Last Updated on November 27, 2025 by Bilal Hasdemir

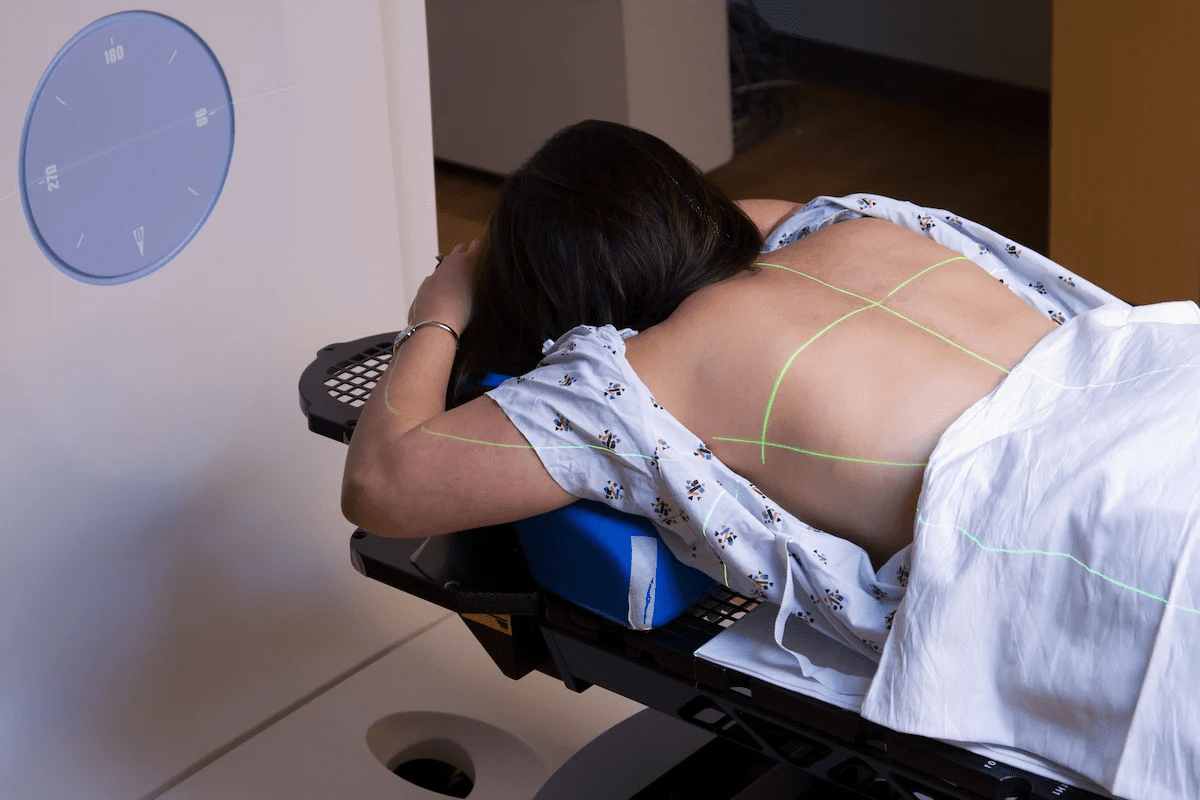
Robotic surgery has changed the medical world with its precise and small cuts. Over 1.2 million procedures were done worldwide in 2020. This shows how important it is to know both the good and bad sides of this new surgery method.
Robot-assisted surgery lets surgeons do complex tasks with better control and flexibility. But, like any surgery, it has its own challenges and downsides.
When we look at robotic surgery, we must compare its good points to its bad ones. This helps both patients and doctors understand it better.
Key Takeaways
- Robotic surgery offers enhanced precision and flexibility.
- Despite its benefits, robotic surgery has several disadvantages.
- Understanding these drawbacks is key for patients and healthcare professionals.
- Robotic surgery is used for many complex procedures.
- The technology keeps getting better, fixing some of its current problems.
The Current State of Robotic Surgery in Modern Medicine

Robotic systems have changed surgery a lot. Now, robotic surgery is used in many areas like urology, gynecology, and heart surgery. It’s becoming more common.
How Robotic Surgical Systems Function
Robotic surgery systems help surgeons do better work. They have a console, a cart for the patient, and a vision system. The console shows a clear 3D view of the area being worked on. The cart has robotic arms that move like the surgeon’s hands.
Key Components of Robotic Surgical Systems:
- Console: Provides the surgeon with a high-definition 3D view.
- Patient-side cart: Equipped with robotic arms that mimic the surgeon’s movements.
- Vision system: Enhances the visual clarity of the operating area.
A study in a Journal found that robotic systems make surgery more precise. This leads to better results for patients.
“Robotic surgery has the power to change surgery. It gives surgeons better views, precision, and control.”
Prevalence and Common Applications in the United States
In the U.S., robotic surgery is used a lot. Many hospitals use it to help patients. It’s used in urology for prostate surgeries, gynecology for hysterectomies, and heart surgery.
| Surgical Specialty | Common Procedures | Benefits of Robotic Surgery |
| Urology | Prostatectomies | Enhanced precision, less blood loss |
| Gynecology | Hysterectomies, endometriosis treatment | Minimally invasive, quicker recovery |
| Cardiothoracic Surgery | Complex heart procedures | Improved visualization, reduced trauma |
Robotic surgery is getting better. We’ll see new tech and techniques soon. It might be used in even more surgeries.
Financial Burdens: The High Cost of Robotic Surgery
Robotic surgery is innovative but comes with big costs for healthcare and patients. It needs a lot of money for the machines, upkeep, training, and running costs.
Capital Investment Requirements for Healthcare Facilities
The cost to start robotic surgery is huge, often in the millions. This includes the price of the machines and changes to the building. For small or poor hospitals, this is a big problem.
The cost is not just for the machines. It also includes training for doctors, which is key to using robotic surgery well.
Ongoing Operational and Maintenance Expenses
After buying the machines, there are ongoing costs. These include parts, maintenance, and updates. There are also costs for training new staff.
The ongoing operational expenses can hurt a hospital’s budget. Hospitals need to think about these costs before starting robotic surgery.
Patient Financial Impact and Insurance Coverage Limitations
Patients also face big financial challenges with robotic surgery. It can be more expensive than traditional surgery. Insurance might not cover it fully, leaving patients with big bills.
The high cost of robotic surgery can make it hard for some to access. Hospitals should talk about these costs with patients and find ways to help.
Technical Limitations and Mechanical Disadvantages
Robotic surgery is getting better, but it has its limits. These technical issues can affect how well procedures go.
Lack of Haptic Feedback for Surgeons
One big problem with robotic surgery is the lack of haptic feedback. This means surgeons can’t feel what they’re doing as they work. They have to rely on what they see, which can sometimes cause problems.
This issue is really tough in delicate surgeries. Surgeons need a lot of practice to get good at it.
Limited Range of Motion in Complex Anatomical Areas
Robotic systems can’t move as much as humans. This makes it hard to reach certain parts of the body. It’s a big problem in surgeries that need to get into tight spots.
To get around this, surgeons have to move the robotic arms a lot. This can make the surgery longer and riskier.
System Failures and Technical Malfunctions During Procedures
System failures and malfunctions are a big worry in robotic surgery. Even though they don’t happen often, they can be very serious. They might even mean the surgery has to stop or be done in a different way.
| Type of Malfunction | Frequency | Potential Impact |
| Robotic Arm Failure | Rare | Significant |
| System Software Glitch | Occasional | Moderate |
| Instrument Failure | Occasional | Moderate |
To avoid system failures, hospitals need to keep their systems up to date. Surgeons and their teams also need training on what to do in emergencies.
The Steep Learning Curve for Surgical Teams
Robotic surgery is a big challenge for surgical teams because it’s hard to learn. As we use more robotic-assisted surgery, we need to understand how to train teams well.
Training Requirements and Certification Challenges
Robotic surgery needs a lot of skill, so surgeons and their teams must get thorough training. These programs help surgeons know the robotic system well and handle its special needs. Certification challenges come from different training methods and the need for a common certification.
Training is complex, with both theory and practice. Surgeons go through a lot, like simulator training, watching experts, and getting hands-on experience. They must really get the complexity of robotic systems and how to use them.
Adaptation Difficulties for Experienced Traditional Surgeons
Experienced surgeons find it hard to switch to robotic-assisted surgery. They have to change their way of working, tools, and thinking. Adaptation difficulties come from missing haptic feedback, working from a console, and needing a team.
It takes time, effort, and a desire to learn new things to overcome these hurdles. It’s not just about learning the robotic system. It’s also about fitting it into their surgical work. With good training and support, surgeons can learn to use robotic-assisted surgery well.
Increased Operative Times: A Significant Drawback
Robotic surgery is precise and has changed surgery a lot. Butit has a big problem: it takes longer. This longer time affects the team and the healthcare system.
Extended Setup and Preparation Requirements
Setting up for robotic surgery takes a lot of steps. This includes docking the robot, getting the patient ready, and preparing tools. These steps are detailed and take more time than other surgeries.
The start of robotic surgery can really add to the time it takes. Making sure the robot is set up right and all tools are ready is key. But this careful setup can make the start of surgery longer.
Procedure Duration Compared to Laparoscopic and Open Surgery
Robotic surgery is longer than laparoscopic and open surgeries. It’s more precise and less invasive, but it takes more time. Studies show robotic surgeries are longer because of the setup.
The good things about robotic surgery, like less blood loss and quicker recovery, must be weighed against the longer time. We need to think about how these benefits compare to the longer time it takes.
In summary, robotic surgery has many benefits, but the longer time it takes is a big problem. Understanding why it takes longer can help make it more efficient and useful.
Complications Specific to Robotic Surgery Procedures
Robotic surgery can face complications from mechanical issues and patient factors. It’s key to grasp the unique aspects of these surgeries.
Mechanical Complications During Operations
Mechanical failures are rare but serious in robotic surgery. They can include system malfunctions or instrument failures. For example, a study found mechanical issues in about 0.4% of cases, mostly due to instrument problems.
Some mechanical issues are:
- Instrument breakage or malfunction
- System software or hardware failures
- Electrical issues within the robotic system
To reduce these risks, it’s vital to maintain and check the robotic equipment regularly. Also, having a backup plan for mechanical failures during surgery is essential.
Patient-Specific Complications and Risk Factors
Patient-specific factors greatly influence the risk of complications in robotic surgery. These include anatomical variations, health conditions, and past surgeries. For instance, severe obesity or previous abdominal surgeries can increase risks due to altered anatomy.
Some patient-specific complications and risks are:
- Anatomical variations that complicate robotic access
- Underlying health conditions, such as diabetes or cardiovascular disease, that affect healing
- Previous surgical interventions that result in adhesions or altered anatomy
Understanding these risks is critical for surgeons to choose patients wisely and plan to minimize risks. A detailed preoperative assessment is essential to spot possible complications early.
As we dive deeper into robotic surgery, it’s evident that technology has made great strides. Yet, there are challenges to overcome. By recognizing and understanding these complications, we can enhance the safety and success of robotic surgeries.
Accessibility Issues and Healthcare Disparities
Robotic surgery is becoming more common, but we face big challenges. We must make sure everyone has equal access to this new technology.
Geographic Distribution Limitations
In the United States, where you live affects your access to robotic surgery. Cities usually have more access, but rural areas are left behind. This is because robotic equipment is very expensive.
Rural areas struggle because they can’t afford the equipment. This creates a big problem for those living far from cities. It’s hard for rural hospitals to keep up with the costs.
Socioeconomic Barriers
Money and insurance also play a big part in who can get robotic surgery. If you can’t afford it or don’t have good insurance, it’s hard to get this treatment.
Robotic surgery might cost as much as traditional surgery. But for many, it’s just too expensive. We need better healthcare policies to help everyone.
We must find ways to make robotic surgery more available. This could include training more surgeons in rural areas. We also need policies that help more people get this treatment.
Comparing Robotic Surgery to Traditional Surgical Approaches
Looking at modern surgery, it’s key to compare robotic surgery to traditional methods. Surgery has evolved, giving patients many options. Each has its own good points and downsides.
Robotic surgery is getting more attention for its precision and quick recovery times. But, how does it stack up against traditional methods like laparoscopic and open surgery?
Outcome Comparisons with Laparoscopic Procedures
Research shows robotic surgery has some big advantages over laparoscopic procedures. It offers better vision and control, which can mean less blood loss and shorter hospital stays for some surgeries.
“Robotic surgery has been shown to reduce the risk of complications and improve patient outcomes in various surgical specialties.”
A study on gynecological surgeries found robotic surgery had less blood loss and fewer complications than laparoscopic surgery.
| Surgical Approach | Blood Loss (ml) | Complication Rate (%) |
| Robotic Surgery | 100 | 5 |
| Laparoscopic Surgery | 200 | 10 |
Cost-Effectiveness Analysis Across Different Specialties
The cost-effectiveness of robotic surgery changes with each specialty. Robotic systems are pricier than traditional laparoscopic tools. Yet, their benefits can save healthcare costs in the long run.
In urology, robotic-assisted surgeries cut down hospital stays. This can make up for the higher upfront cost of robotic surgery.
But a detailed cost-effectiveness study is needed to grasp the economic impact of robotic surgery in different fields.
Negative Impact on Surgical Team Dynamics
Robotic systems have changed how surgeries are done. They affect the team in the operating room. It’s important to know how they change the team’s work.
Communication Challenges in the Robotic Operating Room
Robotic surgery makes talking harder for the team. The setup can block clear communication. For example, the surgeon at the console can’t talk as easily as in open surgery.
Without clear signals, team members might misunderstand or wait too long. This is a big problem during the critical moments.
Physical Separation of Surgeon from Patient and Team
The surgeon is far from the patient and team in robotic surgery. This makes it hard for them to work well together. It can make the surgeon feel disconnected from the team.
Let’s look at how robotic surgery affects teamwork:
| Challenge | Description | Impact on Team Dynamics |
| Communication Barriers | Physical setup hinders direct communication | Potential for misunderstandings and delays |
| Physical Separation | Surgeon isolated from patient and team | Sense of disconnection among team members |
| Training Requirements | Need for specialized training for robotic surgery | Increased complexity in team coordination |
Knowing these challenges helps us improve teamwork in robotic surgeries.
Regulatory and Oversight Challenges
Ensuring patient safety in robotic surgery is a big task. It needs strong rules and checks. We look at the hurdles in making and enforcing these rules, focusing on FDA approval and reporting of bad events.
FDA Approval Process Limitations for Surgical Robots
The FDA is key in approving new robotic surgery tools. But the process has its limits. The pre-market approval process might not show the full safety and effectiveness of these tools. Also, the FDA’s use of 510(k) clearance can mean less strict testing for new robots.
The table below shows some important parts of the FDA approval process for robotic surgery tools.
| Approval Process | Description | Limitations |
| Pre-market Approval | Rigorous review of safety and efficacy | May not capture long-term effects |
| 510(k) Clearance | Approval based on substantial equivalence | Limited clinical testing for new devices |
Adverse Event Reporting and Monitoring Deficiencies
Good reporting of bad events is key to keeping robotic surgery safe. But the current system has its flaws. Not all bad events are reported, mainly because of a lack of standard rules and different reporting ways among doctors. Also, the complex nature of these systems makes it hard to find the cause of problems.
To make things better, we need to work on reporting and watching these events more closely. This can be done by:
- Standardizing reporting practices
- Implementing robust monitoring systems
- Encouraging transparency among healthcare providers
By tackling the regulatory and oversight challenges in robotic surgery, we can make sure these new technologies are used safely. This will help improve patient results.
Marketing Claims vs. Clinical Reality
Robotic surgery is becoming more common, but the gap between what’s promised and what happens is big. Companies making these systems say they offer better precision, less blood loss, and faster recovery. But we need to check if these claims are true.
Critical Analysis of Manufacturer Marketing Strategies
Ads for robotic surgery systems talk up their tech and benefits over old-school surgery. For example, Intuitive Surgical’s da Vinci system is hailed as a game-changer for precision. But we should look closely at the proof behind these claims. It turns out, while robotic surgery has some pluses, the hype might be too high.
Marketing often picks and chooses data to show only the good sides. For example, a study might show robotic surgery cuts down on complications. But it might not talk about longer surgery times or the learning curve for surgeons.
Evidence-Based Assessment of Claimed Benefits
We need to look at real data and studies on robotic surgery. A deep dive into the research shows mixed results. Some studies back up claims of less blood loss and shorter stays. But others find no big difference in how patients do.
| Claimed Benefit | Evidence-Based Outcome | Clinical Significance |
| Improved Precision | Mixed results; some studies show improvement, while others show no significant difference. | Limited clinical significance due to variability in surgeon skill and technique. |
| Less Blood Loss | Generally supported by evidence, robotic surgery often results in less blood loss compared to open surgery. | Clinically significant, particularly for surgeries with a high risk of bleeding. |
| Quicker Recovery | Evidence is mixed; some studies show quicker recovery, while others find no significant difference. | Clinically significant for patients with quicker recovery, but not universally applicable. |
In short, robotic surgery has some good points, but we must be careful with marketing claims. A closer look shows the real benefits are more complex and varied than ads say. As robotic surgery grows, it’s key for doctors and patients to know both the good and the bad.
Patient Selection Problems and Contraindications
The success of robotic surgery depends a lot on picking the right patients. This is a complex task. It’s key to choose wisely to avoid risks and get the best results.
Inappropriate Patient Selection Risks
Choosing the wrong patients for robotic surgery can lead to more problems. Things like obesity or past surgeries can make it harder. For example, obesity can make it tough to set up and use the robotic systems. This can lead to longer surgeries and more mechanical issues.
Key risks include:
- More chance of mechanical failures because of complex body shapes
- Greater chance of needing to switch to open surgery
- More blood loss and longer recovery times
Medical Conditions That Increase Complications with Robotic Approaches
Some health issues make robotic surgery riskier. These include severe adhesions, heart and lung problems, and issues that make long surgeries hard. It’s important to check these carefully before deciding on robotic surgery.
For instance, people with serious heart and lung issues might face more risks. This is because the gas used in laparoscopic procedures can cause breathing problems.
To lower these risks, a detailed check-up before surgery is vital. This includes looking at the patient’s health, past surgeries, and any conditions that might make surgery harder. By picking the right patients, doctors can reduce risks and improve outcomes.
Ethical Concerns in the Adoption of Robotic Surgery
The use of robotic surgery in medicine raises big ethical questions. As we use more robotic systems, we must think about how they affect patient care and safety.
Informed Consent Challenges and Patient Expectations
Ensuring patients know the risks and benefits of robotic surgery is key. Informed consent is vital, but robotic surgery’s complexity makes it hard. We need to make sure patients understand the procedure, its risks, and its benefits compared to traditional surgery.
Managing what patients expect from robotic surgery is also important. We must help patients have realistic hopes about what robotic surgery can do.
Balancing Technological Innovation with Patient Safety
Another big issue is balancing new robotic tech with keeping patients safe. As tech advances, we might forget about safety and how well it works.
To fix this, we need to test and check new robotic systems carefully. We should look at their tech and how it affects patients’ health.
| Ethical Consideration | Description | Action Required |
| Informed Consent | Ensuring patients understand the risks and benefits of robotic surgery | Clear, detailed consent forms and patient education |
| Patient Expectations | Managing patient expectations regarding outcomes | Realistic counseling and outcome reporting |
| Technological Innovation vs. Patient Safety | Balancing advancements with safety concerns | Rigorous testing and evaluation of new systems |
By tackling these ethical issues early, we can make sure robotic surgery improves care and keeps safety and ethics top priorities.
Emerging and Future Challenges for Robotic Surgical Technology
Robotic surgery is getting better, but new problems are coming up. The field is growing fast, with lots of money going into research. But we need to fix some tech issues and research gaps to make robotic surgery better.
Technological Limitations Requiring Solutions
One big problem is the lack of haptic feedback. This makes it hard for surgeons to know how much force they’re using. Improving haptic feedback technology is key to making robotic surgery more precise and safe. Also, the high cost of these systems and the need for standardized training protocols are big hurdles.
Another issue is the complexity of these systems. This can cause technical problems during surgery. It’s vital to make these systems reliable and safe. Companies must focus on robust design and testing to reduce the chance of mechanical failures.
Research Gaps and Development Needs
There are many research areas that need work to improve robotic surgery. One important area is developing better artificial intelligence (AI) algorithms to help surgeons. AI could make decisions faster and improve patient care.
We also need more studies to compare robotic surgery with traditional methods. Comparative effectiveness research will show when robotic surgery is best used.
In summary, robotic surgical technology is promising, but we must tackle the challenges and tech issues. By focusing on research and development, we can make robotic surgery even better.
Conclusion: Weighing the Disadvantages of Robotic Surgery Against Its Benefits
Robotic surgery is a big part of modern medicine, but it has its downsides. We’ve looked at the high costs, technical issues, and possible complications. We also talked about the learning curve for surgeons and picking the right patients.
Robotic surgery is a complex area that needs careful thought about its good and bad sides. It could change healthcare a lot, but we must keep patients safe and happy. Knowing the limits and risks of robotic surgery helps doctors and patients make better choices.
The future of robotic surgery depends on solving current problems and improving it. We need to focus on making it better for patients. Looking at robotic surgery in a balanced way is key. It shows its promise and its current challenges.
FAQ
What are the main disadvantages of robotic surgery?
Robotic surgery has several downsides. It’s expensive, has technical limits, and is hard for surgeons to learn. It also takes longer to operate and can have mechanical issues.
How does the cost of robotic surgery compare to traditional surgical methods?
Robotic surgery costs more than traditional methods. This is because of the high price of robotic systems, training, and certification.
What are the technical limitations of robotic surgery?
Robotic surgery lacks haptic feedback and has limited motion. It also risks system failures during surgery.
How does robotic surgery affect surgical team dynamics?
Robotic surgery can change how teams work together. It can cause communication problems and separate the surgeon from the team and patient.
What are the challenges associated with training surgeons in robotic surgery?
Training surgeons in robotic surgery is tough. It requires special training and can be hard for experienced surgeons to adapt.
How does robotic surgery impact patient outcomes compared to traditional surgery?
Robotic surgery might offer benefits like less blood loss and shorter stays. But its effects vary by procedure and specialty.
What are the accessibility issues related to robotic surgery?
Access to robotic surgery is a problem. It’s mainly available in cities, and cost can be a barrier for some.
How do regulatory challenges affect the adoption of robotic surgery?
Rules and reporting issues can slow down robotic surgery adoption. This includes FDA approval and tracking adverse events.
What are the ethical concerns associated with robotic surgery?
Ethical issues include getting consent, managing patient hopes, and balancing tech with safety.
What are the future challenges facing robotic surgical technology?
Future challenges include improving tech, like haptic feedback, and making surgery safer and more effective.
Is robotic surgery suitable for all patients?
No, robotic surgery isn’t right for everyone. Certain conditions, like obesity, can raise risks. Choosing the right patient is key.
How do marketing claims for robotic surgery compare to clinical reality?
Marketing often highlights robotic surgery’s benefits. But it’s important to check the evidence to see if these claims are true.
References
- Smith, R. A., & Haigh, J. (2018). Technical challenges and complications of robotic surgery. Minimally Invasive Surgery, 2018, 8403163. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5949296