
Did you know that over 600,000 hysterectomies are done every year in the United States? A big part of these use minimally invasive techniques. Is cervix removed during robotic hysterectomy surgery? Understand total vs subtotal hysterectomy options and benefits.
Many women find robotic hysterectomy to be transformative, offering an advanced solution for several gynecological conditions. But, a big question is: does the cervix get removed during this cervix removal procedure? The answer depends on why the surgery is needed and the patient’s health.
We will dive into the details of robotic hysterectomy. We’ll look at when the cervix is removed, helping you understand this big medical choice.
Key Takeaways
- Whether the cervix is removed during a robotic hysterectomy depends on the medical reason.
- Minimally invasive hysterectomy methods, like robotic surgery, have many benefits over open surgery.
- Knowing about the cervix removal procedure is key for making an informed choice.
- Robotic hysterectomy surgery is a cutting-edge, precise way to do hysterectomies.
- Whether the cervix is removed also depends on the patient’s health and the reason for the surgery.
Understanding Hysterectomy: A Complete Overview
A hysterectomy is a big surgery where a woman’s uterus is removed. It’s done for many health reasons. We’ll look at what this surgery is and why it’s needed.
Definition and Basic Concepts
A hysterectomy is when a woman’s uterus is surgically removed. It’s often chosen when other treatments don’t work or aren’t right. The surgery can be done in different ways, like through the belly, vagina, or laparoscopically, sometimes with robots.
Choosing to have a hysterectomy means understanding the surgery and its effects on health. It’s a big choice made with doctors, considering the woman’s health and what she wants.
Common Reasons for Hysterectomy
Hysterectomies are done for many health reasons, including:
- Uterine Fibroids: These are non-cancerous growths in the uterus that can cause pain and heavy bleeding.
- Endometriosis: This is when tissue like the uterus lining grows outside the uterus, causing pain.
- Uterine Prolapse: When the uterus slips into the vagina.
- Cancer: It’s a treatment for cancers of the uterus, cervix, and ovaries.
- Abnormal Uterine Bleeding: Heavy or irregular bleeding that can’t be treated with other methods.
These issues can really affect a woman’s life. A hysterectomy might be considered if other treatments don’t work or aren’t right. The choice to have a hysterectomy is made after talking it over with doctors.
Different Types of Hysterectomy Procedures
Hysterectomy surgery comes in many forms, like total, supracervical, and radical hysterectomy. Each one handles the cervix differently. Knowing these details is key for both patients and doctors to choose the right surgery.
Total Hysterectomy: Complete Removal
A total hysterectomy removes both the uterus and cervix. It’s often chosen for uterine cancer, severe endometriosis, or big uterine prolapse. The cervix’s removal is a big part of this surgery, making sure all bad tissues are gone.
Supracervical (Partial) Hysterectomy: Cervix Preservation
A supracervical or partial hysterectomy takes out the top part of the uterus but keeps the cervix. This is for patients who want to keep their cervix, which might lower some risks. But, talking to a doctor about the pros and cons is important.
Radical Hysterectomy: Extended Removal
A radical hysterectomy is for cancer cases. It removes the uterus, cervix, part of the vagina, and sometimes nearby tissues and lymph nodes. This big removal is key for fighting cancer, making sure all cancerous tissues are taken out.
To understand the differences, let’s look at a table:
| Procedure | Cervix Removal | Typical Indications |
| Total Hysterectomy | Yes | Uterine cancer, severe endometriosis, uterine prolapse |
| Supracervical Hysterectomy | No | Uterine fibroids, abnormal bleeding, endometriosis |
| Radical Hysterectomy | Yes | Cervical cancer, uterine cancer |
The table shows removing or keeping the cervix depends on the hysterectomy type and the medical reason. It’s vital for patients to talk with their doctor to pick the best surgery for them.
The Role of the Cervix in Female Anatomy and Health
The cervix is a key part of the female reproductive system. It’s the lower, narrow part of the uterus that opens into the vagina. Knowing its role is important for women thinking about a hysterectomy, like whether to keep or remove the cervix.
Anatomical Function and Purpose
The cervix has many important jobs. It makes mucus that changes to help or block sperm. During pregnancy, it stays closed to support the growing baby. It opens during labor to help with childbirth. The cervix plays a big role in reproductive health, supporting pregnancy and childbirth.
The cervix is made of fibrous and muscular tissue. This lets it keep its shape and do its jobs. The cervical canal connects the uterus to the vagina, letting menstrual blood and other secretions pass through.
| Function | Description |
| Mucus Production | Produces mucus that changes consistency throughout the menstrual cycle |
| Pregnancy Support | Remains closed during pregnancy to support the fetus |
| Childbirth | Dilates during labor to allow childbirth |
Physiological Implications of Cervix Removal
Removing the cervix during a hysterectomy, known as a total hysterectomy, has several physiological implications. Some women may notice changes in vaginal discharge or sexual function. The possible effects on sexual satisfaction and vaginal health should be thought about when deciding to remove the cervix.
Studies show that keeping the cervix can have benefits, like a lower risk of vaginal cuff dehiscence and possibly better sexual function. But, if there’s cervical disease, removal might be needed. The choice should be made with a healthcare provider, considering the patient’s specific situation and medical history.
Understanding the cervix’s role and the effects of removing it is key for making informed decisions about hysterectomy. By looking at the anatomical and physiological aspects, women can choose what’s best for their health and personal preferences.
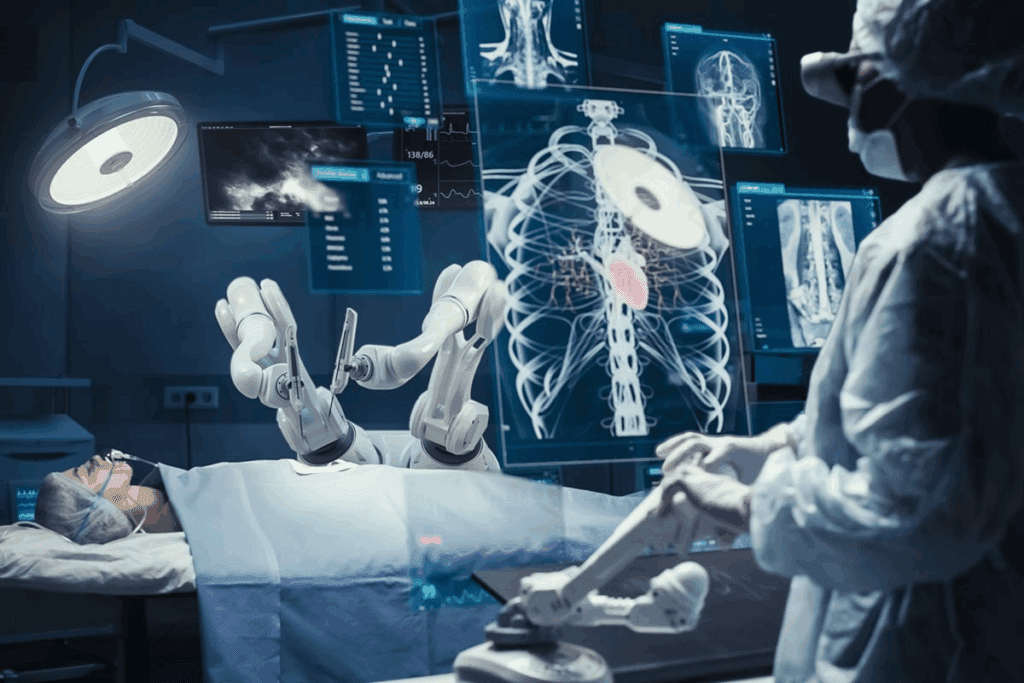
Robotic Hysterectomy Surgery: The Modern Approach
Robotic hysterectomy surgery is a big step forward in gynecology. It gives patients a precise and less invasive option compared to old methods. This new way of doing hysterectomies uses advanced robotic technology.
Today, we can do complex gynecology surgeries with better precision and control. This is thanks to the advanced robotic systems we have. These systems help surgeons do delicate tasks more accurately. This means fewer complications and quicker recovery times for patients.
What Makes a Hysterectomy “Robotic”
A hysterectomy is called “robotic” if it uses a robotic surgical system. This system has a console, robotic arms, and a 3D vision system. The surgeon controls the robotic arms from the console, making precise movements.
The robotic system translates the surgeon’s hand movements into precise actions of the surgical instruments. This gives surgeons enhanced dexterity and control during surgery. It makes complex tasks like dissections and suturing easier and more accurate.
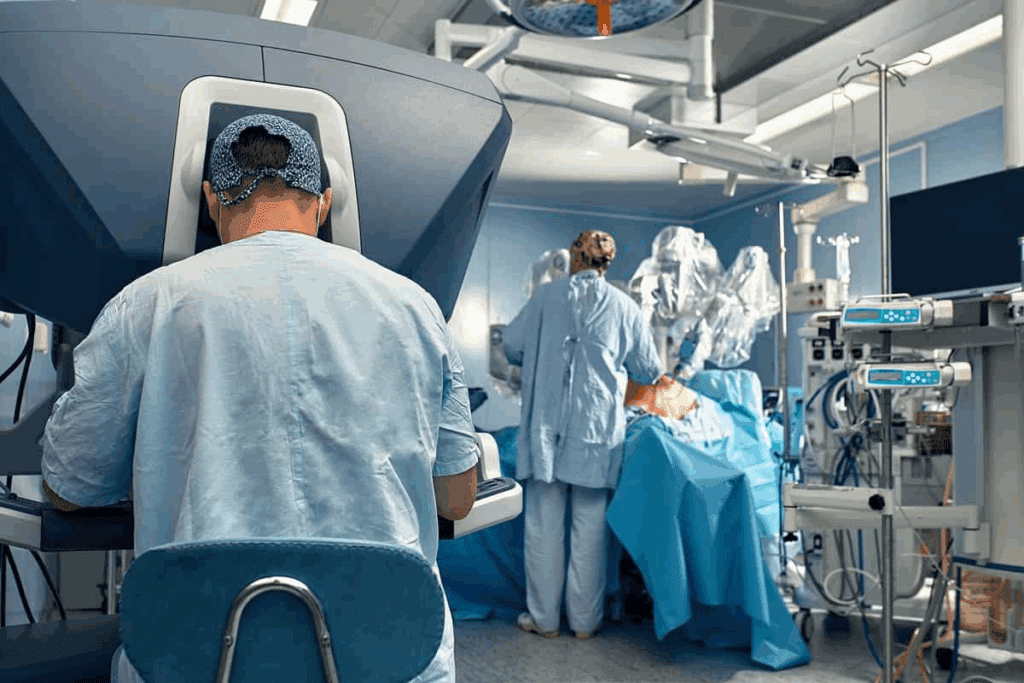
The da Vinci Surgical System in Gynecology
The da Vinci Surgical System is a top choice for gynecology surgeries. It has been key in improving robotic-assisted surgery. It gives surgeons the tools to do complex surgeries with better precision and control.
The da Vinci System has many benefits. It offers improved visualization, enhanced dexterity, and reduced blood loss. Its 3D vision system gives a clear view of the surgical area. This helps surgeons avoid damaging important structures.
There have been big improvements in using the da Vinci System for hysterectomies. Many surgeons now see it as the best choice for robotic-assisted gynecology surgeries.
Is the Cervix Removed During a Robotic Hysterectomy?
When thinking about a robotic hysterectomy, many patients wonder if the cervix will be taken out. The answer varies based on several things. These include why the hysterectomy is needed, the patient’s health, and the surgeon’s choice of method.
Factors Determining Cervix Removal
Several factors decide if the cervix will be removed during a robotic hysterectomy. These include the medical reason for the surgery, the patient’s health history, and the surgeon’s opinion.
- The type of hysterectomy needed (total, supracervical, or radical)
- Any cervical or uterine issues
- The patient’s plans for future pregnancies and age
- The surgeon’s advice based on the patient’s situation
It’s important for patients to understand these factors to make the best choice for their care.
The Surgical Decision-Making Process
The process of deciding on a robotic hysterectomy involves a detailed look at the patient’s health and the pros and cons of removing or keeping the cervix. Our surgeons team up with patients to find the best surgical plan.
| Surgical Approach | Cervix Removal | Considerations |
| Total Hysterectomy | Yes | Removal of uterus and cervix; often recommended for conditions like uterine cancer |
| Supracervical Hysterectomy | No | Cervix preserved; may be chosen for certain benign conditions |
| Radical Hysterectomy | Yes | Removal of uterus, cervix, and surrounding tissue; typically performed for cancer treatment |
Talking with their surgeon about these options helps patients understand what to expect during their robotic hysterectomy.
Robotic Total Hysterectomy: Procedure and Cervix Removal
Robotic total hysterectomy is a new way to remove the uterus and cervix. It uses the da Vinci Surgical System. This system gives surgeons better vision, precision, and control.
Surgical Technique and Approach
The surgery starts with small ports in the abdomen. The robotic arms go through these ports. The surgeon controls them from a console, using a 3D camera.
The key steps in the surgical technique include:
- Preparation of the patient and insertion of uterine manipulator
- Docking of the robotic system and insertion of robotic instruments
- Dissection and removal of the uterus and cervix
- Vaginal cuff closure
| Step | Description | Benefits |
| 1. Preparation | Patient is prepared, and uterine manipulator is inserted | Ensures proper positioning and access |
| 2. Docking | Robotic system is docked, and instruments are inserted | Provides precise control and visualization |
| 3. Dissection | Uterus and cervix are dissected and removed | Minimally invasive with less blood loss |
| 4. Vaginal Cuff Closure | Vaginal cuff is closed after cervix removal | Secure closure to prevent complications |
Vaginal Cuff Closure After Cervix Removal
Closing the vaginal cuff is a key part of the surgery. After removing the cervix, the cuff must be closed to avoid bleeding or prolapse. The robotic system helps with precise suturing, making the closure strong and durable.Robotic-assisted surgery is getting better. Patients now have less pain, shorter hospital stays, and can get back to normal faster.
Robotic Supracervical Hysterectomy: The Cervix Preservation Option
Now, it’s possible to keep the cervix during a hysterectomy with robotic supracervical hysterectomy. This method is both precise and minimally invasive. It has become a focus in gynecology because of its benefits for patients needing a hysterectomy.
Procedure Details and Technique
Robotic supracervical hysterectomy removes the upper part of the uterus but keeps the cervix. It uses the da Vinci Surgical System for better visualization and control. This system helps in a more detailed dissection and removal of uterine tissue, possibly lowering complication risks.
The process starts with small incisions in the abdomen for the robotic arms. The surgeon controls these arms from a console, using 3D visualization. The precision of the robotic system allows for careful separation and removal of the uterus, keeping the cervix intact.
Benefits and Considerations of Cervix Preservation
Keeping the cervix during hysterectomy can offer several advantages. It may improve sexual function and lower the risk of certain complications. Studies suggest it could also help in keeping the pelvic floor strong, reducing prolapse risk.
- Potential benefits of cervix preservation include improved sexual satisfaction and reduced risk of pelvic organ prolapse.
- The decision to preserve the cervix should be made on a case-by-case basis, considering factors such as the patient’s overall health, the reason for the hysterectomy, and the surgeon’s professional judgment.
But, it’s important to consider the risks and other factors. Patients should talk to their healthcare provider about their situation and the implications of cervix preservation. This way, they can make an informed choice.
Robotic Radical Hysterectomy for Cancer Treatment
Robotic radical hysterectomy is a big step forward in treating gynecologic cancers. It’s key for those with cervical or uterine cancer. Surgery is a big part of their treatment.
When Radical Hysterectomy Is Necessary
Radical hysterectomy is needed when cancer is found and needs to be removed thoroughly. This surgery is often suggested for early cervical cancer or some uterine cancers. It’s for cancers that can be taken out by surgery.
Choosing radical hysterectomy is a big decision. It depends on the cancer’s stage, the patient’s health, and if they want kids. We talk with patients to understand their needs and wishes.
Extent of Tissue Removal Beyond the Cervix
In a radical hysterectomy, more than just the cervix is removed. This includes the uterus, cervix, part of the vagina, and sometimes lymph nodes. It depends on how far the cancer has spread.
The robotic system helps remove these tissues carefully. This is important to avoid harming other areas. It also helps patients recover faster.
Surgical Precision in Cancer Treatment
Being precise in surgery is very important in cancer treatment. It affects how well the surgery works and the patient’s future. The robotic system helps surgeons be more accurate.
Robotic radical hysterectomy has many benefits. It means less blood loss, less pain, and a shorter stay in the hospital. These help patients recover more comfortably and quickly.
Ovarian Removal During Robotic Hysterectomy
Deciding to remove ovaries during a robotic hysterectomy is complex. It depends on the patient’s age, medical history, and the surgery’s reason.
Oophorectomy: When and Why
Oophorectomy, or removing one or both ovaries, might happen during a robotic hysterectomy. Reasons include ovarian cysts, cancer, or other issues. It’s also done to lower ovarian cancer risk in high-risk women.
Reasons for Oophorectomy:
- History of ovarian cysts or cancer
- High risk of ovarian cancer
- Presence of ovarian pathology
- Menopausal status
Hormonal Implications of Ovary Removal
Ovarian removal during a robotic hysterectomy has big hormonal effects, mainly for premenopausal women. It causes immediate menopause, leading to hot flashes, night sweats, and vaginal dryness. It also affects bone density, raising osteoporosis risk.
Hormone replacement therapy (HRT) might be suggested to ease these symptoms and prevent long-term health issues.
Preserving Ovaries While Removing the Uterus
In some cases, ovaries can be saved during a robotic hysterectomy. This is key for premenopausal women, as it keeps hormonal balance and reduces menopausal symptoms.
| Consideration | Oophorectomy | Ovarian Preservation |
| Hormonal Impact | Immediate menopause | Maintains hormonal balance |
| Menopausal Symptoms | Severe symptoms likely | Fewer symptoms |
| Bone Density | Increased risk of osteoporosis | Lower risk of osteoporosis |
The choice to remove or keep ovaries during a robotic hysterectomy is made with a healthcare provider. It considers the patient’s health needs and preferences.
Medical Indications for Cervix Removal
It’s important for patients to know why they might need to have their cervix removed. This choice is based on their health and the type of surgery they need.
Cervical Cancer and Precancerous Conditions
Cervical cancer or precancerous conditions often mean the cervix needs to be removed. If someone has cervical cancer, taking out the cervix is a key part of treatment. This might include a radical hysterectomy, which also removes the uterus and nearby tissues.
For cervical cancer, surgery like a robotic hysterectomy is used. It’s a precise way to treat the cancer. The choice to remove the cervix depends on the cancer’s stage and how severe it is.
Uterine Cancer Considerations
When it comes to uterine cancer, whether to remove the cervix depends on the cancer’s spread. If the cancer has reached the cervix or might, removing it is often advised. Uterine cancer surgery usually means taking out both the uterus and cervix.
Hysterectomy outcomes, including cervix removal, are usually good. This is even more true with robotic surgery. It offers better precision and fewer complications.
Non-Cancer Reasons for Cervix Removal
Not all reasons for removing the cervix are related to cancer. Other non-cancerous issues like severe cervical dysplasia, chronic pain, or damage might also require it. Sometimes, the decision to remove the cervix is made during surgery if unexpected problems arise.
The type of hysterectomy affects whether the cervix is removed. Knowing the differences helps patients make better choices about their care.
Benefits of Robotic-Assisted Surgery in Gynecology
Robotic-assisted surgery has changed gynecology for the better. It offers many benefits for those having hysterectomies. This technology improves results, cuts down recovery time, and boosts patient happiness.
Enhanced Surgical Precision and Control
Robotic surgery brings enhanced precision and control to the table. It lets surgeons do complex tasks with better accuracy. This reduces risks and improves patient results.
The tech behind it lets surgeons make very precise moves. This is key in delicate surgeries. It also helps in keeping more of the body’s tissues and organs intact.
Minimized Scarring and Reduced Blood Loss
Robotic surgery is minimally invasive. This means it causes less scarring and less blood loss than old-school surgery. The small cuts lower infection risks and speed up healing.
The system’s advanced tools also cut down on blood loss. This means fewer blood transfusions and less chance of complications after surgery.
Improved Visualization and Access
The robotic system offers better visualization and access to the surgery area. It makes complex surgeries easier. The 3D high-definition view lets surgeons see and work on the area clearly.
| Benefits | Robotic-Assisted Surgery | Traditional Surgery |
| Surgical Precision | High | Moderate |
| Scarring | Minimal | Significant |
| Blood Loss | Reduced | Higher |
| Recovery Time | Faster | Longer |
Recovery After Robotic Hysterectomy With and Without Cervix Removal
Knowing how to recover after a robotic hysterectomy is key. This includes knowing the difference between removing or keeping the cervix. Both choices affect how you feel after surgery.
Immediate Post-Operative Experience
Right after surgery, you’ll go to the recovery room. Here, doctors watch for any bad reactions to the anesthesia or surgery. The robotic method usually means less pain than traditional surgery. But, some pain is normal, and doctors will help manage it.
Key aspects of the immediate post-operative experience include:
- Managing post-operative pain effectively
- Monitoring for any signs of complications
- Gradually resuming normal activities
Recovery Timeline Differences
How long it takes to recover can change based on the cervix’s status. If the cervix is kept, the recovery might be a bit different. This is because the surgery is slightly different.
Factors influencing the recovery timeline include:
- The extent of the surgery
- The patient’s overall health and age
- Any complications that arise during or after surgery
Return to Normal Activities and Work
Most people can get back to normal in 4 to 6 weeks after robotic hysterectomy. But, this can change based on your health, the surgery’s complexity, and your job. Always listen to your surgeon’s advice on what to do and when.
Tips for a smooth recovery include:
- Following a balanced diet to aid healing
- Staying hydrated
- Gradually increasing physical activity
Potential Risks and Complications
It’s important to know the risks and complications of robotic hysterectomy. This surgery is precise and has quick recovery times. But, it’s key to understand the possible issues that can happen.
General Surgical Risks of Robotic Procedures
Robotic hysterectomy, like any surgery, has risks like infection and bleeding. The robotic system’s precision helps, but some risks stay the same. For example, it can reduce blood loss but also has tech-related risks like equipment failure.
Surgeons get a lot of training, and teams follow strict rules. Knowing these risks helps keep patients safe.
Specific Risks Related to Cervix Removal
Choosing to remove the cervix during hysterectomy changes the risk for the patient. It might make recovery faster but could also raise the risk of vaginal cuff dehiscence. This is a serious issue where the vaginal incision opens up again.
Doctors use special techniques to lower this risk. It’s important for patients to talk to their surgeon about their specific risks and what removing the cervix means for them.
Long-Term Health Considerations
After robotic hysterectomy, there are long-term health things to think about. Removing the ovaries can lead to early menopause. Women might need hormone therapy to handle menopause symptoms.
Also, there are long-term effects of removing the cervix versus keeping it. Some studies say keeping the cervix might lower the risk of pelvic organ prolapse.
| Complication | Cervix Removal | Cervix Preservation |
| Vaginal Cuff Dehiscence | Possible | Less Likely |
| Pelvic Organ Prolapse | Potential Risk | Potentially Lower Risk |
| Early Menopause | Dependent on Ovary Removal | |
Talking to a healthcare provider about these points helps patients make choices that fit their health and personal wishes.
Patient Considerations When Choosing Hysterectomy Type
When thinking about a hysterectomy, patients must consider many things. They need to pick the right type for their situation. This means understanding the different types of hysterectomies and what each offers.
Age and Reproductive Status Factors
A patient’s age and if they can have more kids are key in picking a hysterectomy type. Women who are done having kids might have more options than those who want more children. We look at these factors to give care that fits each patient.
For example, a total hysterectomy might be best for older women or those with cervical issues. On the other hand, a supracervical hysterectomy could be better for younger women or those who want to keep their cervix.
Sexual Function and Quality of Life
Sex life and overall happiness are also important. Studies show that the type of hysterectomy can affect these areas. We talk to patients about these topics to help them make good choices.
- The effect on sex life varies by hysterectomy type.
- Keeping the cervix might help some, but not all, patients.
- How happy you’ll be after surgery can depend on the surgery’s extent and your health.
Personal Preferences and Values in Decision-Making
What matters to each patient is also important. We listen to what patients value and what they’re worried about. This way, we can tailor their care to meet their unique needs.
| Consideration | Factors Influencing Decision | Potential Outcomes |
| Age and Reproductive Status | Childbearing plans, age-related health | Choice between total and supracervical hysterectomy |
| Sexual Function | Cervix preservation, nerve-sparing techniques | Impact on sexual satisfaction and pleasure |
| Personal Preferences | Individual values, lifestyle considerations | Tailored approach to hysterectomy and post-operative care |
By carefully thinking about these factors, patients and doctors can make smart choices about hysterectomies. We aim to support our patients every step of the way. This ensures they get care that’s just right for them.
Discussing Your Options With Your Gynecologic Surgeon
Talking to your gynecologic surgeon about a robotic hysterectomy is key. This talk helps you understand your choices. It’s important to know all about the surgery and what it means for you.
Your surgeon is your main source of info and your care partner. You can explore the good and bad of robotic hysterectomy together. This way, you both understand the surgery better.
Essential Questions to Ask Before Surgery
It’s smart to have questions ready for your talk. Here are some important ones to ask your surgeon:
- Why do you think a robotic hysterectomy is best for me?
- Will my cervix be taken out, and why is that?
- What risks or problems could happen during or after surgery?
- How will the robotic tools be used during my surgery?
- How long will I need to recover, and what should I do to get ready?
These questions can clear up any doubts you have. They help you get ready for the surgery and recovery.
The Shared Decision-Making Process
Choosing to have a robotic hysterectomy is a big decision. You should be involved in this choice. Your surgeon will help guide you, using their knowledge and advice.
You and your surgeon will look at the good and bad sides of the surgery. You’ll think about your health, why you need the surgery, and what you prefer. This way, you make a choice that feels right for you.
Talking openly with your surgeon helps you make good choices about your health. This way, you can get the best care for your well-being.
Conclusion: Making an Informed Decision About Robotic Hysterectomy
Exploring robotic hysterectomy surgery shows how important it is to make informed choices. Knowing about different hysterectomy types and the role of the cervix is key. This knowledge helps patients choose what’s best for their health and personal wishes.
Robotic hysterectomy has many advantages, like better precision and less scarring. But, whether to remove the cervix depends on the medical condition and the patient’s health.
We urge patients to talk openly with their gynecologic surgeon. Asking the right questions helps understand options and outcomes of robotic hysterectomy. This way, patients can make choices that improve their health and life quality.
FAQ
What is a robotic hysterectomy?
A robotic hysterectomy is a surgery that uses the da Vinci Surgical System. It removes the uterus and sometimes other organs. This method is precise and controlled.
Is the cervix removed during a robotic hysterectomy?
Whether the cervix is removed depends on the medical reason and the patient’s health. Sometimes, the cervix is taken out, and sometimes it’s not. This choice is made based on the situation.
What are the benefits of robotic-assisted surgery in gynecology?
Robotic surgery in gynecology has many benefits. It offers better precision, less scarring, and less blood loss. It also makes it easier to see what’s happening during surgery.
These advantages can lead to a quicker recovery and less pain after surgery. It also lowers the risk of complications.
How long does it take to recover from a robotic hysterectomy?
The recovery time from a robotic hysterectomy varies. It depends on the patient’s health, age, and how extensive the surgery was. Generally, people can get back to normal in 4-6 weeks.
But, recovery times can be shorter or longer based on individual factors.
Will I experience hormonal changes after ovarian removal during a robotic hysterectomy?
If the ovaries are removed, hormonal changes may occur. This is because the ovaries stop producing hormones suddenly. But, if the ovaries are left in, hormonal changes are unlikely.
The choice to remove or keep the ovaries is made with the surgeon. They consider the patient’s medical history and individual factors.
Can I discuss my personal preferences and values with my gynecologic surgeon before a robotic hysterectomy?
Yes, it’s important to talk to your surgeon about your preferences and values before surgery. This ensures your care meets your needs and priorities.
What are the possible risks and complications of robotic hysterectomy?
Robotic hysterectomy, like any surgery, has risks and complications. These include general surgical risks and risks specific to cervix removal. Your surgeon will discuss these with you in detail.
This helps you make an informed decision about your care.
How does the da Vinci Surgical System enhance the precision of robotic hysterectomy?
The da Vinci Surgical System is a cutting-edge robotic platform. It offers better visualization, precision, and control during surgery. Its tools and 3D view help surgeons perform complex tasks with more accuracy.
This reduces the risk of complications and improves outcomes.
Reference:
- Cambridge University Hospitals. Patient Information on Bladder Care and Management (includes impact of surgeries like hysterectomy), https://www.cuh.nhs.uk/patient-information/bladder-care-and-management
2. Medical News Today. Article on bladder emptying techniques and implications of pelvic surgeries including hysterectomyhttps://www.medicalnewstoday.com/articles/316706
























