Last Updated on October 21, 2025 by mcelik
Sickle cell anemia affects millions worldwide, causing significant health challenges. It’s a genetic disorder that alters the shape of red blood cells, leading to various complications. We will explore the causes, symptoms, and management of this condition.
Understanding sickle cell disease is key for effective management and support. Our guide aims to provide insights into the condition, its impact, and the latest treatments available.
Sickle cell anemia changes the shape and function of red blood cells. We will dive into this condition to grasp its effects.
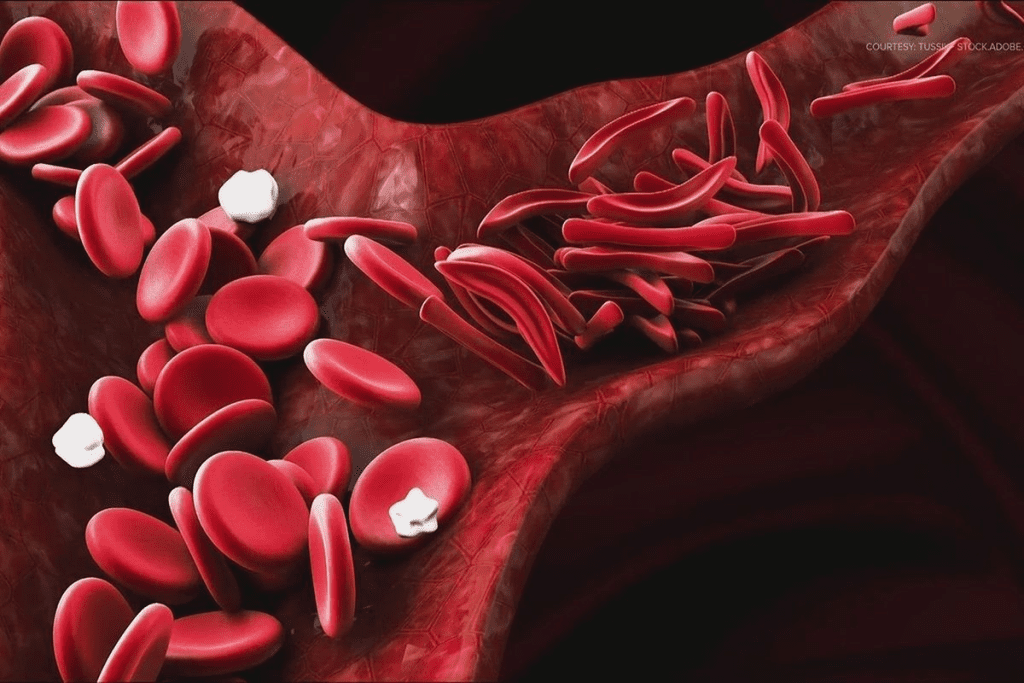
Sickle cell anemia is a genetic disorder. It causes red blood cells to be sickle or crescent shaped instead of their usual disk shape. This shape change leads to health problems like anemia, infections, and pain episodes.
The symptoms of sickle cell disease vary from person to person. Common signs include anemia, pain episodes (crises), swelling in hands and feet, and more infections. Knowing these symptoms is key to managing the disease well.
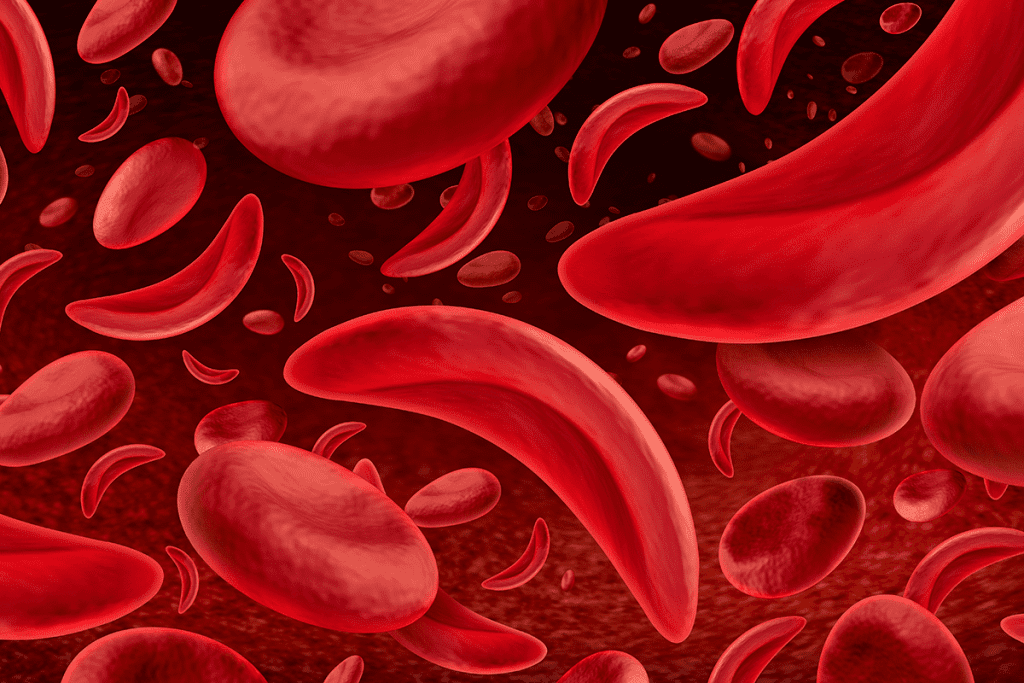
Normal red blood cells are flexible and disk-shaped. They can easily move through blood vessels. On the other hand, sickled red blood cells are stiff and crescent-shaped. They struggle to pass through smaller blood vessels.
Understanding the difference between normal and sickled red blood cells is key. This knowledge helps healthcare providers create better treatment plans. It improves the lives of those with sickle cell anemia.
Sickle cell anemia comes from a change in the HBB gene. This gene makes the beta-globin part of hemoglobin. This change makes abnormal hemoglobin, called hemoglobin S. Knowing about this change helps us understand the disease.
The HBB gene mutation happens on chromosome 11. It changes glutamic acid to valine at the sixth spot of the beta-globin chain. This creates hemoglobin S. The disease is inherited in an autosomal recessive pattern. This means you need two copies of the mutated gene, one from each parent, to have the disease.
Sickle cell disease is a classic example of a monogenic disorder. A single mutation greatly affects the disease’s symptoms. The sickle cell mutation is a prime example of how a single nucleotide change can have significant clinical implications.
Hemoglobin S is made because of the HBB gene mutation. When there’s less oxygen, hemoglobin S sticks together. This makes red blood cells bend into a sickle shape. This shape causes problems like vaso-occlusive crises and hemolytic anemia.
| Normal Hemoglobin | Hemoglobin S |
| Normal beta-globin chain | Mutated beta-globin chain (valine substitution) |
| Flexible red blood cells | Sickled red blood cells under low oxygen |
| Normal oxygen delivery | Impaired oxygen delivery |
The making of hemoglobin S and the sickling of red blood cells are key to sickle cell anemia. Knowing these steps is key to finding good treatments.
The genetic basis of sickle cell disease inheritance is key to understanding the condition’s transmission. Sickle cell disease is inherited in an autosomal recessive pattern. This means the disease shows up in those who get two bad hemoglobin genes, one from each parent.
To grasp the autosomal recessive inheritance pattern, it’s important to know. The genes for hemoglobin are on autosomes. A person with sickle cell disease has two bad hemoglobin genes. This leads to hemoglobin S instead of normal hemoglobin.
In autosomal recessive inheritance, both parents must carry the sickle cell gene. Carriers have one normal and one sickle cell gene. They are usually healthy but can pass the sickle cell gene to their kids.
When both parents are carriers, there’s a 25% chance their child will have sickle cell disease. There’s a 50% chance the child will be a carrier like each parent. And a 25% chance the child will have neither the disease nor be a carrier.
Carrier status means having one normal and one sickle cell gene, known as sickle cell trait. People with sickle cell trait are usually healthy. But they can pass the sickle cell gene to their kids.
They might experience symptoms like those of sickle cell disease under extreme conditions. But this is rare.
Understanding sickle cell trait and carrier status is key for genetic counseling. Carriers should know the risks and possibilities when planning a family. This is important if their partner is also a carrier or has sickle cell disease.
By knowing the inheritance patterns of sickle cell disease, families can prepare better. They can make informed decisions about their health and family planning.
The main cause of sickle cell anemia is a change in the hemoglobin molecule. This change leads to abnormal hemoglobin, called hemoglobin S (HbS). We will look at how this mutation affects red blood cells.
The process of cell sickling starts with the polymerization of HbS when it’s not oxygenated. This makes the red blood cell membrane stiff and sickle-shaped. When oxygen levels go back up, the shape changes back. But, this cycle of change and return can damage the cell over time.
Key factors influencing the polymerization of HbS include:
Several things can make sickling happen in people with sickle cell anemia. These include:
Knowing what triggers sickling is key to managing the disease. By avoiding or reducing these triggers, people with sickle cell anemia can have fewer sickling events. This can greatly improve their life quality.
Sickle cell disease shows a complex pattern around the world. It’s a big health issue, with different levels of occurrence in various places.
This disease is most common in warm and tropical areas. Places where malaria used to be common, like parts of Africa, the Middle East, India, and the Mediterranean, are hit hard.
The World Health Organization (WHO) says millions are affected globally. In sub-Saharan Africa, 1% to 4% of babies are born with it.
In the U.S., sickle cell disease is a big worry, mainly for African Americans. The Centers for Disease Control and Prevention (CDC) reports it affects 1 in 500 African American babies and 1 in 36,000 Hispanic American babies.
| Ethnic Group | Prevalence of Sickle Cell Disease |
| African American | 1 in 500 births |
| Hispanic American | 1 in 36,000 births |
| Middle Eastern | Variable, generally lower than African American |
Knowing about sickle cell disease’s spread is key. It helps in making better health plans and improving care for those affected.
Several factors can increase the chance of getting sickle cell anemia. Knowing these risk factors helps find people more likely to get the disease.
Sickle cell anemia hits certain ethnic and geographic groups harder. People of African descent are most affected, with the highest rates in sub-Saharan Africa. The Mediterranean, Middle Eastern, and Indian subcontinent also see higher rates.
Places where malaria used to be common also see more sickle cell anemia. This is because the sickle cell trait helps fight malaria. This has shaped the disease’s spread.
Having a family history of sickle cell anemia is a big risk factor. The disease is passed down in a specific way. You need two bad genes, one from each parent, to have it.
Carriers, with one good and one bad gene, are usually okay but can pass the bad gene. If both parents are carriers, each child has a 25% chance of getting sickle cell anemia.
| Family History | Risk of Sickle Cell Anemia |
| Both parents are carriers | 25% chance with each pregnancy |
| One parent is a carrier, the other has sickle cell anemia | 50% chance of being a carrier or having the trait |
| One parent has sickle cell anemia, the other does not carry the trait | 100% chance of being a carrier |
Knowing these risk factors helps spot sickle cell anemia early. This can greatly improve life for those affected.
It’s important to know the different types of sickle cell disease. This knowledge helps in managing and treating the condition. Sickle cell disease affects the hemoglobin in red blood cells, causing various symptoms.
Hemoglobin SS disease, also known as sickle cell anemia, is the most common and severe form. It happens when a person gets two mutated HBB genes, one from each parent. This leads to the production of hemoglobin S instead of normal hemoglobin.
Characteristics of Hemoglobin SS Disease:
Hemoglobin SC disease occurs when a person gets one mutated HBB gene for hemoglobin S and another for hemoglobin C.
Characteristics of Hemoglobin SC Disease:
Hemoglobin S beta thalassemia happens when a person gets the HBB mutation for hemoglobin S and a beta thalassemia mutation. Beta thalassemia affects the beta-globin subunit of hemoglobin.
Characteristics of Hemoglobin S Beta Thalassemia:
Here’s a summary of the different types of sickle cell disease and their characteristics:
| Type of Sickle Cell Disease | Genotype | Severity of Anemia | Risk of Complications |
| Hemoglobin SS Disease | SS | Severe | High |
| Hemoglobin SC Disease | SC | Mild/Moderate | Moderate |
| Hemoglobin S Beta Thalassemia | Sβ | Variable | Variable |
The sickle cell trait offers a big advantage in areas hit hard by malaria. This is mainly because it makes it harder for the malaria parasite to grow inside red blood cells.
People with the sickle cell trait (HbAS) are less likely to get sick from malaria. This is true, even for the worst kinds caused by Plasmodium falciparum. The sickle hemoglobin (HbS) in their red blood cells makes it tough for the parasite to thrive.
Mechanisms of Malaria Resistance: There are a few ways the sickle cell trait helps fight malaria. These include:
In places where malaria is common, the sickle cell trait is more likely to be passed on. This is because people with the trait are more likely to live and have kids. This way, they pass the trait to their children.
Impact on Population Genetics: The sickle cell trait’s advantage in malaria areas has big effects on population genetics. It has led to more people in some groups having the trait. This shows how genes, environment, and evolution work together.
To understand sickle cell disease, we must look at how it causes blood vessel blockage, red blood cell destruction, and inflammation. This disease is caused by sickled hemoglobin (HbS). It changes red blood cells into a sickle shape when there’s not enough oxygen.
Vascular occlusion is a key part of sickle cell disease. It happens when sickled red blood cells stick to the blood vessel walls. This causes blood vessels to block.
These steps lead to pain and damage to organs, common in sickle cell disease.
Hemolysis, or red blood cell destruction, is a big part of sickle cell disease. Sickled red blood cells are more likely to break down, causing chronic hemolytic anemia.
The effects of hemolysis include:
Inflammation is very important in sickle cell disease. The repeated blockages and lack of blood flow cause long-term inflammation. This harms the blood vessel walls.
Endothelial dysfunction means:
Inflammation and damaged blood vessel walls create a cycle that keeps sickle cell disease going.
Sickle cell crisis is a serious condition that affects people with sickle cell disease. It causes severe pain and can be life-threatening. This crisis happens when sickled red blood cells block blood vessels.
A vaso-occlusive crisis is a common and painful part of sickle cell disease. It happens when sickled red blood cells block blood vessels. This leads to tissue ischemia and pain.
Triggers for these crises include infections, dehydration, and extreme temperatures. Managing vaso-occlusive crises involves treating pain, staying hydrated, and fixing any underlying issues. Quick medical care is key to avoid lasting harm.
Acute chest syndrome is a serious complication of sickle cell disease. It shows up as a new lung issue on chest X-rays, often with fever, breathing problems, or chest pain. It’s a major cause of illness and death in those with sickle cell disease.
The management of acute chest syndrome includes oxygen, pain relief, and antibiotics. Blood transfusions may be needed in severe cases to prevent more harm.
Splenic sequestration is a serious issue, mainly in kids. It happens when red blood cells get stuck in the spleen. This leads to sudden anemia and can be life-threatening.
Management involves quick medical help, including blood transfusions. In some cases, removing the spleen may be needed to stop future problems.
Managing sickle cell disease requires a detailed treatment plan. Each patient’s needs are different. So, we tailor treatments to fit their specific needs.
Medications and Therapies
Medicines are key in treating sickle cell disease. Hydroxyurea is often used to lessen pain crises and reduce blood transfusions. We also use other drugs to handle infections and acute chest syndrome.
Therapies like physical and occupational therapy help too. Physical therapy improves mobility and reduces pain. Occupational therapy helps patients adapt and stay independent.
Blood transfusions are vital in managing sickle cell disease. They lower the risk of complications by reducing sickled red blood cells. We watch patients closely to avoid iron overload risks.
Stem Cell Transplantation
Stem cell transplantation can cure sickle cell disease. It replaces the patient’s bone marrow with healthy stem cells. We consider it for those with severe disease and a suitable donor, weighing benefits and risks.
In summary, treating sickle cell disease involves many approaches. These include medicines, therapies, blood transfusions, and sometimes stem cell transplantation. Our goal is to provide personalized care that improves each patient’s life and outcomes.
To reduce the effects of sickle cell disease, a complete management plan is needed. This includes preventive care, lifestyle changes, and better pain control.
Preventive care is key in managing sickle cell disease. Getting regular vaccinations, like pneumococcal and meningococcal, helps prevent infections. These infections can cause sickle cell crises.
Regular health check-ups are also important. They help monitor the condition and catch any issues early.
Good oral health is also vital. Regular dental visits can prevent mouth infections that can spread to other parts of the body.
| Vaccination | Recommended Schedule | Importance |
| Pneumococcal | Every 5 years | High |
| Meningococcal | Every 5 years | High |
| Influenza | Annually | Moderate |
Making lifestyle changes is important for managing sickle cell disease. Drinking plenty of water helps avoid dehydration, which can cause crises. Avoiding extreme temperatures is also key.
Nutritional balance is essential. Eating fruits, vegetables, and whole grains helps keep health in check. It’s also important to limit alcohol and smoking, as they can worsen the condition.
Managing pain is critical for those with sickle cell disease. We suggest a mix of medicines and non-medical methods like relaxation and therapy.
In severe cases, hospitalization may be needed. We work with patients to create pain plans that fit their needs.
With a full management plan, people with sickle cell disease can live better lives. This includes preventive care, lifestyle changes, and effective pain management.
Sickle cell anemia is more than a medical issue; it changes your life in many ways. It’s important to manage it well to keep a good quality of life.
Managing sickle cell anemia in daily life is key. Important things to consider include:
Having the right support can greatly improve life with sickle cell anemia. Some resources include:
Reproductive planning is vital for those with sickle cell anemia. Things to think about include:
By focusing on these areas, people with sickle cell anemia can handle the challenges better. This helps improve their overall quality of life.
The treatment for sickle cell disease is changing fast. New research and global efforts are leading the way. We’re learning more about the disease and finding new ways to treat it.
Gene therapy might cure sickle cell disease. It fixes the genetic problem that causes the disease. This could help hemoglobin work right again.
Studies are showing good results. Many clinical trials are testing gene therapy’s safety and how well it works.
Key aspects of gene therapy for sickle cell disease include:
Gene therapy could change sickle cell disease treatment. It might even cure it. Gene therapy is a big step forward in treating genetic diseases like sickle cell anemia. It could get rid of the symptoms and problems it causes.
Other new treatments are also promising. These include new medicines and ways like stem cell transplantation.
| Treatment | Description | Potential Benefits |
| Crisaborole | A topical phosphodiesterase 4 inhibitor | Reduces inflammation and potentially vaso-occlusive crises |
| Hematopoietic Stem Cell Transplantation | A procedure to replace the patient’s bone marrow with healthy stem cells | Potential cure for sickle cell disease |
Global efforts are key to fighting sickle cell disease. Groups like the Sickle Cell Disease Association of America and the World Health Organization are working hard. They aim to spread awareness, fund research, and make sure people get the care they need.
We must keep supporting research and global efforts. Together, we can find new treatments faster. This will help people with sickle cell disease live better lives.
Understanding sickle cell anemia is key to managing it well. We’ve looked at the genetic cause, how it’s passed down, and what happens in the body. This guide has covered a lot about the disease. Sickle cell disease is complex, with many factors at play. These include ethnic and geographic risks. To manage it, we need a mix of preventive care, lifestyle changes, and pain relief. Our look at sickle cell disease shows the need for more research and better treatments. We’ve highlighted the importance of caring for those affected. This includes giving them the support they need. New gene therapy and treatments are on the horizon. They could greatly improve life for those with sickle cell disease. We’re dedicated to providing top-notch healthcare and support to patients worldwide.
Sickle cell anemia is a genetic disorder. It affects the hemoglobin in red blood cells. This makes them misshapen and break down.
Sickle cell disease comes from a mutation in the HBB gene. This gene codes for the beta-globin subunit of hemoglobin. It leads to abnormal hemoglobin S.
Sickle cell disease is inherited in an autosomal recessive pattern. A person needs two copies of the mutated HBB gene to develop the disease. They get one from each parent.
Sickle cell trait happens when a person has one copy of the mutated HBB gene. They are a carrier of the disease. Sickle cell disease occurs when a person has two copies of the mutated gene. This leads to the full expression of the disease.
Symptoms include episodes of pain, anemia, infections, and other complications. These happen because of the abnormal sickling of red blood cells.
Blood tests detect hemoglobin S to diagnose sickle cell disease. Tests like hemoglobin electrophoresis or high-performance liquid chromatography (HPLC) are used.
There are main types of sickle cell disease. These include hemoglobin SS disease (sickle cell anemia), hemoglobin SC disease, and hemoglobin S beta thalassemia. Each type has different characteristics and implications.
A sickle cell crisis happens when sickled red blood cells block blood vessels. This causes tissue ischemia and pain. There are different types of crises, like vaso-occlusive crisis, acute chest syndrome, and splenic sequestration.
Treatment includes medications for pain and preventing complications. Blood transfusions are also used to reduce risks. In some cases, stem cell transplantation is considered.
Sickle cell disease can’t be prevented. But, genetic counseling and prenatal testing help families understand their risk. This helps them make informed reproductive decisions.
Research focuses on gene therapy and new treatments. This includes medications and gene editing technologies. There are also global efforts to improve care and outcomes for those with the disease.
Individuals can manage their condition through preventive care and lifestyle changes. They can also use pain management techniques. Staying connected with support resources is important too.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!