Last Updated on October 21, 2025 by mcelik

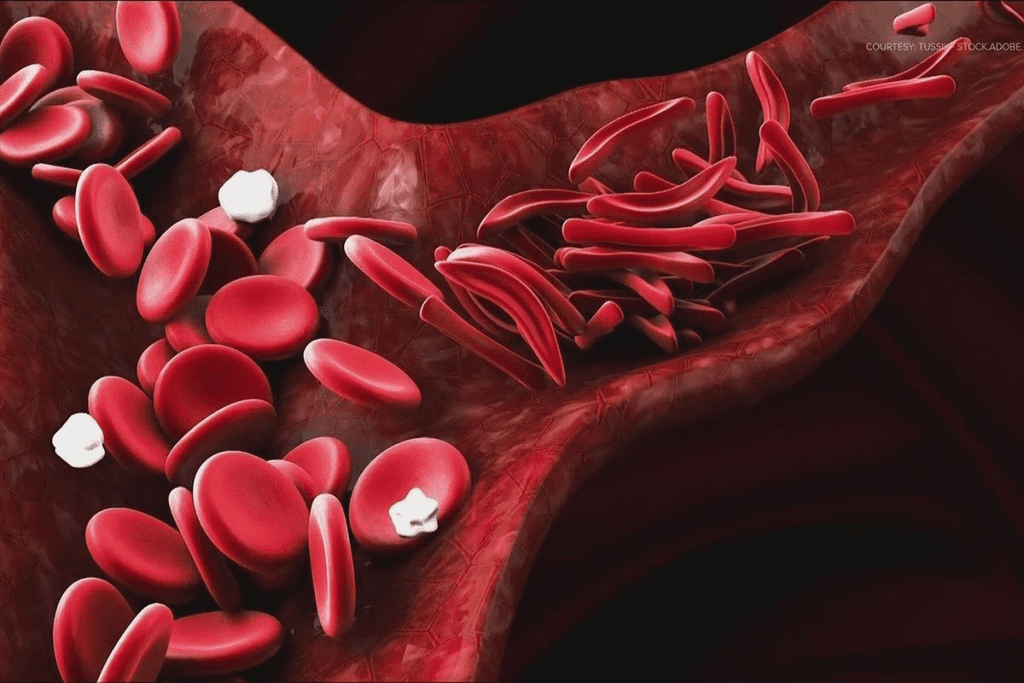
Sickle cell anemia affects millions worldwide, causing significant health issues. It impacts hemoglobin production and red blood cells.This genetic disorder causes red blood cells to become abnormally shaped, leading to multiple health complications.
Understanding sickle cell anemia is key for those affected and their families. This condition not only affects the individual but also has broader implications for public health.
Sickle cell anemia affects millions worldwide, causing significant health issues.
This genetic disorder impacts hemoglobin production, resulting in abnormally shaped red blood cells.
Understanding sickle cell disease is key to managing symptoms and improving life quality for those affected.
To grasp sickle cell anemia, we must explore its definition, history, and the science behind it. It’s a genetic disorder that changes the hemoglobin in red blood cells, making them sickle-shaped. This shape hinders blood flow, causing health issues.
Sickle cell anemia is caused by abnormal hemoglobin, called hemoglobin S. It comes from a gene mutation in the HBB gene. If someone gets two copies of this mutated gene, they might get sickle cell anemia.
The disease causes pain episodes, or crises, when sickled cells block blood vessels. These crises can be triggered by dehydration, high altitude, or stress.
| Characteristics | Normal Red Blood Cells | Sickled Red Blood Cells |
| Shape | Round and flexible | Sickle or crescent-shaped |
| Function | Normal oxygen delivery | Impaired oxygen delivery |
| Lifespan | Approximately 120 days | Shortened lifespan, often dying in 10-20 days |
He noticed sickle-shaped red blood cells in a patient. The condition is common in places where malaria is prevalent, as sickle cell trait protects against malaria.
Over time, managing sickle cell anemia has improved. We now focus on reducing pain crises and improving life quality. This shift has greatly helped those affected.
Understanding sickle cell anemia has also led to better genetic counseling and prenatal testing. This allows families to make informed choices about their reproductive health.
Sickle cell anemia starts with a problem in hemoglobin, a key protein in red blood cells. Hemoglobin carries oxygen around the body. Its right shape is key for red blood cells to work well.
Hemoglobin is made of four chains: two alpha and two beta. Each chain has a heme group that grabs oxygen. This setup lets red blood cells move easily through blood vessels.
Normal Hemoglobin Characteristics:
A change in the HBB gene causes bad hemoglobin, called hemoglobin S (HbS). This change makes hemoglobin S stick together when oxygen is low. This leads to sickle-shaped red blood cells.
Red blood cells with HbS turn sickle-shaped when oxygen is low. The HbS molecules stick together, making the cell stiff and sickle-shaped.
This sickling can be fixed in some cases. But, it keeps happening and damages the red blood cell membrane. This damage makes the cells break down early, a big problem in sickle cell anemia.
Consequences of Sickling:
| Effect | Description |
| Reduced Flexibility | Sickle-shaped cells are less able to navigate through narrow blood vessels. |
| Vaso-occlusion | Sickle cells can obstruct blood flow, leading to tissue ischemia. |
| Hemolysis | Premature destruction of red blood cells results in anemia. |
A leading researcher says, “Sickling of red blood cells is complex. It involves HbS levels and other hemoglobin types.” (
This complexity shows why sickle cell anemia needs a full management plan.
To understand sickle cell anemia, we must look at its genetic roots. It’s caused by a mutation in the HBB gene. This gene is responsible for the beta-globin subunit of hemoglobin.
Sickle cell anemia follows an autosomal recessive pattern. This means a person needs two defective hemoglobin genes, one from each parent, to have the disease. Those with only one affected gene are carriers.
Carriers usually don’t show the disease’s full symptoms but can pass the mutated gene to their kids. If both parents are carriers, there’s a 25% chance their child will have sickle cell anemia. There’s a 50% chance the child will be a carrier, and a 25% chance they won’t have the disease or be a carrier.
Several factors increase the risk of having a child with sickle cell anemia. These include a family history of the disease and being of African, Caribbean, or Middle Eastern descent. These groups are more likely to have the disease.
Sickle cell anemia affects millions globally, with high rates in areas where malaria was common. In the U.S., about 1 in 500 African Americans have sickle cell anemia. Around 1 in 12 African Americans carry the sickle cell trait.
The high prevalence of sickle cell anemia stresses the need for genetic screening and counseling. Knowing the genetic risks helps families plan better for the future.
The terms sickle cell anemia and sickle cell disease are often mixed up. But they mean different things. Sickle cell disease covers many genetic disorders that affect hemoglobin. Sickle cell anemia is the most common and severe form.
Sickle cell anemia comes from a specific gene mutation. This leads to abnormal hemoglobin, called hemoglobin S (HbS). Red blood cells then take on a sickle shape under certain conditions.
On the other hand, sickle cell disease includes other conditions. These include hemoglobin SC disease and hemoglobin S-beta thalassemia. They also involve abnormal hemoglobin but with different genetic changes.
Key differences between sickle cell anemia and other forms of sickle cell disease include:
Hemoglobinopathies are genetic disorders that affect hemoglobin. They include thalassemias and hemoglobin C disease, aside from sickle cell disease. Knowing about these related conditions is key for proper care and management.
| Condition | Description | Key Characteristics |
| Sickle Cell Anemia | A specific type of sickle cell disease caused by a mutation leading to hemoglobin S production. | Severe anemia, pain crises, increased infection risk |
| Hemoglobin SC Disease | A compound heterozygous condition involving both hemoglobin S and hemoglobin C. | Milder than sickle cell anemia, but can cause health issues |
| Hemoglobin S-Beta Thalassemia | A condition resulting from the combination of hemoglobin S and beta thalassemia mutations. | Severity varies depending on the beta thalassemia mutation |
It’s important to understand the differences between sickle cell anemia and other forms of sickle cell disease. This helps with accurate diagnosis and effective management. By clarifying the terms and exploring related hemoglobinopathies, healthcare providers can offer better care.
It’s important to know the signs and symptoms of sickle cell anemia to manage the disease well. The symptoms can vary a lot from person to person.
In young children, sickle cell anemia can cause anemia, jaundice, and swelling in the hands and feet. These happen because red blood cells get sickled and block small blood vessels.
Children might also get sick more often because their spleen doesn’t work right. This is called autosplenectomy. Finding out early through newborn tests is key to handling these symptoms.
As people with sickle cell anemia get older, they may face pain crises, acute chest syndrome, and other problems. Pain crises happen when blood cells block blood flow and cause tissue damage.
Adults might also deal with long-term damage to organs, like cardiac enlargement and renal failure. A good treatment plan is needed to manage these symptoms.
Sickle cell anemia has both chronic and acute symptoms. Chronic symptoms include ongoing anemia, jaundice, and possible organ damage over time.
Acute symptoms, like pain crises and acute chest syndrome, need quick medical help. Knowing the difference between these symptoms is important for proper care.
It’s important to know about sickle cell crisis to handle its acute problems. This crisis happens when sick red blood cells block small blood vessels. This causes tissue ischemia and pain.
Pain crises are a big part of sickle cell anemia. They come in different forms. The most common is the vaso-occlusive crisis. It happens when sickled red blood cells block blood vessels, causing severe pain.
Knowing the triggers and warning signs is key to preventing or managing sickle cell crises. Common triggers include dehydration, extreme temperatures, and infections.
| Trigger | Warning Signs |
| Dehydration | Increased thirst, dark urine, dizziness |
| Infections | Fever, chills, fatigue |
| Extreme Temperatures | Dizziness, nausea, headache |
Having good emergency management plans is vital for sickle cell crises. These include quick medical checks, staying hydrated, managing pain, and sometimes blood transfusions.
By knowing about the different pain crises, their causes, and emergency plans, people with sickle cell anemia can deal with these serious problems better.
Sickle cell anemia has long-term effects on many parts of the body. It affects the quality of life for those who have it.
Sickle cell anemia can harm organs like the spleen, kidneys, and heart. The spleen is often damaged because of sickled red blood cells. This can make it stop working or even get removed.
Organ Damage Overview
| Organ | Potential Damage | Consequences |
| Spleen | Repeated infarctions leading to fibrosis and loss of function | Increased risk of infections |
| Kidneys | Damage to renal microvasculature | Renal failure, proteinuria |
| Heart | Chronic anemia, leading to cardiac enlargement | Heart failure, arrhythmias |
People with sickle cell anemia are more likely to get infections. This is because their spleen doesn’t work right and their immune system is weak. They are at high risk for infections from bacteria like Streptococcus pneumoniae.
Sickle cell anemia and its complications can deeply affect a person’s mind and social life. The constant pain, hospital stays, and unpredictable crises can cause anxiety, depression, and make people feel isolated.
It’s important for family, friends, and mental health experts to offer support. New medical treatments and ways to manage the disease are also helping improve life for those with sickle cell anemia.
Finding sickle cell anemia early is key. Doctors use several tests to do this. Accurate diagnosis helps manage symptoms and avoid problems.
Newborn screening is vital for early detection. It’s a simple blood test for abnormal hemoglobin. Universal newborn screening is required in many places, like the U.S., for early treatment.
After newborn screening, blood tests confirm sickle cell anemia. These include:
Genetic analysis is key for families with sickle cell anemia history. It shows the risk for future pregnancies.
Pregnant women at risk can get prenatal testing. This includes:
Using these methods helps doctors create a detailed care plan. This improves life quality for those with sickle cell anemia.
Sickle cell anemia treatment has many options. Each one is chosen based on the person’s needs. The main goal is to manage symptoms, prevent problems, and improve life quality.
Medicines are key in treating sickle cell anemia. Hydroxyurea is often used. It helps reduce pain crises and may lower blood transfusion needs. Other drugs help with specific symptoms or complications.
Disease-modifying therapies aim to lessen the disease’s impact. These include drugs that boost fetal hemoglobin. This can help prevent red blood cells from sickling.
Blood transfusions are vital for some sickle cell anemia patients. They help lower risks of stroke and acute chest syndrome. Simple transfusions replace some red blood cells, while exchange transfusions replace more.
Pain management is key in sickle cell anemia care. Pain crises are managed with hydration, pain meds, and rest. Sometimes, hospital care is needed for severe pain.
Bone marrow transplantation can cure sickle cell anemia. It replaces the patient’s bone marrow with healthy marrow from a donor. This option is complex and risky, usually for those with severe disease.
Choosing bone marrow transplantation depends on the patient’s health, disease severity, and donor availability. It’s a personal decision made with careful consideration.
Sickle cell anemia is a genetic disorder that affects how the body makes hemoglobin. It requires a detailed plan to manage its symptoms and complications. Understanding how to reduce its impact on daily life is key.
Managing sickle cell anemia daily involves medication, lifestyle changes, and watching for complications. It’s important to drink plenty of water, avoid extreme temperatures, and see doctors regularly.
Changing your lifestyle can greatly improve life with sickle cell anemia. This includes eating right, exercising safely, and managing stress.
Nutritional Considerations are key. Eating a balanced diet can help manage symptoms.
Eating well is essential for those with sickle cell anemia. Certain foods can help ease symptoms and support health.
| Nutrient | Benefit | Food Sources |
| Folic Acid | Supports red blood cell production | Leafy greens, legumes, citrus fruits |
| Iron | Essential for healthy red blood cells | Red meat, poultry, fish, beans |
| Vitamin B6 | Helps in hemoglobin production | Fish, poultry, potatoes, bananas |
Chronic pain is a big challenge with sickle cell anemia. Managing pain involves medication, alternative therapies like acupuncture, and psychological support.
It’s vital for patients to work closely with their healthcare providers to create a pain management plan that works for them.
Sickle cell anemia is well-known, but sickle cell trait is not as clear. It happens when someone has one sickle cell gene and one normal gene. This makes them carry the sickle cell condition.
The main difference is in genetics and health effects. People with sickle cell anemia have two sickle cell genes. This leads to sickle-shaped red blood cells. On the other hand, those with sickle cell trait have one normal gene that helps, leading to fewer health problems.
Key differences include:
Carriers of sickle cell trait are usually healthy. But, they should know about some health risks. For example, at high altitudes or during intense exercise, they might face complications.
Health implications include:
Genetic counseling is key for families with sickle cell disease history. Knowing the risks of passing the condition to children helps with planning.
Genetic counseling considerations:
In conclusion, sickle cell trait is different from sickle cell anemia. But, knowing its implications is important for carriers and their families. Genetic counseling helps manage and understand the risks.
Sickle cell anemia is a big public health problem worldwide. It affects how red blood cells carry oxygen. This condition is found in many places, not just certain areas.
The number of people with sickle cell anemia varies by place. It’s more common where malaria used to be a big problem. This is because the sickle cell trait helps protect against malaria.
In places like sub-Saharan Africa, the Middle East, and parts of India, more people have it. This is different from other areas.
| Region | Prevalence of Sickle Cell Anemia |
| Sub-Saharan Africa | High |
| Middle East | Moderate to High |
| India (certain regions) | Moderate |
| Europe and North America | Low |
The sickle cell trait helps protect against severe malaria. This is why it’s more common in places where malaria is a problem. The genetic adaptation to malaria has resulted in a higher frequency of the sickle cell gene in these populations.
Even with better medical care, there are big gaps in how sickle cell anemia is treated. People in poorer areas often can’t get the care they need. This leads to worse health outcomes. Addressing these disparities is key to better managing sickle cell anemia globally.
In summary, sickle cell anemia affects many areas due to its genetics and the fight against malaria. Understanding these factors is vital for finding ways to manage and maybe even lower its occurrence worldwide.
New research in gene therapy and CRISPR technology is changing sickle cell anemia treatment. These advancements bring hope to those affected by this condition.
Gene therapy is a promising treatment for sickle cell anemia. It aims to fix the genetic issue causing the disease. Researchers are looking into different gene editing methods to change the faulty gene.
One big challenge is getting the corrected gene into the patient’s stem cells safely and effectively. Improvements in viral vectors and gene editing tools are helping solve this problem.
CRISPR-Cas9 technology has changed genetic editing, making it more precise. For sickle cell anemia, CRISPR can fix the specific mutation. This technology has huge promise for treating many genetic diseases.
Scientists are studying CRISPR-based therapies for sickle cell anemia. They edit stem cells outside the body and then put them back in. This could lead to a lasting cure.
Many clinical trials are underway for gene therapy and CRISPR treatments for sickle cell anemia. These trials are key to making these treatments work in real life.
Trials are looking into ways to increase fetal hemoglobin production. This could make the disease less severe. Others are working on gene therapy to directly fix the sickle cell mutation.
As research keeps moving forward, the future for sickle cell anemia patients looks brighter. With new studies and technologies, effective treatments and even a cure are becoming closer to reality.
Sickle cell anemia is a complex genetic disorder that affects millions worldwide. It causes significant morbidity and mortality. Understanding its causes, symptoms, and treatment options is key for effective management.
This article’s guide shows the importance of genetic inheritance patterns and risk factors. It also highlights the difference between sickle cell anemia and sickle cell disease. Recognizing signs and symptoms early can help reduce risks of acute complications and long-term damage.
Medical research has made great strides, including gene therapy and CRISPR technology. These advancements offer new treatment options. As research evolves, staying informed about new developments is vital for improving patient outcomes.
In conclusion, a multifaceted approach is needed to tackle sickle cell anemia. Combining medical advancements with patient education and support can greatly improve the quality of life for those affected by this debilitating disease.
Sickle cell anemia is a genetic disorder. It affects how red blood cells are made. This causes them to break down.
It’s caused by a gene mutation. This mutation affects hemoglobin production. It leads to abnormal hemoglobin S.
Symptoms include pain episodes and anemia. Infections and swelling in hands and feet are also common. The severity and frequency vary.
It’s diagnosed through newborn screening and blood tests. Genetic analysis is also used. Prenatal testing is available for at-risk families.
Sickle cell disease is a broader term. It includes several conditions. Sickle cell anemia is a specific type of this disease.
Treatments include medications for pain crises and blood transfusions. Pain management strategies are also used. Bone marrow transplantation is an option in some cases.
Bone marrow transplantation is the only cure. But it’s not suitable for everyone.
Sickle cell trait means carrying one mutated HBB gene. It can be passed to offspring.
People with sickle cell trait usually don’t have symptoms. But they may be at risk during extreme physical exertion.
It affects millions worldwide. It’s more common in areas where malaria is or was present. This is because it offers protection against malaria.
Research focuses on gene therapy and CRISPR. Other innovative treatments aim to cure or improve the disease management.
Daily management includes staying hydrated and avoiding extreme temperatures. Managing pain and following treatments and lifestyle changes is also important.
Long-term complications include organ damage and increased infection risk. Psychological and social impacts are also significant.
Yes, genetic counseling is vital. It helps families understand the risks of passing the condition to their children.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!