Last Updated on November 20, 2025 by Ugurkan Demir
Distinguishing sickle cell disease from other blood disorders is complex. It needs advanced diagnostics and trusted medical experts. At LivHospital, we follow international standards and focus on patient care. This ensures every patient gets a correct diagnosis and the right treatment from the start.
Sickle cell anemia differential diagnosis is marked by episodes of blood blockage and ongoing blood loss. Doctors confirm it by finding a lot of HbS and sometimes other abnormal beta globin chains. Accurate diagnosis is key for managing the disease and genetic counseling. This helps us offer care that meets each patient’s unique needs.
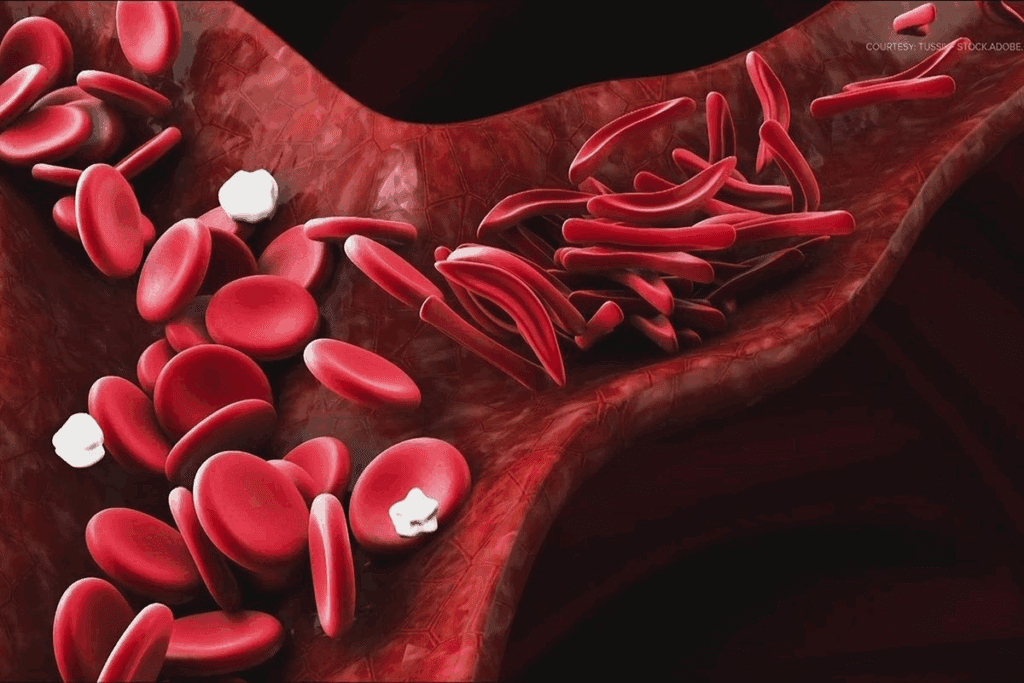
Sickle cell disease happens because of a key change in the HBB gene. This change leads to abnormal hemoglobin, called hemoglobin S (HbS). This abnormal hemoglobin causes the disease’s symptoms.
The disease starts with a single gene change in the HBB gene. This gene is for the beta-globin part of hemoglobin. The change swaps glutamic acid for valine at the sixth spot of the beta-globin chain, making HbS. This change can cause sickle cell trait or sickle cell disease, depending on the genes present.
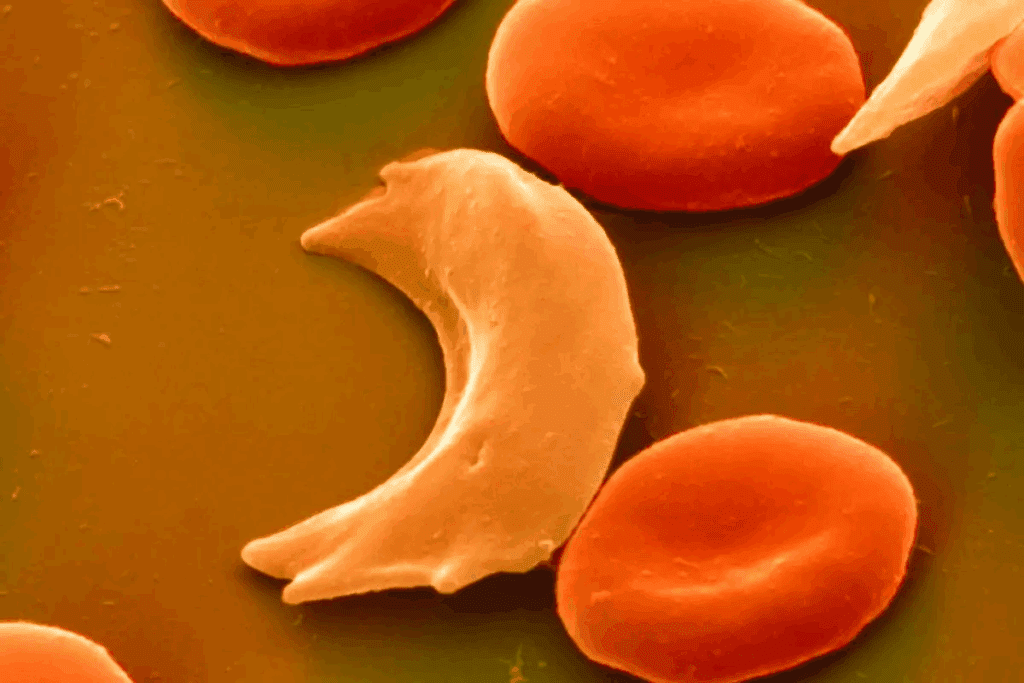
When there’s less oxygen, HbS forms long strands inside red blood cells. This makes the cells bend into a sickle shape. This shape change causes problems like more red blood cell destruction, blockages, and organ damage.
Sickle cell disease shows in many ways, like pain episodes, anemia, infections, and organ damage. Some main symptoms are:
It’s important to know the different types of sickle cell disease for proper diagnosis and treatment. Sickle cell disease includes several disorders caused by at least one hemoglobin S allele.
SS disease is the most common and severe form of sickle cell disease. People with SS disease have two hemoglobin S genes, one from each parent. This leads to a lot of abnormal hemoglobin, causing frequent and severe pain and anemia.
The symptoms of SS disease include:
Compound heterozygous forms happen when someone has one hemoglobin S gene and another abnormal gene. The most common types are SC disease and S-beta thalassemia.
SC Disease: SC disease is milder than SS disease. People with SC disease have one hemoglobin S gene and one hemoglobin C gene. Symptoms can include:
S-Beta Thalassemia: S-beta thalassemia happens when someone has one hemoglobin S gene and one beta-thalassemia gene. The severity can vary, depending on whether it’s S-beta+ or S-beta0 thalassemia.
Heterozygous sickle cell disease, or sickle cell trait, occurs when someone has one normal hemoglobin gene and one hemoglobin S gene. People with sickle cell trait usually don’t show symptoms but can pass the hemoglobin S gene to their children.
Under normal conditions, sickle cell trait has little clinical impact. But high altitude or intense physical activity can lead to complications.
Distinguishing sickle cell anemia from other hemoglobinopathies like beta-thalassemia and hemoglobin C disease is key. This accurate diagnosis is vital for effective management and genetic counseling.
Several conditions can look like sickle cell disease, making diagnosis tough. These include:
It’s important to tell these apart from sickle cell disease for the right treatment and care.
Getting the diagnosis right is critical for many reasons:
“Accurate diagnosis is the cornerstone of effective management of sickle cell disease and other hemoglobinopathies.”
Natalie, Hematologist
When sickle cell disease is suspected, a mix of clinical checks and lab tests are used.
| Test | Purpose |
| Complete Blood Count (CBC) | To evaluate hemoglobin levels and red blood cell indices |
| Hemoglobin Electrophoresis | To identify abnormal hemoglobin variants |
| Peripheral Blood Smear | To examine red blood cell morphology |
These tests help confirm the diagnosis and tell sickle cell disease apart from other conditions.
We stress the need for a detailed diagnostic process. This ensures an accurate diagnosis and proper care.
Diagnosing sickle cell disease right means knowing it apart from other hemoglobinopathies. This includes beta-thalassemia and hemoglobin C disease. Sickle cell disease is caused by abnormal hemoglobin, called hemoglobin S (HbS). Knowing the exact type of hemoglobinopathy is key because each has its own treatment and care plan.
We’ll look at the main differences between sickle cell disease and other related conditions. This includes beta-thalassemia and hemoglobin C disease. We’ll also talk about other hemoglobin types that might be part of the diagnosis.
Beta-thalassemia affects how the body makes beta-globin, a part of hemoglobin. It can range from mild to severe. It’s important to tell beta-thalassemia apart from sickle cell disease because they show different symptoms and need different treatments.
| Characteristics | Sickle Cell Disease | Beta-Thalassemia Major |
| Primary Hemoglobin Abnormality | HbS | Reduced/ Absent HbA |
| Clinical Features | Vaso-occlusive crises, anemia | Severe anemia, iron overload |
| Hemoglobin Electrophoresis | HbS predominant | HbF elevated, HbA reduced/absent |
Hemoglobin C disease can be mistaken for sickle cell disease because they share some symptoms. But, hemoglobin C disease is usually less severe.
Differential Diagnosis: Hemoglobin electrophoresis is key here too. It can tell HbS (sickle cell disease) from HbC (hemoglobin C disease).
Other hemoglobin types, like HbE and HbD, can also be part of the diagnosis. Each has its own traits and health effects.
Getting the right diagnosis with tests like hemoglobin electrophoresis, HPLC, and genetic testing is vital. It helps identify these variants and manage them properly.
Diagnosing sickle cell disease in the lab is complex. It requires several tests to accurately identify and manage the condition. This disease is caused by abnormal hemoglobin, known as hemoglobin S (HbS). It makes red blood cells take on a sickle shape under certain conditions.
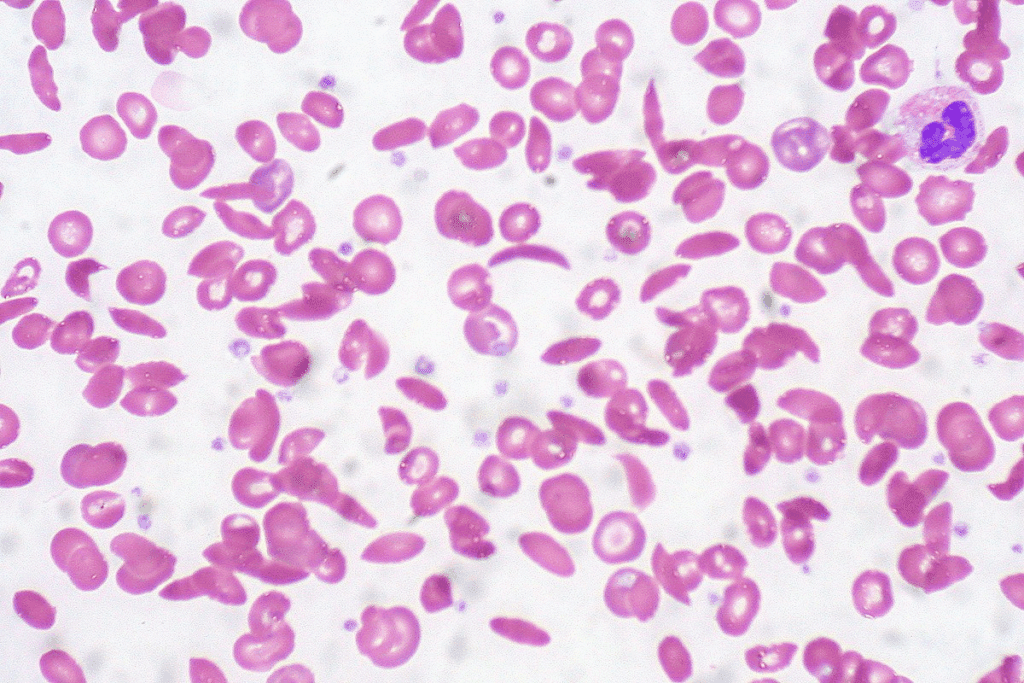
A complete blood count (CBC) is often the first test for sickle cell disease. It shows the hemoglobin level, hematocrit, and red blood cell indices. A peripheral blood smear looks for sickled red blood cells, a key sign of the disease.
Hemoglobin electrophoresis is a key test. It separates different hemoglobins by their electrical charge. This test is vital for finding HbS and other abnormal hemoglobin types.
HPLC is used to measure the different hemoglobins in blood. It’s very sensitive and can spot small amounts of abnormal hemoglobin.
Genetic testing looks at the HBB gene, which codes for the beta-globin subunit of hemoglobin. Mutations in this gene cause sickle cell disease. DNA analysis confirms the diagnosis and shows the individual’s genotype.
| Diagnostic Test | Purpose | Key Findings in Sickle Cell Disease |
| Complete Blood Count (CBC) | Assess hemoglobin level, hematocrit, and red blood cell indices | Anemia, variable MCV and MCHC |
| Peripheral Blood Smear | Examine morphology of red blood cells | Presence of sickled red blood cells |
| Hemoglobin Electrophoresis | Identify and quantify different hemoglobin types | Presence of HbS, possibly HbF and HbA2 alterations |
| High-Performance Liquid Chromatography (HPLC) | Quantify different hemoglobin types with high sensitivity | Accurate quantification of HbS and other variants |
| Genetic Testing and DNA Analysis | Analyze HBB gene for mutations | Identification of specific mutations causing sickle cell disease |
Understanding hemoglobin electrophoresis results is key for doctors to diagnose and treat sickle cell disease. This test is vital for spotting different hemoglobins in the blood. It’s essential for diagnosing hemoglobinopathies.
People without hemoglobinopathies usually have mostly Hemoglobin A (HbA). They also have a bit of Hemoglobin A2 (HbA2) and fetal hemoglobin (HbF). This pattern is used as a reference for abnormal results.
Homozygous sickle cell disease (HbSS) shows a specific pattern. It has a lot of Hemoglobin S (HbS) and high levels of HbF. HbA is usually not found in these patients.
Compound heterozygous forms like HbSC disease and HbS-beta thalassemia have unique patterns. HbSC disease has both HbS and Hemoglobin C (HbC). HbS-beta thalassemia shows HbS and varying amounts of HbA, based on the beta thalassemia mutation.
People with sickle cell trait (HbAS) have a mix of HbA and HbS. HbA is usually more common than HbS. This helps doctors tell the difference between sickle cell trait and disease.
It’s important for doctors to accurately read these patterns. This helps with diagnosis, genetic counseling, and managing sickle cell disease and trait. By knowing these patterns, healthcare providers can give better care and support to those affected.
Peripheral blood smears are key in diagnosing and managing sickle cell disease. They offer quick insights into red blood cell shapes. This is vital for spotting different sickle cell disease types.
In SS disease, the blood smear reveals sickle-shaped cells, or drepanocytes. These cells form when hemoglobin S clumps together in low oxygen. They are a clear sign of the disease.
In compound heterozygous forms, like HbSC disease or HbS-beta thalassemia, the smear shows a mix of SS disease and the other hemoglobinopathy’s features.
For example, in HbSC disease, the smear may show:
In sickle cell trait (HbAS), the blood smear is usually normal or shows slight issues, like:
Peripheral smear findings are essential for diagnosing, assessing disease severity, and tracking complications in sickle cell disease. Healthcare providers use these findings to understand the patient’s condition better and adjust treatment plans.
It’s important to know the difference between sickle cell disease and sickle cell trait. Sickle cell trait has one normal and one abnormal HBB gene. Sickle cell disease has two abnormal HBB genes. This difference affects how patients are treated and managed.
Sickle cell disease causes pain, anemia, and a higher risk of infections. This is because red blood cells sickle. People with sickle cell trait usually don’t have these problems unless they’re in extreme situations.
Key differences in clinical manifestations include:
Lab tests are key to diagnosing sickle cell disease and trait. Hemoglobin electrophoresis helps tell them apart by showing the types of hemoglobin.
Laboratory findings for sickle cell disease typically show:
Managing sickle cell disease is complex. It includes managing pain, preventing infections, and sometimes blood transfusions. People with sickle cell trait usually don’t need treatment but might get genetic counseling for family planning.
Genetic counseling is key for:
The future for those with sickle cell disease is uncertain. It depends on how severe the disease is, access to care, and other factors. People with sickle cell trait usually live a normal life without health problems related to their trait.
Prognostic factors for sickle cell disease include:
Understanding the difference between SS disease and SC disease is key in sickle cell disease care. Both are types of sickle cell disease but differ in genetics and symptoms.
SS disease is usually more severe than SC disease. People with SS disease often face more severe pain crises and are at higher risk for serious problems like acute chest syndrome.
SC disease, on the other hand, is generally milder. Some people with SC disease may not show symptoms or have fewer pain crises. Yet, SC disease can cause significant health issues, like during pregnancy or under stress.
Lab tests are vital in telling SS disease from SC disease. Hemoglobin electrophoresis shows HbS in both but with different patterns. SS disease has mostly HbS, while SC disease has both HbS and HbC in equal amounts.
High-performance liquid chromatography (HPLC) helps measure the different hemoglobin types. This test is useful in making a diagnosis.
SS disease increases the risk of infections, mainly from encapsulated bacteria, due to the loss of the spleen. SC disease, though less severe, can cause problems like splenic sequestration and, less often, pain crises.
Managing SS and SC disease involves some similar steps. These include supportive care, pain management, and preventive measures like vaccinations and folic acid. The approach depends on how severe the disease is.
Patients with SS disease might need closer monitoring and more aggressive treatments. This could include hydroxyurea to reduce pain crises and, in some cases, chronic blood transfusions.
Early detection of sickle cell disease is key. Newborn screening programs help find babies with the disease early. This early find allows for quick action to stop problems.
Newborn screening uses isoelectric focusing and/or HPLC. These tests spot abnormal hemoglobin, like HbS, which causes sickle cell disease. The results show if a baby is normal, a carrier, or has the disease.
Understanding these results is vital, says the American Academy of Family Physicians. It helps in diagnosing and managing the disease.
Infants with abnormal results need more tests to confirm sickle cell disease. Tests like hemoglobin electrophoresis and genetic testing are used. They show the exact type of disease.
Newborn screening has its hurdles, like false positives. It’s important to follow up quickly. This ensures babies get the right tests and care, easing family worries.
Infants with positive screens need a clear follow-up plan. This includes more blood tests, doctor visits, and genetic counseling. Early action helps prevent serious issues.
Getting a correct diagnosis for sickle cell disease is key. It helps in managing the disease and in genetic counseling. We’ve covered the disease’s basics, like how it works, its types, and how to test for it.
Knowing how to tell sickle cell disease apart from other blood disorders is vital. This knowledge helps doctors give the right treatment.
Having an accurate diagnosis is very important. It lets doctors start treatment right away. Genetic counseling is also essential. It helps families understand their genetic risks.
Doctors need to know how to diagnose sickle cell disease well. This knowledge helps them give the best care to their patients. By doing this, we can help patients get better and support them fully.
Sickle cell disease is diagnosed by ruling out other conditions. This includes beta-thalassemia and hemoglobin C disease. It also involves identifying conditions that mimic its symptoms.
Doctors use several tests to diagnose sickle cell disease. These include a complete blood count and a peripheral blood smear. They also use hemoglobin electrophoresis, high-performance liquid chromatography, and genetic testing.
Sickle cell disease is caused by a specific mutation in the HBB gene. This mutation leads to the production of abnormal hemoglobin S (HbS).
There are several types of sickle cell disease. These include homozygous SS disease and compound heterozygous forms like SC disease and S-beta thalassemia. There’s also heterozygous sickle cell disease, known as sickle cell trait.
Hemoglobin electrophoresis is key in diagnosing sickle cell disease. It identifies different hemoglobin variants, including HbS. This helps doctors distinguish between various forms of the disease.
Blood smears show sickled red blood cells and target cells in sickle cell disease. These findings help doctors diagnose the condition.
Sickle cell disease occurs when an individual has two abnormal hemoglobin genes. Sickle cell trait, on the other hand, is when someone has one normal and one abnormal gene. This usually doesn’t cause significant symptoms.
SC disease is a milder form of sickle cell disease compared to SS disease. It has different symptoms, lab findings, and treatment options.
Newborn screening is vital for early diagnosis of sickle cell disease. It allows for timely treatment and management, improving outcomes for affected infants.
Genetic testing confirms sickle cell disease diagnosis and identifies carriers. It also helps with genetic counseling for families.
HPLC separates and quantifies different hemoglobin variants. It aids in diagnosing and managing sickle cell disease.
Symptoms of sickle cell disease vary by type and severity. They include pain episodes, anemia, infections, and other complications.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!