Last Updated on December 1, 2025 by Bilal Hasdemir
Stereotactic Body Radiation Therapy (SBRT) has changed cancer treatment. It offers high precision and is very effective in targeting tumors.
Recent studies show SBRT works well for many cancers, like lung and prostate cancer. It has impressive cure rates and minimal side effects. As SBRT keeps getting better, a big question is: how many times can a patient get stereotactic radiation?
It’s important for patients and doctors to know the limits and possibilities of stereotactic radiation. This knowledge helps in making smart choices about cancer treatment.
Key Takeaways
- SBRT is a highly effective treatment for various cancers.
- The number of times SBRT can be administered depends on several factors.
- Understanding the limitations of stereotactic radiation is key for treatment planning.
- SBRT offers minimal side effects compared to traditional radiation therapy.
- Advances in SBRT continue to improve cancer treatment outcomes.
Understanding Stereotactic Radiation Therapy
Stereotactic radiation therapy has changed how we treat cancer. It uses precise, high doses of radiation to target tumors. This makes it a key part of cancer treatment.
Definition and Basic Principles
Stereotactic radiation therapy, or SRT, uses advanced tech to hit tumors from many angles. This method gives high doses to the tumor while protecting healthy tissues.
The main ideas behind SRT are:
- Using advanced imaging to find the tumor’s exact spot
- Shooting radiation from many sides to focus on the tumor
- Using special software to plan the best radiation pattern
Historical Development of Stereotactic Techniques
The idea of SRT started in the early 1900s with neurosurgery frames. Later, CT and MRI scans helped target tumors better. The use of linear accelerators and robotic systems made SRT even more precise.
Key Components of Stereotactic Radiation Systems
Today’s SRT systems have important parts:
- Advanced imaging for finding tumors
- Smart software for planning treatment
- Accurate systems like linear accelerators or robots for delivering radiation
These parts work together to deliver radiation precisely. This makes SRT a strong tool against cancer.
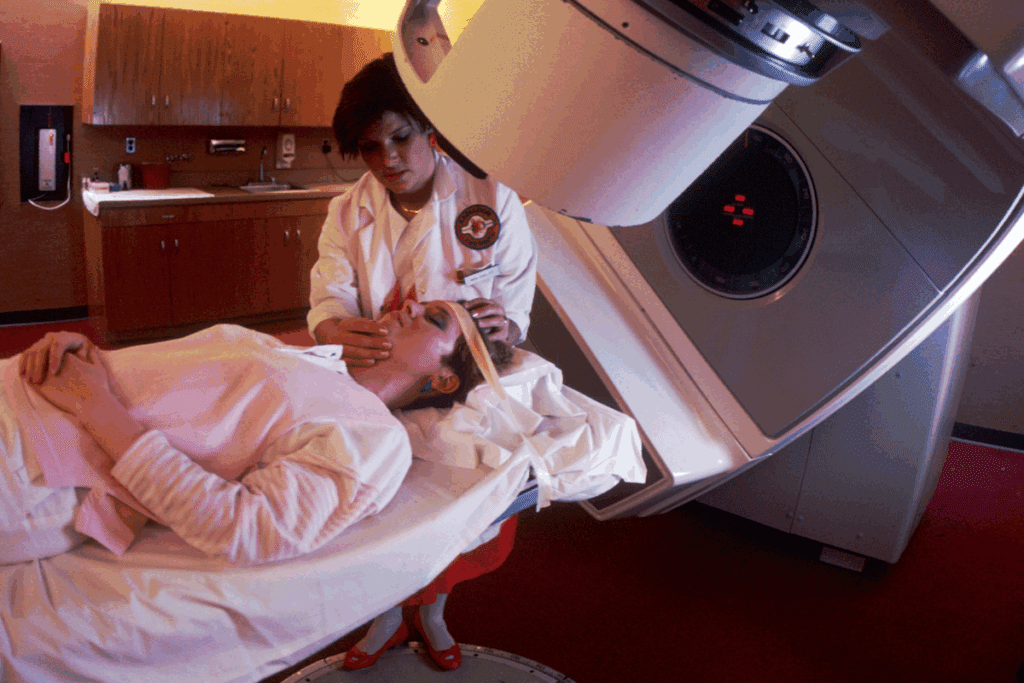
Types of Stereotactic Radiation Treatments
Stereotactic radiation therapy includes many treatments for different health issues. These methods have changed how we treat cancer and other diseases. They offer precise and effective solutions.
Stereotactic Radiosurgery (SRS)
Stereotactic Radiosurgery (SRS) is a precise radiation therapy for brain tumors and abnormalities. It’s not surgery but a non-invasive treatment. This method delivers a high dose of radiation to the target area while protecting healthy tissues. It’s used for conditions like acoustic neuromas and brain metastases.
Stereotactic Body Radiation Therapy (SBRT)
Stereotactic Body Radiation Therapy (SBRT) targets tumors outside the brain, like in the lung or liver. It gives high doses of radiation in a few sessions. SBRT is popular for treating tumors that can’t be removed surgically or are near important structures. It’s better than some other treatments because it delivers high doses in fewer sessions.
Stereotactic Radiotherapy (SRT)
Stereotactic Radiotherapy (SRT) combines SRS’s precision with conventional radiotherapy’s fractionation. It’s used for targets near critical structures or larger tumors. SRT can treat both brain and body targets. It’s a flexible option that may reduce side effects by fractionating the dose.
It’s important to know the differences between these treatments to choose the best one for each patient. Tumor size, location, and patient health are key factors. As radiation oncology advances, these treatments will likely remain key in cancer care, bringing hope and better outcomes to patients globally.
The Science Behind SBRT and Radiation Dose Limitations
Understanding SBRT is key to seeing its value in cancer treatment. SBRT is a precise way to give high doses of radiation to tumors. It does this while protecting the healthy tissues around the tumor.
Radiation Fractionation Principles
Radiation fractionation is a core idea in SBRT. It breaks down the total dose into smaller parts. This lets us give high doses to tumors while normal tissues recover between doses. It helps control tumors better while keeping normal tissues safe.
Biological Effective Dose (BED)
The Biological Effective Dose (BED) is vital in SBRT. It considers the dose per fraction, total dose, and how sensitive the tumor and normal tissues are. It helps doctors plan treatments that work best for each patient.
Normal Tissue Tolerance
Normal tissue tolerance is key in planning SBRT treatments. Different tissues can handle different amounts of radiation. Knowing this helps avoid harming healthy tissues. Advanced tools help doctors plan treatments that protect these tissues.
Concept | Description | Importance in SBRT |
Radiation Fractionation | Dividing the total radiation dose into smaller fractions | Maximizes therapeutic ratio, enhances tumor control while minimizing normal tissue damage |
Biological Effective Dose (BED) | A measure that predicts the biological effect of a radiation dose | Helps in optimizing treatment plans by considering dose per fraction and total dose |
Normal Tissue Tolerance | The ability of normal tissues to withstand radiation without significant damage | Crucial for avoiding toxicity and designing safe treatment plans |
By using the science of radiation fractionation, BED, and normal tissue tolerance, doctors can make SBRT treatments better. This helps patients get the best results. As we keep improving in radiation oncology, these principles will be even more important for safe and effective cancer treatments.
Factors Determining Retreatment Possibilities
When thinking about Stereotactic Body Radiation Therapy (SBRT) retreatment, many important factors come into play. Deciding on retreatment is complex. It involves looking at several elements to get the best results for the patient.
Time Interval Between Treatments
The time between the first treatment and any possible retreatment is key. Research shows that the gap between treatments affects how well and safely retreatment works. A few months’ wait is often advised to let normal tissues heal and to check if more treatment is needed.
Cumulative Radiation Dose Considerations
The total radiation dose to the tumor and nearby tissues is also very important. It’s vital to calculate this dose carefully. This ensures the tumor is treated well without harming the surrounding tissues too much. Advanced dosimetry techniques help keep the dose safe.
Factor | Description | Consideration |
Time Interval | Time between initial treatment and retreatment | Allows for recovery of normal tissues |
Cumulative Dose | Total radiation dose delivered | Must be within safe limits to avoid toxicity |
Patient Factors | Individual patient health and condition | Influences tolerance to retreatment |
Individual Patient Factors
Each patient’s health, how well they can perform daily tasks, and how they’ve reacted to previous treatments are all important. These factors can affect how well a patient can handle retreatment and the chances of success. It’s important to evaluate these carefully before making a decision.
Healthcare providers carefully weigh these factors to decide if SBRT retreatment is right for each patient. Our team makes sure to consider all important factors to give the best care possible.
Retreatment Guidelines for Different Body Sites
Deciding to retreat with SBRT requires understanding the unique challenges of different body parts. It’s important to follow specific guidelines to ensure safety and effectiveness.
Brain Retreatment Protocols
Brain retreatment is complex due to the risk of radiation necrosis and neurological issues. Key factors include the initial dose, time elapsed, and target lesion volume. We also check the cumulative dose to critical areas like the brainstem and optic pathways.
- Evaluate initial radiation dose and target volume
- Assess time elapsed from first treatment
- Consider cumulative dose to critical structures
Lung Reirradiation Considerations
Lung reirradiation is challenging due to the risk of pneumonitis and limited lung tolerance. Factors include the initial dose, treatment interval, and lung disease presence. We look at dose to critical areas and use techniques to protect normal lung tissue.
- Assess initial radiation dose and lung function
- Evaluate interval between treatments and disease progression
- Minimize dose to normal lung tissue
Liver, Spine, and Other Sites
Liver and spine reirradiation consider the organ’s function and proximity to critical areas. The liver’s regenerative ability and spine’s radiation tolerance are key. Advanced imaging and dose calculation are vital for safe retreatment. We also tailor our approach to other sites like adrenal glands and lymph nodes, based on their anatomy and radiation sensitivity.
SBRT Applications in Cancer Treatment
SBRT in cancer treatment is showing great promise, mainly for lung, prostate, and liver tumors. It’s a non-invasive option with high success rates and few side effects. This makes it a key tool in the fight against cancer.
Lung Cancer SBRT
SBRT is now a top choice for early-stage lung cancer. It’s great for those who can’t have surgery because of health issues. High local control rates have been seen, with some studies showing over 90% success.
“SBRT is a highly effective treatment for lung cancer,” says Dr. [Last Name], a leading radiation oncologist. “It can cure the disease or greatly improve life quality.”
Prostate Cancer SBRT
SBRT is popular for prostate cancer because it’s a hypofractionated treatment. This means fewer sessions than traditional radiation. It’s more convenient and lowers side effect risks. Studies show SBRT for prostate cancer has high success rates, similar to other treatments.
- High biochemical control rates
- Reduced treatment duration
- Minimal side effects
Liver and Other Abdominal Malignancies
SBRT is also used for liver tumors and other abdominal cancers. Its precision allows for high doses to tumors while protecting healthy tissues. This is a big plus for patients with tumors near important areas.
Comparing SBRT to Other Radiation Modalities
Radiation oncology is always evolving. It’s key to compare SBRT with conventional radiotherapy, IMRT, and proton therapy to find the best treatment. SBRT stands out because it can give high doses of radiation right to the tumor. This helps avoid harming healthy tissues nearby.
SBRT vs. Conventional Radiotherapy
Conventional radiotherapy uses smaller doses over a longer time. SBRT, on the other hand, gives higher doses in fewer sessions. This change can greatly affect how well the treatment works and how easy it is for the patient. Research shows SBRT can be very effective for some tumors, making it a strong option for certain cases.
But, conventional radiotherapy is good for bigger or more spread-out tumors. Whether to choose SBRT or conventional radiotherapy depends on the tumor’s size, where it is, and the patient’s health.
SBRT vs. IMRT
Intensity-Modulated Radiation Therapy (IMRT) is another precise radiation therapy. It’s similar to SBRT in precision but differs in dose and how it’s given. IMRT is often used for tumors near important areas or that are not perfectly shaped.
SBRT is better for smaller, more focused tumors because it uses higher doses. The choice between SBRT and IMRT depends on the specific situation and what the treatment aims to achieve.
SBRT vs. Proton Therapy
Proton therapy uses protons to kill cancer cells, unlike photons in other therapies. It has a sharp drop-off in dose beyond the target, which can protect important areas. When comparing SBRT to proton therapy, we look at the type of radiation and how it works on cells.
Proton therapy might be better for some, like kids or tumors near vital areas. But SBRT is also very effective for many patients. Choosing between them depends on the tumor and the patient’s situation.
In summary, comparing SBRT with other treatments shows how important tailored treatment plans are in radiation oncology. Knowing the strengths and weaknesses of each helps doctors make the best choices for their patients.
Side Effects of Repeated Stereotactic Radiation
It’s important to know about the side effects of repeated stereotactic radiation. This is key for those thinking about this treatment. As we keep improving cancer treatments, we must talk about how repeated radiation affects the body.
Acute Side Effects
Acute side effects happen right after or during treatment. They can change based on where the treatment is given. Common ones include feeling tired, skin issues, and pain in the treated area. It’s vital for patients to tell their doctors about these symptoms to get help.
For example, lung treatments might cause coughing or trouble breathing. Liver treatments could lead to nausea or stomach pain. Keeping an eye on these side effects helps doctors act fast.
Treatment Area | Common Acute Side Effects |
Lung | Cough, shortness of breath |
Liver | Nausea, abdominal discomfort |
Prostate | Urinary frequency, discomfort |
Late and Cumulative Toxicities
Late toxicities can show up months or years after treatment. They happen because of the long-term effect of radiation on healthy tissues. These can include scarring, damage to important parts, and rare cases of new cancers.
Cumulative toxicities are a big worry with repeated treatments. The risk goes up with each treatment. Using advanced imaging and planning is key to lowering these risks.
Managing Side Effects from Multiple Treatments
Handling side effects well needs a team effort. This team includes radiation and medical oncologists, and specialists in supportive care. They adjust treatment plans, use medicines to ease symptoms, and help improve life quality.
When SBRT is done again in the same spot, careful planning is needed. This helps avoid too much radiation and lowers toxicity risk. Teaching patients and following up are also key in managing side effects.
By knowing about the side effects of repeated radiation and how to manage them, we can make patients’ lives better. It’s a detailed process, but it’s vital for giving our patients the best care.
The Treatment Planning Process for Reirradiation
Reirradiation planning is a complex process. It uses the latest technology and clinical knowledge. Stereoctactic body radiation therapy (SBRT) planning is extra tricky because it needs precise targeting and dose delivery.
Advanced Imaging Requirements
Advanced imaging is key in reirradiation planning. We use high-resolution MRI and CT scans to clearly see the target area and important structures. This helps us give high doses to the tumor while protecting normal tissues.
Dose Calculation Challenges
Calculating doses for reirradiation is hard. We must consider the effects of previous radiation and the risk of harm. Our advanced algorithms account for this history, keeping doses safe for critical areas.
Treatment Delivery Considerations
Delivering treatment for reirradiation needs careful planning. We use image-guided radiation therapy (IGRT) and respiratory gating to ensure the dose is delivered accurately. This precision is vital to reduce side effects and improve treatment results.
By combining advanced imaging, precise dose calculation, and careful treatment delivery, we can plan and execute reirradiation treatments. These treatments meet the complex needs of our patients.
Clinical Decision-Making for Repeat SBRT
Deciding on repeat Stereotactic Body Radiation Therapy (SBRT) requires a deep understanding of its benefits and risks. A thorough evaluation is key to ensure the benefits outweigh the risks for each patient.
Multidisciplinary Tumor Board Approach
A multidisciplinary tumor board is vital for deciding on repeat SBRT. It brings together experts from radiation oncology, medical oncology, surgical oncology, and radiology. This team makes informed decisions based on a patient’s condition and treatment history.
Key benefits of this approach include better treatment outcomes, safer care, and more tailored treatment plans. The tumor board reviews each case, using the latest information and treatment options.
Risk-Benefit Analysis
Doing a detailed risk-benefit analysis is key in deciding on repeat SBRT. We look at the benefits of more SBRT against the risks and side effects. We consider the patient’s health, tumor location and size, previous treatments, and success chances.
We compare the benefits, like better local control and survival, to the risks, like more toxicity and side effects. This careful analysis helps decide if repeat SBRT is right for each patient.
Patient Selection Criteria
Setting clear criteria is essential for choosing the right patients for repeat SBRT. These criteria include how long ago the last SBRT was, the total radiation dose, and the patient’s health.
Key considerations include oligometastatic disease, the chance for local control, and the patient’s health status. By carefully looking at these factors, we find the best candidates for repeat SBRT, reducing risks.
Real-World Case Studies of Multiple SBRT Treatments
SBRT is versatile in treating different clinical scenarios. This includes oligometastatic disease and local recurrence. Real-world case studies offer insights into SBRT’s practical application and outcomes.
Oligometastatic Disease Management
Oligometastatic disease means patients have a few metastatic lesions. SBRT is a promising treatment for these patients. It aims to improve survival and control the disease.
Several cases show SBRT’s effectiveness in managing oligometastatic disease. For example, a patient with lung cancer had three lesions. SBRT treated them, leading to complete or partial response in all.
Patient Profile | Number of Lesions | SBRT Outcome |
65-year-old male with lung cancer | 3 | Complete response in 2 lesions, partial response in 1 |
50-year-old female with breast cancer | 2 | Complete response in both lesions |
Local Recurrence Scenarios
Local recurrence after initial radiation therapy is a big challenge. SBRT is a viable retreatment option. It aims for local control with minimal side effects.
A notable case was a patient with locally recurrent prostate cancer. He was first treated with conventional radiation. SBRT was used as a second treatment, achieving biochemical control without major side effects.
These case studies highlight SBRT’s role in complex clinical scenarios. By examining real-world outcomes, we gain a better understanding of SBRT’s benefits and limitations.
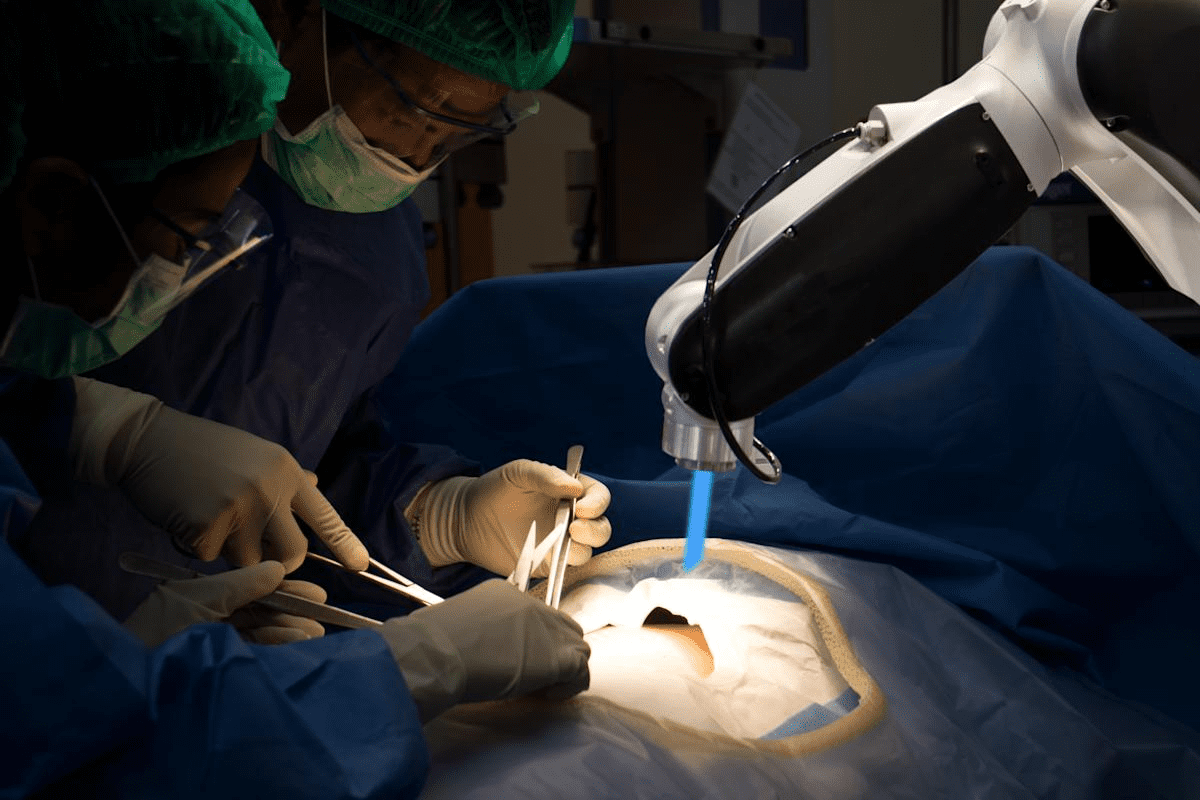
Technological Advances Enabling Safer Retreatment
The field of SBRT is changing fast, thanks to new technology. These changes are making treatments safer and more effective for patients.
Advancements in MRI-Guided Radiation Therapy
MRI-guided radiation therapy is a big step up in SBRT. It combines MRI scans with radiation therapy for precise tumor targeting. This means we can give more radiation to the tumor while protecting healthy tissues.
MRI-guided SBRT brings many benefits. It improves accuracy and lets us adjust treatment plans as needed. This is key for tumors near important areas or those that move, like in the lungs or belly.
Adaptive Planning Techniques
Adaptive planning is another key improvement in SBRT. It lets us change the treatment plan during therapy if the tumor or patient changes. This keeps the treatment safe and effective.
Adaptive planning uses advanced imaging and software to adjust treatment plans. This makes radiation delivery more precise, reducing side effects and improving results.
Improvements in Motion Management
Motion management is vital for SBRT, mainly for tumors that move. New tech has greatly improved how we manage this. Techniques like respiratory gating and real-time tracking help us hit moving tumors accurately.
These motion management upgrades have made SBRT retreatments safer and more effective. They help us target tumors better and reduce side effects, giving patients better treatment options.
In summary, MRI-guided radiation therapy, adaptive planning, and motion management tech are changing SBRT. These advancements are making retreatments safer and more effective, giving patients new hope for their treatment.
Cost and Insurance Considerations for Multiple SBRT Courses
It’s important to know the costs of repeated SBRT courses. This helps in making smart choices. We need to talk about the money side and insurance rules that affect both patients and doctors.
Insurance Coverage Policies
Insurance for SBRT changes from one provider to another. Make sure to check your coverage before starting treatment. Many plans cover SBRT for certain reasons, but how much they cover can vary.
- Find out if your insurance covers SBRT for your condition.
- Know the costs you’ll face, like deductibles and co-pays.
- Look at any limits or exclusions that might affect your coverage.
We suggest talking to your doctor and insurance about your treatment’s costs. This way, you’ll understand what you’ll have to pay for your treatment plan.
Cost-Effectiveness of Retreatment
When thinking about SBRT retreatment costs, consider a few things. These include the treatment price, any side effects, and how it affects your life. New technologies and methods can change these, possibly making things better and cheaper.
- The first cost of SBRT treatment.
- The price of dealing with side effects and problems.
- The chance for better results and a better life.
Research shows SBRT can be a good deal in some cases, compared to other treatments. But, whether it’s worth it for a second time depends on each person’s situation and treatment details.
Knowing about the costs and insurance for multiple SBRT treatments helps patients and doctors make better choices. They can weigh the benefits against the costs.
Conclusion: The Future of Multiple Course Stereotactic Radiation
The future of Stereotactic Body Radiation Therapy (SBRT) is looking bright. New research and tech are making treatments safer and more effective. This is great news for those needing multiple treatments.
SBRT has made big strides, helping treat many cancers safely. New tech is making it even better. MRI-guided therapy and adaptive planning are key to these improvements.
SBRT’s future is all about tailoring treatments to each patient. This means using the latest in imaging and dose planning to reduce side effects. It’s a big step towards better cancer care.
As SBRT advances, we’ll see better results for patients. It will play a bigger role in treating complex cases. The future of SBRT is full of promise, thanks to ongoing research and tech.
FAQ
What is stereotactic radiation therapy?
Stereotactic radiation therapy uses precise, high doses of radiation. It targets tumors or lesions, often in a single fraction or a few fractions.
How many times can you have stereotactic body radiation therapy (SBRT)?
The number of SBRT sessions varies. It depends on the tumor’s location, size, and the dose from previous treatments. We consider each case individually to find the best treatment.
What is the difference between SRS, SBRT, and SRT?
SRS is for brain lesions, delivering a single high dose. SBRT treats extracranial tumors with a few fractions. SRT includes both SRS and SBRT, plus fractionated treatments.
Can you have SBRT more than once for the same tumor?
Retreatment with SBRT is possible in some cases. It depends on the initial dose, time elapsed, and tumor details. We assess risks and benefits for each patient.
What are the side effects of repeated stereotactic radiation?
Side effects vary by location and dose. Common ones include fatigue, skin reactions, and nausea. Late effects might include fibrosis or secondary cancers. We aim to minimize these risks through careful planning.
How is SBRT different from conventional radiation therapy?
SBRT uses higher doses in fewer fractions than conventional therapy. This precision and higher dose rate can lead to better tumor control and fewer side effects.
What is the role of a multidisciplinary tumor board in deciding on repeat SBRT?
A tumor board reviews complex cases. It includes radiation oncologists, medical oncologists, and surgeons. This team decides if repeat SBRT is best, ensuring a thorough approach.
Are there any new technologies that enable safer retreatment with SBRT?
Yes, new technologies like MRI-guided radiation therapy and adaptive planning have improved SBRT safety and effectiveness. These advancements make retreatment more feasible in some cases.
How does insurance coverage work for multiple SBRT courses?
Insurance for multiple SBRT courses varies. We help patients understand their coverage and explore cost management options for retreatment.
What is the cost-effectiveness of retreatment with SBRT?
The cost-effectiveness of SBRT retreatment depends on several factors. These include the patient’s health, tumor characteristics, and retreatment benefits. We evaluate each case to find the most cost-effective approach.
References
National Center for Biotechnology Information. Stereotactic Body Radiation Therapy Retreatment Efficacy and Frequency. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5754194/