeding, and it can be very harmful, causing serious problems or even death.
We know patients worry a lot about stroke risks with brain stem surgery. So, it’s very important to check the blood vessels before surgery and watch patients closely during and after.
Vessel Damage and Management
Vessel damage is another problem that can happen during brain stem surgery. The brain stem has a complex network of blood vessels. Damage to these can cause serious bleeding or lack of blood flow. Using skilled surgical techniques and careful planning before surgery is key to avoid vessel damage.
If vessel damage does happen, quick and good management is very important. This might mean using intraoperative angiography to find the bleeding or damage. Then, the right steps are taken to fix or block the affected vessel.
We stress the need for a team effort to handle vascular problems. This team should include neurosurgeons, radiologists, and other experts to get the best results for patients.
Cerebrospinal Fluid-Related Complications
Patients having brain stem surgery face serious cerebrospinal fluid-related complications. These issues come from the surgery’s delicate nature and the area’s importance.
CSF Leaks
A CSF leak is a big worry. It happens when the dura mater, the brain and spinal cord’s protective layer, gets damaged. This lets cerebrospinal fluid leak out.
CSF leaks can cause problems like:
- Infection: The leak can let bacteria into the brain, raising infection risks.
- Headaches and discomfort: Losing CSF can lead to headaches and discomfort due to pressure changes.
- Need for more surgery: Sometimes, a CSF leak needs more surgery to fix the dura mater.
Hydrocephalus Development
Brain stem surgery can also lead to hydrocephalus. This is when too much cerebrospinal fluid builds up in the brain, causing pressure to rise.
Condition | Description | Potential Outcomes |
CSF Leaks | Breach in the dura mater allowing CSF to escape | Infection, headaches, need for additional surgery |
Hydrocephalus | Accumulation of CSF within the brain | Increased intracranial pressure, cognitive impairments, need for shunting procedure |
Hydrocephalus can come from surgery or complications like bleeding or infection. It can cause headaches, nausea, vomiting, and problems with thinking. Sometimes, a shunt is needed to manage the fluid.
Knowing about these complications helps manage patient hopes and results. Healthcare teams can lessen these risks and better care for patients by understanding and acting on them.
Risk Factors That Increase Complications
Brain stem surgery comes with risks. It’s important to know the patient-specific and surgical risk factors to reduce complications. Many factors can affect the outcome of such a delicate procedure.
Patient-Specific Risk Factors
Patient-specific factors greatly affect the risk of brain stem surgery. Age, overall health, and pre-existing medical conditions are key. For example, older patients or those with diabetes or high blood pressure may face higher risks.
Also, the patient’s neurological status before surgery is important. Patients with severe neurological deficits may have a higher risk of complications. This includes longer recovery times or the need for extended rehabilitation.
Tumor Characteristics and Location
The tumor’s characteristics and location in the brain stem are vital. Tumors that are deeply embedded or closely associated with critical brain stem structures are more challenging. This can increase the risk of neurological damage during surgery.
The size and type of tumor also affect the surgery’s complexity. Larger or more aggressive tumors may require more extensive surgeries. This can increase the risk of complications.
Surgical Approach Considerations
The surgical approach chosen can impact the risk of brain stem surgery. Minimally invasive techniques may reduce recovery time and lower risks. But, more traditional open surgeries might be needed for larger or more complex tumors. This could increase the risk of post-operative issues.
Choosing the right surgeon and a multidisciplinary team is key. They help decide the best surgical approach. This balances effective tumor removal with minimizing risks to the patient.
Minimizing the Risks of Brain Stem Surgery
Brain stem surgery is complex but can be safer with advanced techniques and careful planning. The brain stem controls vital functions, making surgery here very precise and careful.
Advanced Surgical Techniques
Using advanced techniques is key to reducing risks in brain stem surgery. Microsurgical techniques offer more precision and less damage. Neuro-navigation helps surgeons understand the anatomy better and plan their approach.
Some advanced techniques include:
- Minimally invasive surgery to reduce tissue damage
- Use of lasers for precise dissection
- Intraoperative imaging to guide the surgery
Preoperative Planning and Imaging
Good preoperative planning is essential for brain stem surgery success. Detailed imaging, like MRI and CT scans, helps understand the patient’s anatomy and the condition being treated.
Imaging Technique | Purpose |
MRI | Detailed soft tissue imaging |
CT Scan | Quick assessment of anatomy and pathology |
Intraoperative Monitoring
Intraoperative monitoring is vital for brain stem surgery safety. Electrophysiological monitoring checks the function of key neural structures during surgery. This allows for quick adjustments if needed.
Key benefits of intraoperative monitoring include:
- Real-time feedback on neural function
- Ability to adjust surgical technique on the fly
- Reduced risk of postoperative neurological deficits
Conclusion
We’ve looked into the risks of brain stem surgery, a very complex procedure. It’s key for patients and doctors to know these risks well.
Brain stem surgery can lead to serious problems like neurological, respiratory, and vascular issues. The brain stem controls important functions, making surgery here very tricky.
To lower these risks, we use advanced surgery methods, detailed planning before surgery, and monitoring during it. We must think about each patient’s unique risks, the tumor’s type, and the surgery plan to get the best results.
In short, brain stem surgery is risky, but with careful planning and new techniques, we can reduce these risks. It’s vital to understand these risks well to help patients get the best care possible.
FAQ
What are the general risks associated with brain stem surgery?
Brain stem surgery carries several risks because the area controls vital functions. Common risks include problems with anesthesia, infection, and bleeding during or after the operation. These complications can have a serious effect on the patient’s overall health and recovery.
What are the possible neurological complications of brain stem surgery?
Neurological complications may occur when the delicate nerves and pathways around the brain stem are affected. The surgery can damage cranial nerves, leading to motor or sensory problems, and in some cases, cause seizures or partial paralysis.
What are the risks of respiratory complications after brain stem surgery?
Respiratory issues are among the most serious risks after brain stem surgery. Because the brain stem helps regulate breathing, any damage or swelling in this area can make it difficult to breathe independently. Some patients may require temporary or prolonged ventilator support.
Can brain stem surgery lead to swallowing and speech impairments?
Yes, brain stem surgery can cause problems with swallowing and speech. This happens when the nerves controlling these functions are affected. Difficulty swallowing and speaking can greatly impact a patient’s quality of life and may require therapy for improvement.
What are the possible balance and coordination issues after brain stem surgery?
Balance and coordination problems are also common after brain stem surgery. Patients may struggle with walking or maintaining balance due to disruption in motor control pathways. These issues often improve with physical therapy and long-term rehabilitation.
How does the location within the brain stem affect the risks of surgery?
The risks depend on the exact location of the surgery within the brain stem. Procedures involving the midbrain, pons, or medulla oblongata carry different challenges, as each region controls specific vital functions. The closer the surgery is to critical areas, the higher the risk.
What are the possible consciousness disorders and cognitive impairments after brain stem surgery?
Some patients may experience disorders of consciousness such as coma, vegetative states, or reduced awareness following surgery. Cognitive impairments, including memory loss or difficulty with focus and decision-making, can also occur depending on the extent of the damage.
What are the vascular complications associated with brain stem surgery?
Vascular complications are a major concern because the brain stem has a rich network of blood vessels. Surgery can lead to stroke, vessel damage, or reduced blood flow to critical brain areas. These complications can affect both short-term recovery and long-term function.
Can brain stem surgery lead to cerebrospinal fluid-related complications?
Yes, cerebrospinal fluid (CSF) issues are possible after surgery. Patients may develop CSF leaks, which increase infection risk, or hydrocephalus, which is a buildup of fluid in the brain that causes pressure and requires further treatment.
What are the risk factors that increase the likelihood of complications during and after brain stem surgery?
Several factors can make complications more likely, such as the patient’s age, overall health, and the type of brain condition being treated. The complexity of the tumor or lesion and the chosen surgical technique also play a major role in determining the outcome.
How can the risks associated with brain stem surgery be minimized?
Risks can be reduced through careful surgical planning, advanced imaging, and the use of modern microsurgical techniques. Having an experienced neurosurgical team and close monitoring during and after surgery also significantly improves safety and outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/9632179/