Last Updated on December 1, 2025 by Bilal Hasdemir
Radiation therapy and stereotactic radiosurgery are two ways to fight cancer. They use high-energy beams to hit tumors. But they work in different ways.
Radiation therapy is a wide term for many methods to kill cancer cells with radiation. It can be given from outside or inside the body, based on the cancer type and stage.
Stereotactic radiosurgery, or SRS, is a precise radiation therapy. It gives a strong dose of radiation to one spot, trying to harm less of the healthy tissue around it.
Key Takeaways
- Radiation therapy and stereotactic radiosurgery are both cancer treatments that use radiation.
- The key difference lies in their approach and application.
- Radiation therapy is a broader term that encompasses various techniques.
- Stereotactic radiosurgery is a precise form of radiation therapy.
- Both treatments are effective in destroying cancer cells.
Understanding Radiation Therapy Fundamentals
Radiation therapy is a key part of cancer treatment. It uses high-energy particles to kill cancer cells. Machines beam intense energy to target and destroy cancer cells, as Medical Expert.
Definition and Basic Principles of Radiation Therapy
Radiation therapy, or radiotherapy, is a treatment that uses high-energy rays. It aims to kill cancer cells or slow their growth. The goal is to deliver a precise dose of radiation to a specific area, protecting healthy tissues.
Key aspects of radiation therapy include:
- Precision in targeting tumors
- Effective dose delivery
- Minimizing side effects
Common Abbreviations in Radiation Oncology (RT, XRT)
In radiation oncology, several abbreviations are used. RT means Radiation Therapy, and XRT is for External Beam Radiation Therapy. Knowing these terms helps patients and healthcare providers communicate better.
Abbreviation | Meaning |
RT | Radiation Therapy |
XRT | External Beam Radiation Therapy |
Historical Development of Radiation Treatment
The history of radiation therapy began in the late 19th century. It started after Wilhelm Conrad Röntgen discovered X-rays in 1895. Over time, treatments have evolved from simple X-rays to advanced technologies like IMRT and SBRT.
As we keep improving in radiation oncology, knowing the basics of radiation therapy is key. This knowledge helps us make better choices in cancer treatment.
Introduction to Stereotactic Radiosurgery (SRS)
SRS, or stereotactic radiosurgery, is a precise medical technique. It delivers high doses of radiation with great accuracy. This method has changed how we treat complex medical conditions, like tumors and some neurological disorders.
Defining Stereotactic Radiosurgery
Stereotactic radiosurgery is a non-invasive treatment. It uses many beams of radiation to focus on a small area of the body. This method allows for high doses of radiation to target the area while protecting healthy tissues nearby. It’s great for treating tumors and lesions that are hard to reach or near important structures.
The Origin and Evolution of SRS Technology
Lars Leksell introduced SRS in the 1950s for treating brain conditions. Over time, SRS technology has grown, using better imaging and radiation systems. CyberKnife technology, for example, uses a robot to track and deliver radiation to tumors, even when a patient breathes. This has made SRS a treatment option for more conditions.
Key Components of SRS Treatment
The success of SRS depends on several key parts. These include precise imaging, accurate patient positioning, and advanced radiation systems. Advanced imaging like MRI and CT scans help doctors target the area with precision. Immobilization devices and tracking systems also ensure the radiation hits the right spot, reducing risks.
As SRS technology improves, so do patient outcomes. Its precision and effectiveness make it a valuable treatment for many conditions. Plus, its non-invasive nature offers a gentler alternative to traditional surgery.
Core Differences Between Radiation Therapy and Radiosurgery
When looking at cancer treatment options, it’s key to know the difference between radiation therapy and radiosurgery. Both use radiation to fight cancer, but they work in different ways. They have different methods, uses, and results.
Precision and Targeting Capabilities
Radiation therapy is a wide term for using radiation to treat cancer. It can be given from outside or inside the body, based on the cancer type and stage. Radiosurgery, like Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiation Therapy (SBRT), is very precise. It sends high doses of radiation to exact spots, harming less of the surrounding tissue.
We use the latest tech to aim accurately, which helps lower side effects and better patient results. Radiosurgery is great for tumors near important areas or that can’t be removed.
Dose Delivery and Fractionation Approaches
The way radiation is given and split up is another big difference. Regular radiation therapy breaks the total dose into smaller parts given over time. This lets normal tissues heal between doses. Radiosurgery, though, gives a big dose all at once or in a few parts, thanks to its exact aim.
Choosing between regular radiation and radiosurgery depends on many things. These include the tumor’s type, size, and where it is, and the patient’s health. SBRT, for example, is a strong treatment for lung cancer because it targets radiation well.
Treatment Characteristics | Radiation Therapy | Radiosurgery |
Precision | Variable, depending on the technique | Highly precise |
Fractionation | Often fractionated | Single or few fractions |
Application | Broad applications in cancer treatment | Ideal for specific, localized tumors |
Treatment Intent and Outcomes
The goals of radiation therapy and radiosurgery are different. Regular radiation can aim to cure or ease symptoms. Radiosurgery is mostly for trying to cure tumors that are in one place or for easing symptoms in some cases. The results of these treatments vary, with radiosurgery often giving quick tumor control for the right patients.
We work with patients to find the best treatment plan for them. Knowing the main differences between radiation therapy and radiosurgery helps us tailor our treatment for the best results.
SBRT Radiation: A Revolutionary Approach
SBRT radiation has changed the game in cancer treatment. It’s a precise and effective way to fight cancer. This method sends high doses of radiation right to the tumor, while keeping healthy tissues safe.
What Makes SBRT Different from Conventional Radiation
SBRT is a new way to treat tumors compared to old methods. It doesn’t need weeks of treatment like traditional therapy. Thanks to advanced tech, it can finish in just a few sessions.
Key differences include:
- High dose per fraction
- Hypofractionation (fewer treatment sessions)
- Precise tumor targeting
- Minimized damage to surrounding tissues
The Technology Behind SBRT Delivery
SBRT’s success comes from its cutting-edge tech. Modern machines and imaging systems help deliver radiation with pinpoint accuracy. Tools like image-guided radiation therapy (IGRT) and respiratory gating make sure the tumor is hit right, even when it moves.
When SBRT is Recommended Over Other Options
SBRT is great for small, well-defined tumors that can’t be reached by surgery. It’s also good for those who’ve had radiation before and need it again.
Cancer Type | SBRT Suitability | Typical Fractions |
Lung Cancer | Highly suitable | 3-5 fractions |
Liver Cancer | Suitable | 3-5 fractions |
Prostate Cancer | Suitable | 5 fractions |
The new SBRT and SRS system at UPMC Hillman Cancer Center is a big step forward. It can target hard-to-reach tumors in just a few sessions, down from up to 45. This shows how much SBRT has improved radiation oncology.
Technical Aspects of Treatment Planning
The accuracy of radiation therapy and stereotactic radiosurgery depends on careful treatment planning. A team of healthcare experts works together to make a treatment plan for each patient.
Conventional Radiation Therapy Planning
Planning for conventional radiation therapy starts with simulation. The patient gets CT scans to find the tumor and nearby tissues. This info helps create a plan to target the tumor while protecting healthy tissues.
Key steps in conventional radiation therapy planning include:
- Patient immobilization to ensure consistent positioning
- Imaging and contouring of the tumor and organs at risk
- Beam arrangement and dose calculation
- Plan verification and quality assurance
Stereotactic Treatment Planning
Stereotactic treatment planning is more precise than conventional therapy. It uses advanced imaging like MRI and CT angiography to clearly see the tumor and nearby important structures.
The stereotactic treatment planning process includes:
- High-resolution imaging for precise tumor localization
- Advanced software for dose calculation and plan optimization
- Quality assurance measures to ensure accurate dose delivery
Image Guidance and Patient Positioning
Image-guided radiation therapy (IGRT) is key for both conventional and stereotactic treatments. IGRT uses imaging like X-ray, CT, or MRI to check the patient’s position and the tumor’s location before and during treatment.
Image Guidance Technique | Description | Application |
X-ray Imaging | Uses X-rays to visualize bony anatomy and implanted markers | Commonly used for prostate, lung, and other tumors |
CT Imaging | Provides detailed cross-sectional images of the patient’s anatomy | Used for complex cases requiring high precision |
MRI Imaging | Offers superior soft-tissue contrast for precise tumor delineation | Ideal for tumors in the brain, liver, and other soft-tissue areas |
Getting the patient’s position right and using image guidance is vital. It ensures the radiation dose hits the tumor accurately, reducing harm to healthy tissues.
Radiation Dose Considerations and Biological Effects
The impact of radiation dose changes a lot between regular and stereotactic treatments. It’s key to know how different doses affect patients.
Standard Radiation Therapy Dosing
Regular radiation therapy breaks the total dose into smaller parts given over weeks. This helps normal tissues repair while keeping tumors under control.
A common plan is daily doses of 1.8 to 2 Gy, up to 60 to 70 Gy for many tumors. The aim is to use the difference in repair between tumor and normal tissues to our advantage.
High-Dose Precision in Stereotactic Treatments
Stereotactic radiosurgery (SRS) and stereotactic body radiation therapy (SBRT) give high doses in a few or one fraction. This is thanks to advanced imaging and planning.
SBRT can give doses up to 20 Gy per fraction, with a total of 30 to 60 Gy over 3 to 5 fractions. The precision in SRS/SBRT needs exact patient positioning and immobilization to hit the target with minimal damage.
A leading oncologist says, “The treatment strategy is to boost the patient’s immune system.” This shows how vital it is to grasp the biological effects of different doses.
“The ability to deliver high doses of radiation precisely to the tumor, while sparing surrounding normal tissues, has revolutionized the treatment of various cancers.”
Characteristics | Conventional Radiation Therapy | Stereotactic Radiosurgery/SBRT |
Dose Fractionation | 1.8-2 Gy per fraction, 30-40 fractions | High dose per fraction (up to 20 Gy), 1-5 fractions |
Treatment Duration | Several weeks | Single fraction or a few days |
Treatment Precision | Less conformal, larger margins | Highly conformal, minimal margins |
Understanding the Radiobiology Differences
The effects of conventional versus SRS/SBRT radiation therapy are different. Knowing these differences is key to better treatment results.
High-dose therapy can cause unique effects like vascular damage and immune changes. These effects are less seen in regular fractionated therapy.
Treatment Duration and Patient Experience
The time it takes for radiation treatment is key to the patient’s experience. We’ll look at how long treatments last for conventional therapy and SRS/SBRT. Knowing this helps us see how treatments affect patients.
Conventional Radiation Therapy Timeframes
Conventional radiation therapy takes a long time. Treatments are split over weeks, with therapy given 5 days a week for 5 to 7 weeks. This long schedule can be hard for patients, affecting their life quality.
The long time needed for conventional therapy is because it aims to kill the tumor without harming healthy tissues. But, it can cause fatigue and other side effects, making daily life harder.
Accelerated Schedules with SRS and SBRT
SRS and SBRT are much quicker. SBRT treatments usually last just three to four sessions over one to two weeks. This is because SRS and SBRT are very precise, allowing for effective treatment in fewer sessions.
- Reduced treatment time
- Less disruption to daily life
- Potential for fewer side effects due to the precise targeting of tumors
The quick schedule of SRS and SBRT makes it a better choice for many. It’s great for those with certain tumors or who need to recover fast.
How Long Does It Take for SBRT to Work?
SBRT’s success depends on many things, like the cancer type and stage. Some see rapid tumor shrinkage after SBRT, while others may take months.
It’s important to know that SBRT is very effective. But, results can vary based on the tumor and the patient’s health. Regular follow-up appointments with doctors are key to tracking how well the treatment is working.
Understanding the differences in treatment time and patient experience helps both patients and doctors. This knowledge aids in choosing the best treatment option.
Applications of SBRT in Cancer Treatment
SBRT is a game-changer in cancer treatment. It’s a special kind of external therapy that gives focused doses of radiation. This offers hope to those with tough-to-treat tumors.
SBRT is changing oncology. It’s precise and can give high doses of radiation. This makes it great for treating many cancers, from early stages to advanced cases.
SBRT for Lung Cancer Treatment
SBRT is a big hope for lung cancer patients. It targets tumors well while keeping healthy tissue safe. This makes it a good choice for lung cancer treatment.
Studies show SBRT for lung cancer works well. It has high success rates and low side effects. A top oncologist says,
“SBRT is a big step forward in lung cancer treatment. It’s a non-invasive and effective option.”
SBRT for Liver and Pancreatic Tumors
SBRT is also used for liver and pancreatic tumors. Its precision lets it give high doses right to the tumor. This reduces harm to nearby organs.
For liver cancer, SBRT can improve survival and reduce symptoms. In pancreatic cancer, it helps control tumors and ease pain.
SBRT for Spinal and Bone Metastases
SBRT is used for spinal and bone metastases too. It delivers precise radiation to these areas. This helps with pain and prevents fractures.
SBRT targets metastatic disease, improving life quality for advanced cancer patients. As cancer treatment evolves, SBRT will be key in managing complex cases.
SRS Applications in Neurological Conditions
SRS is a big step forward in treating complex neurological issues. It offers a precise way to help patients. We use SRS for many neurological problems, thanks to its accuracy and success.
Brain Tumors and Metastases
SRS is great for treating brain tumors and metastases. It’s a non-surgical option that uses high-dose radiation. This method targets the tumor without harming nearby healthy tissue.
It’s perfect for tumors that are hard to reach or for those who can’t have surgery. Recent studies show SRS is very effective for brain metastases. For example, a new treatment kept 5 patients with GBM tumor-free, with 2 showing almost complete recovery.
Functional Disorders and Vascular Malformations
SRS also helps with functional disorders and vascular malformations. It’s very good at treating trigeminal neuralgia, giving patients relief from severe pain. SRS is also used to treat AVMs, aiming to stop future bleeding.
Its precision makes SRS a key tool for hard-to-treat conditions. We’ve seen great results with AVMs, with many patients seeing their malformation completely disappear.
SRS Results and Outcome Expectations
The results of SRS depend on the condition, the target’s size and location, and the patient’s health. Most patients find SRS easy to handle, with few side effects. For brain tumors and metastases, SRS can control the disease well, improving life quality and survival.
Condition | Treatment Outcome | Common Side Effects |
Brain Tumors/Metastases | Effective local control, improved survival | Fatigue, localized hair loss |
Trigeminal Neuralgia | Pain relief | Facial numbness, rare |
Arteriovenous Malformations | Obliteration of AVM, reduced bleeding risk | Rare, radiation-induced changes |
Results can vary, and choosing the right patient is key for the best outcome. We work with patients to set realistic goals and provide full care during treatment.
Comparing Side Effects and Recovery
When picking between traditional radiation therapy, Stereotactic Radiosurgery (SRS), and Stereotactic Body Radiation Therapy (SBRT), side effects and recovery are key. Knowing these differences helps patients and doctors choose the best treatment.
Common Side Effects of Conventional Radiation
Traditional radiation therapy affects both cancer cells and healthy ones. It can cause fatigue, skin changes, and hair loss. The severity depends on the treatment’s dose, duration, and where it’s applied.
“Radiation therapy side effects can be tough,” says a radiation oncologist. “But knowing them helps patients prepare.” We tell patients to talk to their healthcare team about these effects to manage them better.
Side Effects of Stereotactic Radiosurgery
SRS gives high doses of radiation to tumors, sparing healthy tissue. This makes SRS have fewer side effects than traditional radiation. But, it can cause headaches, nausea, and fatigue, mainly if it’s near important areas.
SBRT Side Effects and Management
SBRT delivers high doses of radiation in a few fractions. It can cause side effects like fatigue, nausea, and pain at the treatment site. Managing these side effects is key to keeping patients’ quality of life. We help patients closely monitor and manage these effects.
Recovery times after radiation therapy vary. Patients getting SRS or SBRT usually recover faster than those with traditional radiation. But, everyone’s recovery is different, based on their health and other conditions.
Understanding side effects and recovery for different radiation therapies helps patients prepare. It lets them make informed choices about their care.
Patient Selection and Personalized Treatment Decisions
The success of radiation treatment depends on choosing the right patients and making treatment plans that fit each one. We know that every patient is different. So, we use a personalized approach to radiation therapy.
Who Benefits Most from Conventional Radiation?
Conventional radiation therapy is best for patients with tumors that respond well to it. It’s also good when the tumor is in a place where healthy tissues can be kept safe. We look at the tumor type, stage, and the patient’s health to decide if conventional radiation is right.
Patients with big tumors or those near important structures might do well with conventional radiation. This method spreads out the dose over several treatments. It helps protect the healthy tissues around the tumor.
Ideal Candidates for Stereotactic Treatments
Stereotactic radiosurgery (SRS) and stereotactic body radiation therapy (SBRT) are best for small, well-defined tumors. These treatments are great for tumors in hard-to-reach places or for those who can’t get traditional radiation because of previous treatments.
We check the tumor’s size, location, and the patient’s medical history. This helps us decide if SRS or SBRT is the best choice for them.
Shared Decision-Making in Radiation Oncology
In radiation oncology, making decisions together is key. We work with patients and their families to understand their wishes, worries, and values. This teamwork makes sure the treatment plan meets the patient’s needs and hopes.
We talk about all the treatment options and their pros and cons. This way, patients can make choices about their care that feel right for them.
Advanced Radiation Techniques: IMRT vs SBRT
IMRT and SBRT are leading-edge radiation therapy methods that have greatly improved cancer treatment. It’s vital for doctors and patients to know the differences between these advanced techniques. We’ll dive into the specifics of IMRT and SBRT, looking at their methods and uses in cancer care.
Understanding Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy, or IMRT, is a high-tech way to target tumors with precise radiation beams. It allows for higher doses to the tumor while protecting healthy tissues. IMRT is great for treating complex or irregular tumors.
IMRT uses advanced computers to adjust the radiation beam intensity. This creates a dose that closely matches the tumor’s shape. This precision helps reduce side effects and improves treatment results.
Comparing IMRT and SBRT Approaches
IMRT and SBRT are both advanced radiation methods, but they differ in their approach and use. SBRT gives high doses in a few fractions, perfect for small, well-defined tumors. IMRT, on the other hand, can treat a wider range of tumor sizes and locations, often in more fractions.
SBRT requires extremely high precision, often using advanced imaging for accurate targeting. IMRT also needs precision but is more flexible with fractionation schedules.
Clinical Decision-Making Between Techniques
Choosing between IMRT and SBRT depends on several factors. These include tumor size, location, and the patient’s health. We consider the tumor’s proximity to critical structures, its radiosensitivity, and the patient’s treatment tolerance.
In some cases, combining techniques is best. For example, IMRT might treat larger areas at risk, while SBRT boosts dose to a specific tumor site. Our team works together to find the best treatment plan for each patient.
The Multidisciplinary Approach to Radiation Oncology
In radiation oncology, working together is key. We know that treating cancer well needs a team effort from different medical fields.
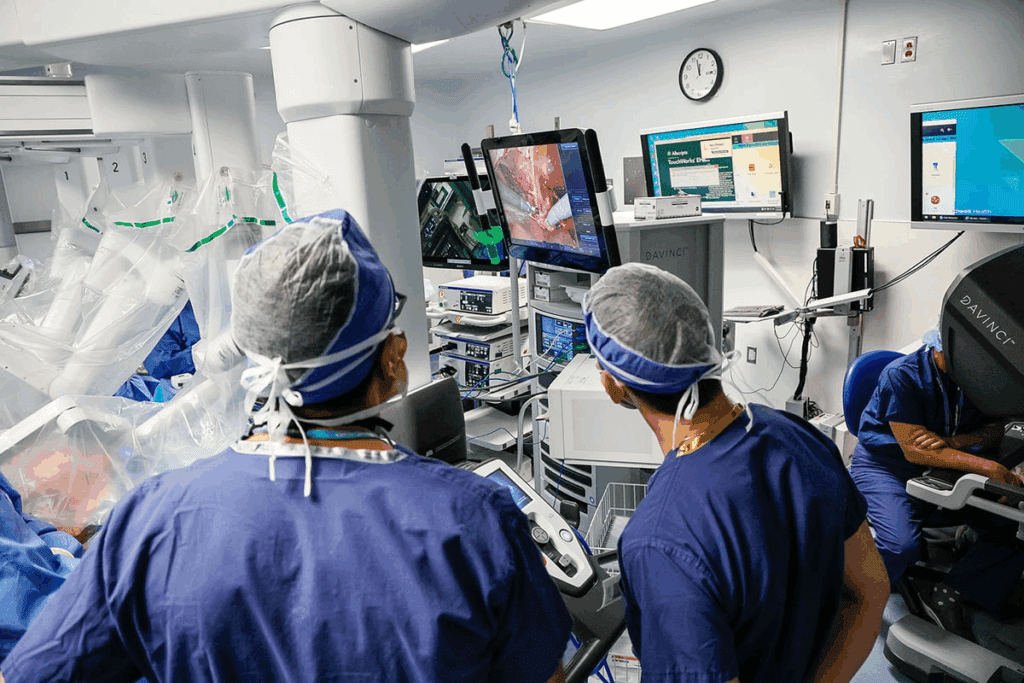
The Radiation Oncology Team
A team in radiation oncology includes experts like doctors, physicists, therapists, and nurses. Each one is important for the treatment. Doctors plan the radiation, and physicists make sure it’s safe and right.
Coordination with Surgery and Medical Oncology
Working with surgery and medical oncology is vital. We team up to plan treatments that use radiation, surgery, and chemotherapy together. This teamwork helps make care better for patients.
Patient Support During Treatment
Supporting patients is a big part of our work. Radiation therapy can be tough, both in body and mind. Our team offers full support, like nutrition advice, mental help, and teaching about side effects. We focus on the whole patient to make their experience better.
Our multidisciplinary way helps us give top-notch care to cancer patients. It meets their complex needs in a caring way.
Technology and Equipment in Modern Radiation Delivery
Advanced systems have changed how we fight cancer. These systems make radiation treatment more precise and efficient. This leads to better results for patients.
Linear Accelerators and Specialized Machines
Linear accelerators (LINACs) are key in today’s radiation therapy. They speed up electrons to make X-rays that hit tumors accurately. Machines with advanced imaging can adjust treatment in real-time.
Some big improvements include:
- Image-guided radiation therapy (IGRT): Uses X-rays, CT scans, or MRI for precise tumor targeting.
- Intensity-modulated radiation therapy (IMRT): Changes the beam’s intensity to match the tumor’s shape.
- Volumetric modulated arc therapy (VMAT): Treats in a continuous arc, making it faster and more efficient.
SRT Systems and Emerging Technologies
Stereotactic radiation therapy (SRT) systems, like CyberKnife and TrueBeam, are at the top of precision. They use advanced robotics and imaging for accurate tumor treatment.
New technologies are expanding what’s possible in radiation therapy. For example:
- Proton therapy: Uses protons to destroy cancer cells, with benefits in some cases.
- MR-guided radiation therapy: Mixes MRI with radiation for better soft-tissue contrast and real-time guidance.
Quality Assurance in Radiation Delivery
Ensuring radiation delivery is accurate and safe is critical. Quality assurance (QA) programs test and maintain equipment. They also train radiation oncologists and technologists.
Key QA aspects include:
- Regular calibration and testing of equipment.
- Strong quality control for treatment planning and delivery.
- Continuous education for the radiation oncology team.
Cost, Insurance, and Accessibility Considerations
Understanding the cost of radiation therapy is key for making smart choices. The cost can change a lot based on the type and where you get it.
Billing and CPT Codes
Knowing how billing works and what CPT codes mean is important. CPT77435 is used for Stereotactic Body Radiation Therapy (SBRT). We’ll explain how different CPT codes apply to different treatments.
- CPT77435: Stereotactic body radiation therapy, treatment delivery
- Other relevant CPT codes for radiation oncology services
Talking to your doctor and insurance company is a must to know your treatment costs.
Insurance Coverage for Different Radiation Modalities
Insurance for radiation therapy changes based on the type and your plan. We’ll cover the basics of insurance for different radiation therapies.
Key Points to Consider:
- Most plans cover conventional radiation therapy.
- SRS and SBRT might need special approval.
- IMRT and other advanced methods might need pre-approval too.
Check your insurance before starting treatment to avoid surprises.
Geographic Availability of Advanced Radiation Techniques
Access to advanced treatments like SRS and SBRT varies by location. Big cancer centers and specialized departments are more likely to offer these.
It’s wise to look into local options and talk to your doctor. This helps find the best treatment for you, considering your location and insurance.
Conclusion
We’ve looked into radiation therapy and stereotactic radiosurgery, showing their differences and uses. We’ve seen how modern technology has improved these treatments. A team approach in radiation oncology is key for complete patient care.
The role of stereotactic radiosurgery and radiation therapy is vital in cancer treatment. These methods offer precise and effective care. This allows doctors to tailor treatments to each patient’s needs.
The future of these treatments is bright, with new tech and planning methods on the horizon. We can look forward to better patient results and quality of life. This shows how important these treatments are in the fight against cancer.
FAQ
What is radiation therapy, and how does it work?
Radiation therapy is a treatment for cancer. It uses high-energy particles or waves to kill or damage cancer cells. The radiation is aimed directly at the tumor, slowing its growth or killing it.
What is the difference between radiation therapy and stereotactic radiosurgery?
Radiation therapy is a wide term for many treatments. Stereotactic radiosurgery (SRS) is a precise method. It gives a high dose of radiation to a small tumor or lesion.
What is SBRT, and how is it different from conventional radiation therapy?
Stereotactic Body Radiation Therapy (SBRT) is a precise treatment. It gives a high dose of radiation to a specific area in a few fractions. It’s different because of its precision and shorter treatment time.
What are the common abbreviations used in radiation oncology?
Common terms include RT (radiation therapy), XRT (external beam radiation therapy), SRS (stereotactic radiosurgery), SBRT (stereotactic body radiation therapy), and IMRT (intensity-modulated radiation therapy).
How long does it take for SBRT to work?
SBRT’s effects vary by cancer type, tumor location, and patient factors. Symptoms may improve in weeks to months after treatment.
What are the side effects of SBRT, and how are they managed?
Side effects include fatigue, nausea, and pain. Management includes medication, lifestyle changes, and monitoring by the radiation oncology team.
What is the difference between IMRT and SBRT?
IMRT uses precise doses from multiple beams. SBRT gives a high dose to a specific area in a few fractions.
How is patient selection done for different types of radiation therapy?
Patient selection involves evaluating medical history, tumor characteristics, and health status. The team decides the best treatment for each patient.
What is the role of a multidisciplinary team in radiation oncology?
A team includes radiation oncologists, medical physicists, and therapists. They work together to provide care to patients.
How is radiation therapy billed, and what are the relevant CPT codes?
Billing uses specific CPT codes, like CPT77435. The process varies by insurance and location.
Is radiotherapy the same as radiation therapy?
Yes, both terms describe using radiation to treat cancer.
What is stereotactic radiosurgery used for?
It treats brain tumors, vascular malformations, and functional disorders.
What are the benefits of SBRT in cancer treatment?
SBRT is precise, short, and effective. It’s great for hard-to-reach tumors.
References
National Center for Biotechnology Information. Radiation Therapy Versus Stereotactic Radiosurgery for Cancer. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3656557





