Last Updated on November 27, 2025 by Bilal Hasdemir

Prostate cancer is a big health issue for men all over the world. Prostate cancer surgery is a common way to treat it.
Robotic prostatectomy surgery is a precise and less invasive way to treat prostate cancer. It involves removing the prostate gland. Many patients wonder if the urethra is cut during this surgery.
We know you have questions. We’ll answer them directly. This will help you understand what to expect during robotic prostatectomy surgery.
Key Takeaways
- Robotic prostatectomy is a precise treatment for prostate cancer.
- The procedure involves removing the prostate gland.
- Understanding the surgical process can alleviate concerns.
- The urethra’s involvement during surgery is a common query.
- Clarity on the surgical details can help patients prepare.
The Fundamentals of Prostate Cancer Treatment
It’s important for patients and their families to understand prostate cancer treatment. This disease is a big concern for men. It can be treated in many ways, from watching it closely to surgery.
Prevalence of Prostate Cancer in the United States
Prostate cancer is very common in men in the United States. Every year, over 200,000 men are diagnosed. Knowing about it and its treatments is key.
Treatment Options Overview
Choosing a treatment for prostate cancer depends on several things. These include the cancer’s stage, the patient’s health, and their wishes. Treatments range from watching it closely to surgery, like robotic prostatectomy. Each option has its own benefits and risks.
Robotic prostatectomy is a popular choice because it’s precise and has less recovery time. It removes the prostate gland. It’s often chosen for men with early-stage cancer.
Why Surgical Intervention May Be Necessary
Surgery, like removing the prostate, might be needed for some men. The decision to have surgery is made after talking with a doctor. Surgery tries to remove the cancer while keeping other tissues safe.
The type of surgery, like robotic-assisted, depends on the doctor and the patient’s situation. Knowing about surgery’s role in treatment helps make better choices.
Understanding Robotic Prostatectomy Surgery
Robotic prostatectomy surgery is a big step forward in treating prostate cancer. It’s a less invasive option that might lead to fewer complications. This method uses a robotic system to help surgeons remove the prostate gland with better precision.
What is a Robotic-Assisted Radical Prostatectomy
A robotic-assisted radical prostatectomy is a detailed surgery to remove the prostate gland and affected tissues. It’s done with a robotic system for robotic surgical precision. This makes it easier to remove the prostate accurately.
The surgery uses small incisions in the abdomen for the robotic arms. A surgeon controls these arms from a console, getting a clear 3D view of the area. The robotic system makes the surgeon’s hand movements exact, making delicate tasks easier.
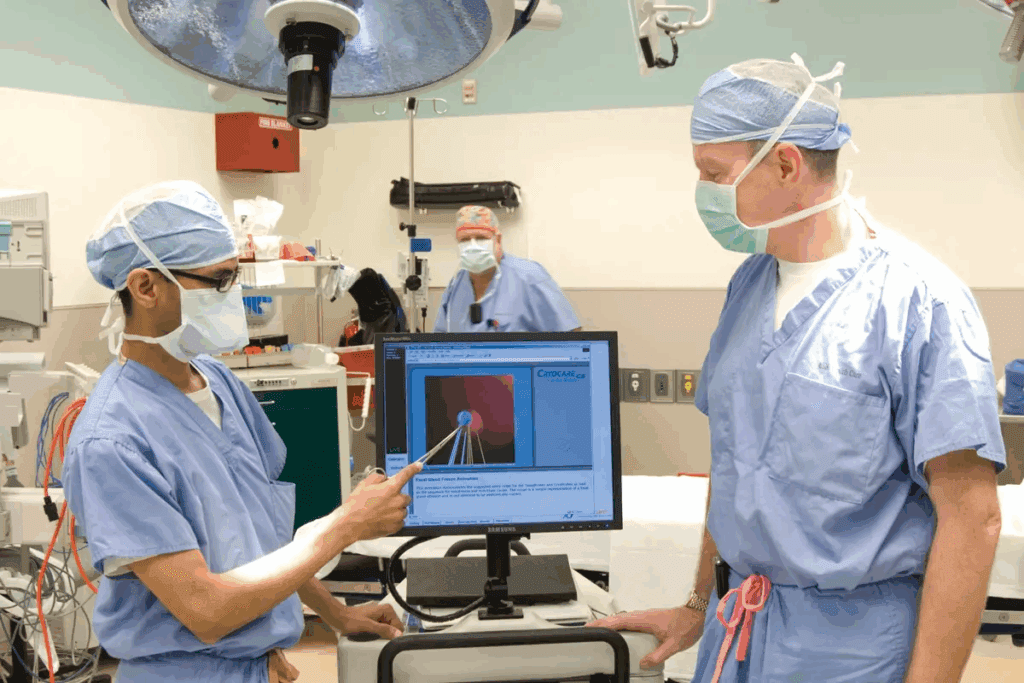
The Da Vinci Surgical System Explained
The Da Vinci Surgical System is a top-notch robotic platform for prostatectomy surgeries. It offers better visualization, precision, and control. It has a surgeon’s console, a cart with four robotic arms, and a 3D vision system.
This technology helps with nerve sparing techniques more accurately. This can lead to better urinary and sexual function after surgery. The system’s design makes complex surgeries simpler for surgeons.
Key Benefits of Minimally Invasive Approach
The robotic-assisted prostate surgery has many benefits. It includes smaller incisions, less blood loss, and a lower risk of infection. It also means less pain after surgery compared to open surgery.
Also, the robotic system’s precision can lead to better cancer control. Patients often have shorter hospital stays and recover faster. This means they can get back to their daily activities sooner.
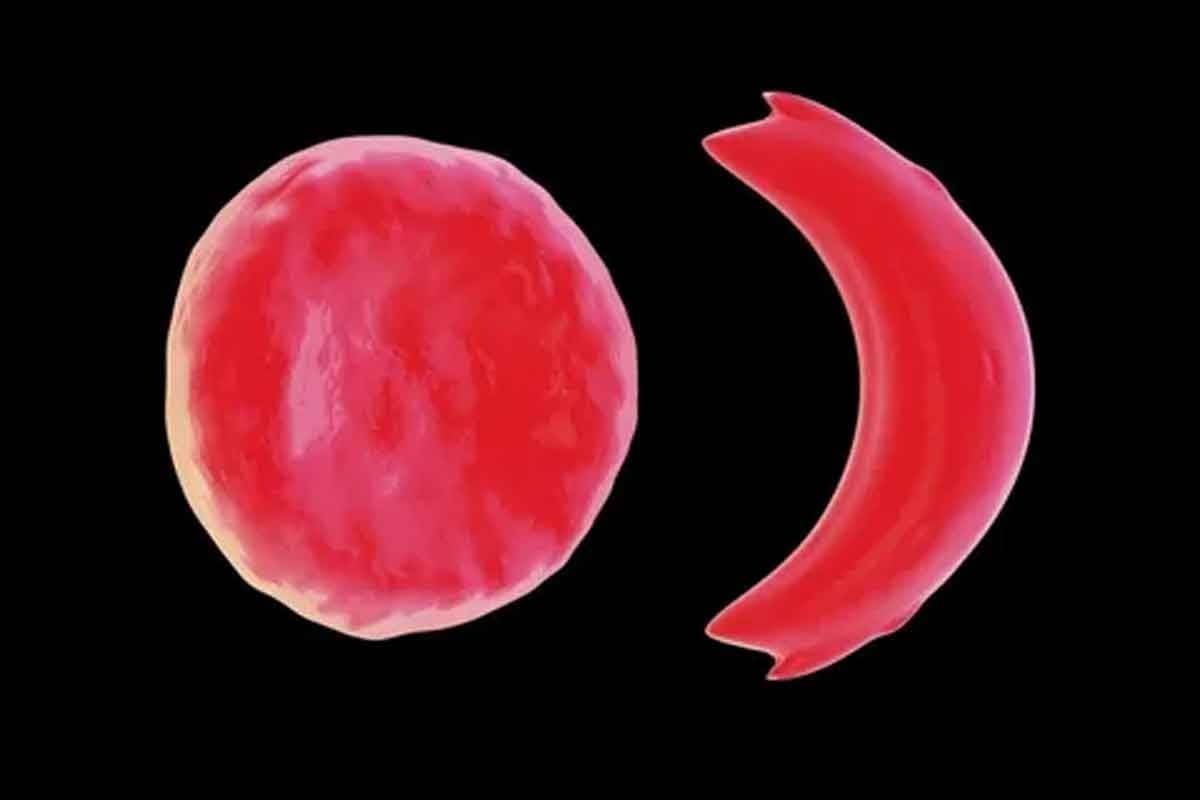
Anatomy of the Prostate and Urinary System
It’s important to know how the prostate and urinary system work. This helps us understand robotic prostatectomy surgery better. The prostate gland is key to the male reproductive system. It’s close to the urethra, making it a focus during surgery.
Prostate Location and Function
The prostate gland is below the bladder and wraps around the urethra. The urethra carries urine out of the body. The prostate makes seminal fluid, which helps sperm during ejaculation. The prostate’s location near the urethra and bladder neck is very important.
The Relationship Between Prostate and Urethra
The urethra goes through the prostate gland. This is why their connection is so important. During a pelvic surgical procedure like robotic prostatectomy, keeping the urethra safe is key. The urethral anastomosis site needs careful surgery to heal well and keep urine flowing right after surgery.
| Anatomical Structure | Function | Relation to Prostatectomy |
| Prostate Gland | Produces seminal fluid | Removed during prostatectomy |
| Urethra | Canal for urine and semen | Preserved and reconnected during surgery |
| Bladder | Stores urine | Connected to urethra; neck dissected during prostatectomy |
Understanding the Male Urinary Tract
The male urinary tract includes the kidneys, ureters, bladder, and urethra. The urethra is key for urine to leave the body. Knowing the urinary tract’s anatomy helps us see the challenges of urethral anastomosis in robotic prostatectomy.
Understanding the prostate, urethra, and their surroundings helps us see the need for precision in pelvic surgery.
The Surgical Approach to the Urethra During Prostatectomy
Robotic prostatectomy is a precise surgery that aims to remove cancer while keeping urinary function intact. We will look into the key aspects of this technique.
Surgical Access Points and Port Placement
The success of robotic prostatectomy starts with the right placement of surgical ports. These access points help surgeons work with great precision. The setup includes a camera port and others for instruments. Precise port placement is key for the best access to the prostate and urethra.
Bladder Neck Dissection Techniques
Dissecting the bladder neck is a vital part of prostatectomy. This step involves carefully separating the bladder from the prostate. Advanced imaging and robotic precision help surgeons do this delicate task with little harm to nearby tissues. The aim is to keep the bladder neck intact while removing the prostate completely.
| Technique | Description | Benefits |
| Bladder Neck Preservation | Careful dissection to maintain bladder neck integrity | Improved urinary continence |
| Prostate Removal | Precise separation of prostate from surrounding tissues | Reduced risk of cancer recurrence |
| Urethral Sparing | Minimal disruption to urethral structures during surgery | Faster recovery of urinary function |
Urethral Management During Surgery
Managing the urethra well is key during prostatectomy. This includes the initial dissection and the later reconstruction. Surgeons must balance removing cancer with keeping urethral function. Techniques like urethral sparing and precise anastomosis are essential for good results.
By using advanced surgical methods and robotic systems, we can achieve a good balance between removing cancer and preserving function.
Is the Urethra Actually Cut During Surgery?
Many patients wonder about the urethra during robotic prostatectomy. The urethra is key to our urinary system. Its care during surgery is very important.
The Technical Answer to Urethral Handling
During robotic prostatectomy, the urethra isn’t cut off completely. Instead, it’s handled with care. Surgeons use advanced methods to keep the urethra and its surroundings intact. This helps keep urinary function as normal as possible.
The surgery involves a disconnection of the urethra from the prostate. This is different from just cutting it. Knowing this helps us understand the surgery better.
Disconnection vs. Cutting: Understanding the Difference
Disconnection and cutting are not the same in robotic prostatectomy. Disconnection means the urethra is carefully separated from the prostate. This way, as much of the urethra’s length and function is kept as possible.
- Disconnection gives surgeons more control over the urethral stump.
- It helps keep the urethral sphincter intact, lowering the chance of bladder control issues.
- This method leads to better urinary continence after surgery.
Modern Preservation Techniques
Modern preservation techniques are key to keeping the urethra intact during robotic prostatectomy. These include:
- Advanced imaging to see the urethral anatomy clearly.
- Precision surgery to avoid damage to nearby tissues.
- Nerve-sparing techniques to keep urinary function intact.
Using these modern preservation techniques, surgeons can greatly improve patient results. This reduces the chance of complications and helps patients recover faster.
The Urethral Anastomosis Process
After removing the prostate gland, reconnecting the urinary pathway is key. This step, called urethral anastomosis, is vital for urine flow to return to normal.
Reconnecting the Urinary Pathway
Urethral anastomosis reconnects the urethra to the bladder neck. This is essential for the urinary tract’s continuity. We use advanced suturing techniques for a strong and precise connection.
The robotic system helps with better vision and control. This makes the surgery less invasive and speeds up recovery.
Advanced Suturing Techniques
The success of urethral anastomosis depends on the suturing method. We use continuous suturing or interrupted suturing based on the patient’s needs. Choosing the right technique is key for a watertight closure and preventing leaks.
Our surgeons are up-to-date with the latest suturing methods. Robotic assistance helps us make a secure and leak-free connection.
Ensuring Watertight Closure
A watertight closure is critical for the anastomosis’s success. We place sutures carefully and test for leaks. The robotic system’s magnification and precision tools are essential for checking the anastomosis’s integrity.
After surgery, a catheter placement procedure is done to keep the urinary tract open during healing. The catheter is removed after a few weeks, once the anastomosis has healed well.
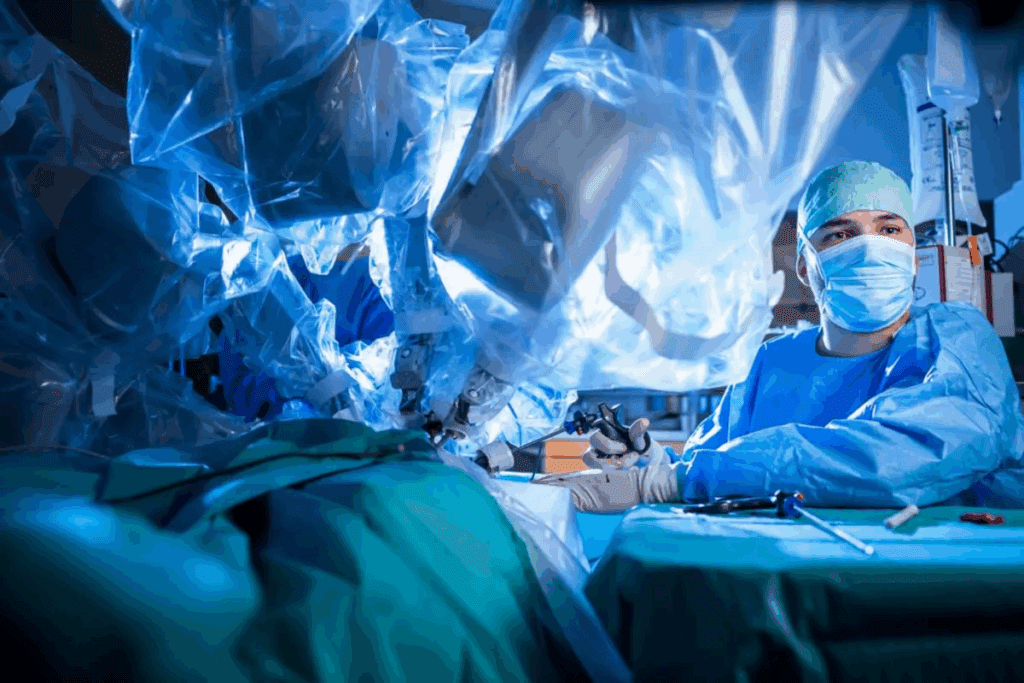
Advantages of Robotic Prostatectomy Surgery for Urethral Preservation
Robotic prostatectomy has changed how we treat prostate cancer. It helps keep the urethra safe and makes recovery faster. This new surgery method has greatly improved treatment results.
Enhanced Visualization of Urethral Structures
The robotic system gives surgeons a clear, 3D view of the area. This enhanced visualization is key for seeing and saving the nerves and tissues around the urethra. These are important for keeping urine flow steady.
Precision in Anastomosis Creation
Robotic prostatectomy allows for precise anastomosis creation. This is very important for fixing the urinary tract. The robotic tools help make a tight seal between the bladder and urethra. This reduces the chance of problems and helps with a quicker recovery.
Benefits for Long-term Urinary Function
The better view and precise work in robotic prostatectomy help with long-term urinary function. Research shows patients do better and recover faster with this method. This is because it’s less invasive and the urethral tissues are handled carefully.
| Benefits | Robotic Prostatectomy | Traditional Prostatectomy |
| Visualization | High-definition, 3D view | Limited, 2D view |
| Precision in Anastomosis | High precision with wristed instruments | Lower precision, more manual dexterity required |
| Continence Recovery | Faster recovery timeline | Slower recovery timeline |
In summary, robotic prostatectomy is a big step forward for urethral preservation. It offers better visualization, precise work, and better long-term urine control. These advantages lead to a better prostatectomy healing process and better results for patients.
Urethral Sphincter Preservation Techniques
Keeping the urethral sphincter intact is key for good results in prostate surgery. This part of the body is important for controlling when we pee. It’s a big deal during robotic prostatectomy.
Importance of Sphincter Function for Continence
The urethral sphincter helps us stay dry. If it gets hurt during surgery, we might leak urine. This can really change how we live. So, keeping the urethral sphincter safe is very important.
Anatomical Considerations During Surgery
When doing robotic prostatectomy, surgeons have to think about the urethral sphincter’s location. This area is very sensitive. They need to be very careful to not hurt it.
Knowing how the prostate, urethra, and other parts around them work is key. This knowledge helps them keep the sphincter safe.
Technological Tools for Sphincter Identification
Tools like high-definition imaging and nerve-sparing methods help surgeons find and keep the urethral sphincter safe. These tools let them see better and work more precisely.
Using the latest technology and careful surgery, we can make sure patients do well after robotic prostatectomy. Focusing on keeping the urethral sphincter safe shows how surgery is getting better. It helps patients recover faster and with fewer problems.
Post-Surgical Catheterization Requirements
After robotic prostatectomy surgery, patients need to use a urinary catheter. This is a big concern for many. It’s important to know why it’s needed, how long it stays in, and how to take care of it at home.
Why a Urinary Catheter is Necessary
A urinary catheter helps the urethral anastomosis heal after surgery. This is the connection between the bladder and urethra. It lets urine drain while the area heals, avoiding leaks or blockages.
Typical Duration of Catheterization
The time a catheter stays in can vary. Usually, it’s 1 to 2 weeks after surgery. It’s key to follow the doctor’s catheter management advice to avoid infections and help the bladder heal.
Catheter Management and Care at Home
At home, it’s important to keep the catheter area clean. Patients should learn how to clean the site, secure the catheter, and watch for infection signs. We offer detailed catheter care tips to help with recovery.
By understanding catheter use and following care tips, patients can reduce risks. This supports their urinary function recovery after surgery.
Recovery of Urinary Function After Surgery
Understanding how urinary function recovers after robotic prostatectomy is key. The process is complex and varies greatly among people.
Timeline for Continence Recovery
The time it takes to regain urinary control can differ a lot. Most people see some improvement in the first few months. But, full recovery might take up to a year or more for some.
Key milestones in the continence recovery timeline include:
- Initial improvement within 3-6 months
- Significant progress by 6-12 months
- Potential for continued improvement beyond 1 year
Factors Affecting Urinary Control
Many factors can affect how well you recover urinary control. These include your age, health, and any pre-existing urinary issues.
The surgical technique and the surgeon’s experience also play a big role in the outcome. Post-operative care and rehabilitation practices also greatly impact recovery.
Pelvic Floor Exercises and Rehabilitation
Pelvic floor exercises, or Kegel exercises, are vital in post-operative care. They help strengthen muscles that support urinary control.
A good pelvic floor rehabilitation program can greatly improve urinary function recovery. It’s important to start these exercises early, with guidance from a healthcare professional.
Potential Complications Related to Urethral Surgery
It’s important for patients to know about the risks of urethral surgery, like robotic prostatectomy. This surgery is advanced and minimally invasive. But, there are risks to the urethra that can affect recovery and long-term urinary function.
Causes and Management of Anastomotic Leakage
Anastomotic leakage is a serious issue after robotic prostatectomy. It happens when urine leaks from the connection between the bladder and urethra. Causes include tension, poor suturing, or slow healing. Treatment often involves keeping a catheter in longer and sometimes more surgery.
Stricture Formation and Its Treatment
Stricture formation is another risk. It’s when the urethra narrows due to scar tissue. Symptoms include weak urine flow and trouble urinating. Treatment can range from simple procedures like dilation to more complex surgeries.
Incontinence Issues: Short and Long-term
Incontinence is a common worry after robotic prostatectomy. Short-term incontinence is often due to swelling and trauma. Long-term incontinence can be from permanent damage. Pelvic floor exercises and treatments like sling procedures can help manage it.
| Complication | Causes | Management/Treatment |
| Anastomotic Leakage | Tension on anastomotic site, poor suturing, inadequate healing | Prolonged catheterization, additional surgery |
| Stricture Formation | Scar tissue at anastomotic site | Dilation, surgical revision |
| Incontinence | Swelling/trauma to urethral sphincter, nerve damage | Pelvic floor exercises, sling procedures, artificial sphincter |
It’s key for patients to talk to their healthcare provider about these risks. Understanding the risks and benefits helps patients prepare for recovery and make informed decisions.
Comparing Traditional vs. Robotic Prostatectomy Approaches
It’s important to know the differences between traditional and robotic prostatectomy. These methods treat prostate cancer in different ways. They also affect how well you can urinate after surgery.
Differences in Urethral Handling Techniques
Traditional open prostatectomy uses a big incision. This can hurt the urethra more. On the other hand, robotic prostatectomy uses the Da Vinci Surgical System. It allows for precise work and keeps the urethral sphincter safe.
The robotic method lets surgeons do detailed work with better control. This helps avoid damage to nearby tissues. It’s key for keeping urine control after surgery.
Outcomes for Urinary Function Preservation
Research shows robotic prostatectomy keeps urinary function better than traditional methods. The robotic system’s clear view and precision help in urinary reconstruction surgery.
| Aspect | Traditional Prostatectomy | Robotic Prostatectomy |
| Urethral Handling | More invasive, potentially causing greater trauma | Less invasive, with precise dissection |
| Urinary Continence | Higher risk of short-term incontinence | Better preservation of urinary continence |
| Recovery Time | Generally longer recovery period | Typically shorter recovery period |
Recovery Comparisons Between Approaches
Looking at recovery comparisons, robotic surgery has its advantages. It usually means a shorter hospital stay and less pain after surgery. This leads to a quicker recovery.
People who have robotic prostatectomy often get back to their normal life faster. This is great for those who are active or have important work to do.
Conclusion
Robotic prostatectomy is a cutting-edge surgery for prostate cancer. It offers many benefits to patients. We’ve looked into how it affects the urethra and urine function.
This surgery is precise, leading to better recovery times for patients. It shows how complex the procedure is. Patients can now understand the surgery better.
Robotic prostatectomy is getting better with time. It’s changing prostate cancer surgery for the better. Its minimally invasive nature and precision are setting new standards in care.
FAQ
What is robotic prostatectomy surgery?
Robotic prostatectomy surgery is a new way to treat prostate cancer. It uses a robotic system, like the Da Vinci Surgical System. This system helps doctors remove the prostate gland with great precision and care for the nerves.
Is the urethra cut during robotic prostatectomy?
During robotic prostatectomy, the urethra is carefully disconnected from the prostate rather than fully cut. Instead, it’s carefully disconnected from the prostate. This helps keep urinary function intact.
What is the purpose of urethral anastomosis during prostatectomy?
Urethral anastomosis reconnects the urinary pathway after removing the prostate gland. It’s done by suturing the urethra to the bladder neck. This ensures a tight seal and prevents leaks.
How long does it take to recover urinary function after robotic prostatectomy?
Recovery time for urinary function varies. Most people regain control within a few months after surgery. Exercises and rehabilitation can help speed up the process.
What are the benefits of robotic prostatectomy for urethral preservation?
Robotic prostatectomy offers better visualization and precise anastomosis creation. It also helps preserve nerves, leading to better long-term urinary function and continence recovery.
Why is a urinary catheter necessary after robotic prostatectomy?
A urinary catheter is needed after surgery to help the urethral anastomosis heal. It also ensures proper drainage. Most people use a catheter for 1-2 weeks.
What are the possible complications related to urethral surgery during prostatectomy?
Possible complications include leakage, stricture formation, and incontinence. These can be managed with proper treatment and care.
How does robotic prostatectomy compare to traditional prostatectomy in terms of urethral handling?
Robotic prostatectomy offers more precise handling and anastomosis creation. This results in better outcomes for preserving urinary function compared to traditional prostatectomy.
What techniques are used to preserve the urethral sphincter during robotic prostatectomy?
Techniques like nerve sparing and precise dissection are used. These help preserve the urethral sphincter, which is key for maintaining continence.
Can robotic prostatectomy surgery improve long-term urinary function?
Yes, robotic prostatectomy surgery can improve long-term urinary function. Its precise and nerve-sparing approach helps preserve the urethra and its surrounding structures.
Reference:
Robot-Assisted Radical Prostatectomy: A Step-by-Step Guide (NCBI, 2018)https://pmc.ncbi.nlm.nih.gov/articles/PMC6071518/
Complete urethral preservation in robot-assisted radical prostatectomy (NCBI, 2024)https://pmc.ncbi.nlm.nih.gov/articles/PMC11628903/