Last Updated on November 13, 2025 by
Recent studies show that over 95% of kids with sickle cell disease (SCD) in rich countries live into adulthood. This is a big step forward for kids with this condition.
Sickle cell disease is a serious lifelong illness. But, thanks to better medicine, kids with SCD have a much better chance at a long life. We’ll look at how far we’ve come in treating SCD, and what it means for kids today.
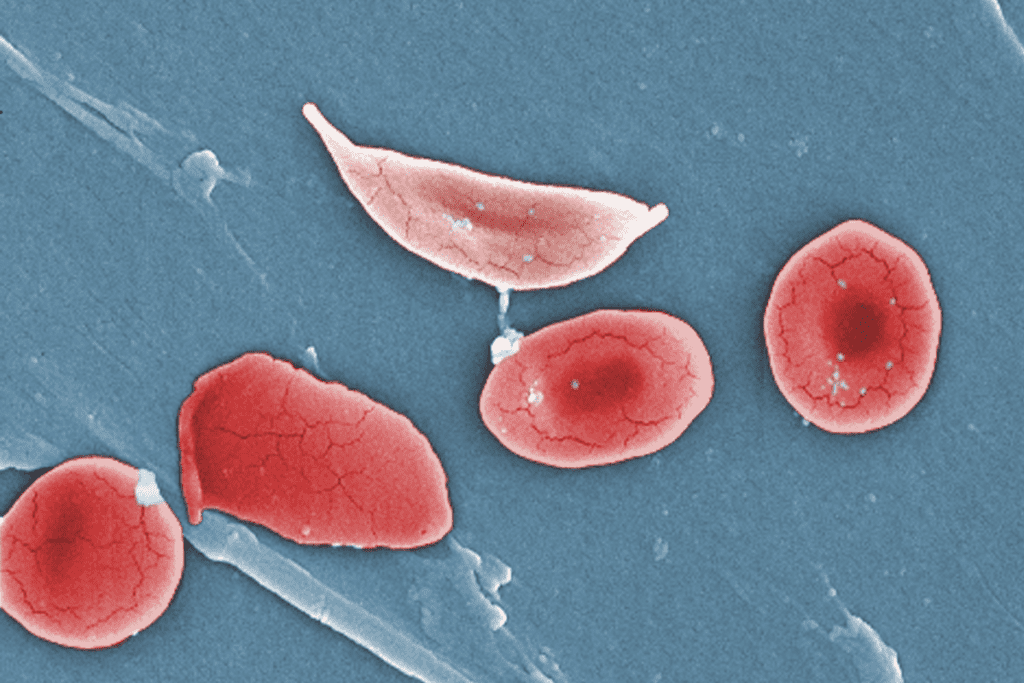
It’s important to understand sickle cell disease to help those affected, like children. SCD is a genetic disorder that changes how red blood cells are made. It makes them have a ‘sickle’ shape.
This condition is due to codominance of the sickle cell allele. This means people with one normal and one sickle cell allele will have both types of red blood cells.
Sickle cell disease comes from a mutation in the HBB gene. This gene is for the beta-globin subunit of hemoglobin. The mutation leads to sickle hemoglobin or hemoglobin S.
When someone has two copies of this mutated gene, they get SCD. It’s not caused by outside factors but is inherited in an autosomal recessive pattern.
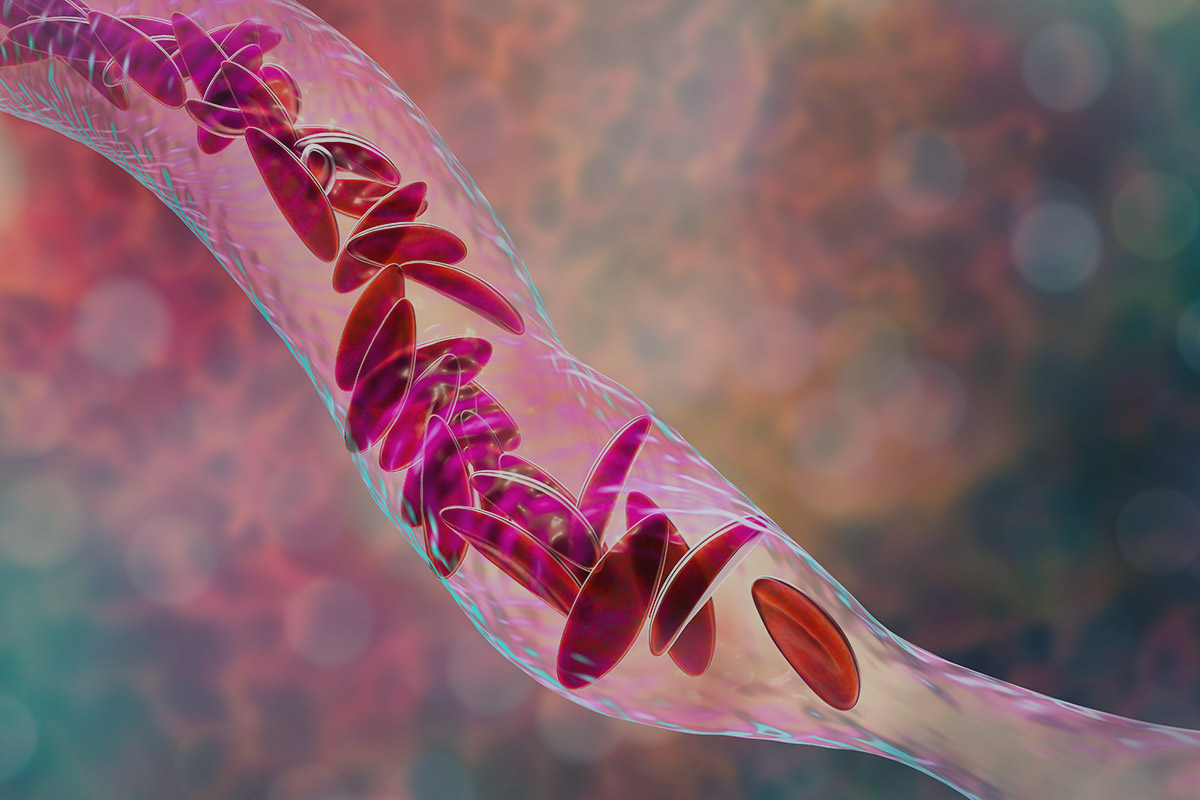
The sickle-shaped red blood cells die early, leading to anemia. Anemia means not enough healthy red blood cells to carry enough oxygen. These cells can also block small blood vessels.
This causes vaso-occlusive crises. These crises lead to pain episodes, organ damage, and other problems. SCD affects many parts of the body, like the spleen, kidneys, and heart.
Children with SCD face many risks. They can get sickle cell anemia symptoms like frequent infections, acute chest syndrome, and splenic sequestration. These can be very serious and need quick medical help.
Regular medical care is key. This includes getting vaccinated and taking antibiotics to prevent infections. It helps improve their life quality.
Knowing about sickle cell disease helps us manage it better. Early diagnosis and good care are essential to lessen its effects.
Sickle cell disease was once a death sentence for children. But thanks to better medical care, there’s now hope. Life expectancy for those with the disease has greatly improved.
Before modern medicine, survival rates for sickle cell disease were very low. Many children with SCD did not live to see adulthood. The disease was often deadly in early childhood, caused by severe infections and other complications.
Now, over 95% of children with SCD in developed countries live to adulthood. This big change comes from early diagnosis, preventive care, and better treatment for acute problems. These steps have made a huge difference, helping kids live longer and healthier lives.
In the United States, people with SCD can expect to live between 52-54 years on average. This is a big jump from the past and shows the positive effect of medical progress. While outcomes vary, this trend is hopeful and highlights the need for more research and better healthcare access for SCD patients.
We’re working hard to improve our understanding and treatment of SCD. Our goal is to provide top-notch healthcare and support to patients from around the world. The outlook for kids with sickle cell disease is getting brighter, thanks to ongoing research and medical breakthroughs.
Medical technology and treatment have greatly improved life for those with sickle cell disease (SCD). We’ve moved from just treating symptoms to preventing problems. This change has made a big difference in how long people with SCD can live.
Newborn screening has been a game-changer for SCD. It finds affected babies early, allowing for quick action. This early start has cut down on deaths in kids with SCD.
Preventive care is key in fighting SCD. Antibiotics like penicillin help prevent infections, a big killer in kids. Vaccines also help fight off sicknesses. These steps have greatly helped people live longer.
Treating sudden problems like sickle cell crises has gotten better. New ways to manage pain and keep patients hydrated have helped. Also, clear guidelines for treating these crises ensure patients get the best care fast.
New treatments aim to change the course of SCD. Hydroxyurea, for example, cuts down on pain episodes and chest problems. Other drugs like voxelotor and crizanlizumab also help lessen symptoms. These treatments could change the disease’s impact, making life better and longer.
Thanks to these medical leaps, people with SCD are living longer. Doctors can now give care that really meets their needs.
Together, these efforts offer hope for those with SCD. They show why we need to keep researching and finding new ways to help.
It’s key to know the critical times in a child’s life with SCD for good care. Each stage of a child’s life brings its own set of challenges.
Infancy and early childhood are very risky for kids with SCD because of high infection risks. Sickle cell anemia symptoms can show up early. It’s vital for parents to watch for signs like fever, fussiness, and not wanting to eat.
We suggest regular doctor visits and keeping up with vaccinations to lower these risks. Early detection through newborn screening has greatly helped kids with SCD. This early finding lets us start preventive care, like antibiotics, to lessen severe infection risks.

When kids with SCD get to school age and adolescence, they face new hurdles. They must learn to handle pain and understand the healthcare system. It’s important for us to help them find ways to cope and for doctors to guide them in managing their SCD.
Adolescents with SCD also need to take more control of their care. This can be tough. We must make sure they get the support and education to handle their condition on their own.
The move from pediatric to adult care is a big deal for people with SCD. This time needs careful planning to keep care going smoothly and tackle adult SCD challenges.
We must team up with both pediatric and adult doctors to make this transition easier. This means teaching the person about their condition, treatment choices, and the need for ongoing care.
Geographic and healthcare disparities greatly affect sickle cell disease outcomes. The quality of healthcare, access to specialized care, and socioeconomic status all play a role. These factors impact survival and quality of life for those with the disease.
In developed countries, sickle cell disease survival rates have improved. This is thanks to better medical care and early diagnosis through newborn screening. A study in Frontiers in Hematology shows how these advancements have helped.
But, in developing countries, challenges are different. Limited healthcare access, lack of disease awareness, and inadequate resources are common. These issues lead to lower life expectancy for those with SCD in these areas.
Having access to specialized sickle cell centers is key. These centers offer essential care like disease-modifying therapies and pain management. Patients who get care here often have better health and quality of life.
But, not all areas have these centers. This creates a care gap. It’s important to increase access to these centers or provide similar care locally.
Socioeconomic factors like income, education, and insurance status also matter. Families with more resources can get the care they need, including expensive treatments.
“The socioeconomic burden of sickle cell disease is substantial, and addressing these disparities is critical for better outcomes.”
Expert Opinion
When planning to improve SCD outcomes worldwide, we must think about these factors. By tackling geographic and healthcare disparities, we can ensure fair care distribution. This will lead to better lives for all with SCD.
Children with SCD need to thrive, not just survive. Medical progress has boosted survival rates, but quality of life is key. Effective care tackles physical, emotional, and social impacts of SCD.
Managing pain and symptoms is vital for a better life with SCD. Strategies include medication, acupuncture, and lifestyle changes. Good pain management lets kids fully enjoy daily life and feel better overall.
SCD poses unique hurdles in school and social life. Hospital stays and health issues can hinder learning and socializing. Supportive education and social programs are key to keeping kids on track academically and socially.
“Children with SCD need a supportive environment that understands their condition and accommodates their needs, enabling them to succeed academically and socially.”
The mental toll of SCD is significant. Kids and families may feel anxious, depressed, and stressed. Psychological support and counseling are essential for emotional well-being.
By focusing on these areas, we can greatly improve the lives of children with SCD. They can lead fulfilling lives despite their condition.
Today, kids with sickle cell disease have a much brighter future. Thanks to modern medicine, over 95% of them make it to adulthood. It’s important to know what sickle cell disease is and its symptoms to catch it early.
There’s been a lot of progress in treating SCD. New medical treatments and support systems have made life better for these kids. With the right care, they can live more normal lives.
We need to keep pushing forward in medical care and support. This will help improve the long-term outlook for those with SCD. We must support research and care efforts to give kids with sickle cell disease the best care possible.
Sickle cell disease (SCD) is a genetic disorder. It affects how the body makes hemoglobin. This causes red blood cells to be misshapen and break down. It leads to health problems.
SCD can cause anemia and infections. It also causes pain episodes. This is because sickle-shaped red blood cells get stuck in small blood vessels. This reduces blood flow and oxygen to vital organs.
Common complications include acute chest syndrome and stroke. Splenic sequestration and increased susceptibility to infections are also common. These can be life-threatening if not treated quickly.
With modern medical care, children with SCD live longer. Many live into their 50s. Studies suggest a median survival age of 52-54 years in countries like the United States.
Advances in newborn screening and prophylactic antibiotics have helped. So have immunizations and treatments for acute complications. Disease-modifying therapies have also improved survival and quality of life.
Infancy and early childhood are high-risk periods. This is because of susceptibility to infections. School-age and adolescence also bring challenges, like managing the disease and transitioning to adult care.
There’s a survival gap between developed and developing countries. Access to specialized care and socioeconomic factors are key. They determine long-term prognosis.
Managing pain and chronic symptoms is vital. It improves quality of life. It lets individuals with SCD fully participate in activities.
SCD can affect school attendance and performance. But, with proper support and management, individuals with SCD can reach their educational and social goals.
Living with SCD can lead to anxiety and depression. Support systems, like counseling and support groups, can help. They help individuals cope with the disease.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!