Last Updated on October 21, 2025 by mcelik
Did you know Sickle Cell Disease affects millions worldwide? Yet, many still believe it’s contagious. We are here to set the record straight. It’s not contagious; it’s a genetic disorder that affects how red blood cells carry oxygen.
We understand the concerns about this condition. It’s our goal to clear up any confusion. A sickle cell screening test can help identify if a person carries or has Sickle Cell Disease. The condition is inherited, not spread by contact with someone who has it. This is important for those affected and their families to know
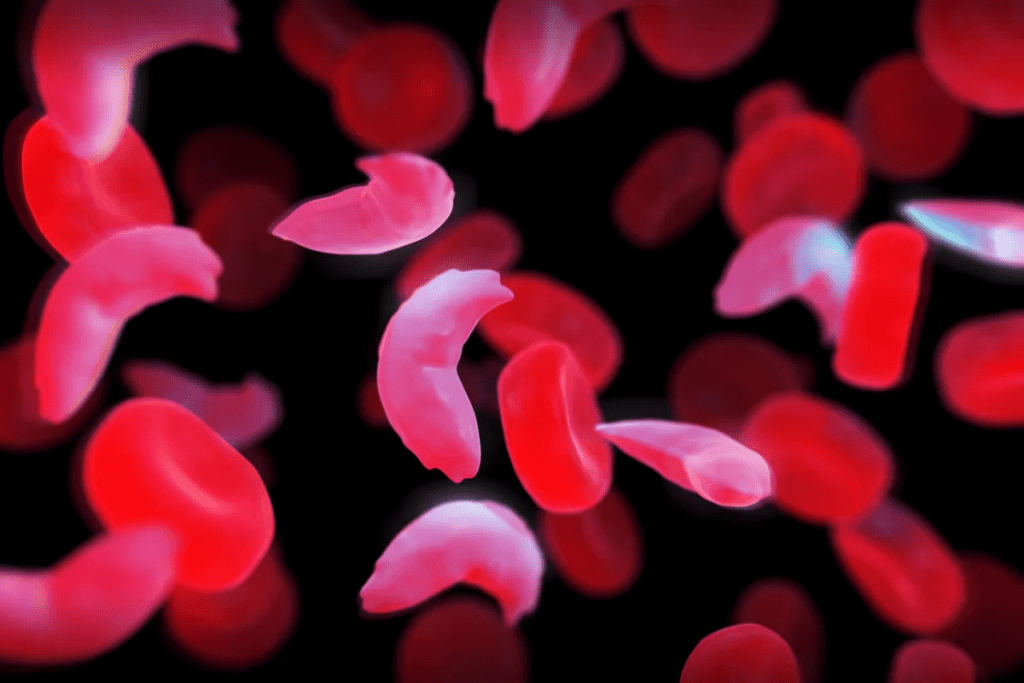
To grasp the full picture of Sickle Cell Disease, we must first understand its definition and how it affects the world. It’s a genetic disorder that changes how red blood cells make hemoglobin.
Sickle Cell Disease is a genetic disorder that changes the hemoglobin in red blood cells. Normally, these cells are flexible and round, moving smoothly through blood vessels. But for those with Sickle Cell Disease, the cells become stiff and crescent-shaped because of the abnormal hemoglobin.
This condition comes from a mutation in the HBB gene, which codes for a part of hemoglobin. If someone inherits two copies of this mutated gene, they usually get Sickle Cell Disease. Those who have one normal and one mutated gene are carriers. They don’t show all the symptoms but can pass the mutated gene to their children.
Sickle Cell Disease is a major health concern worldwide, especially in warm climates. It’s estimated that millions of people are living with this condition. In the United States, about 100,000 people have Sickle Cell Disease, mostly those of African descent.
The impact of Sickle Cell Disease goes beyond health issues. It also affects families socially and economically. Families dealing with the disease face high medical costs, lost work time, and emotional stress from managing a chronic illness.
Sickle Cell Disease is not contagious. It’s passed down from parents to their children. This happens because of a gene mutation in the HBB gene. This mutation leads to abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
Sickle Cell Disease is an autosomal recessive disorder. This means a person needs two defective copies of the HBB gene to have the disease. The genetic nature of the disease is why it’s not contagious. It can’t be spread through contact or exposure to someone with the disease.
Carriers of Sickle Cell Disease have one normal and one defective HBB gene. They usually don’t show the full symptoms of the disease. But, they can pass the mutated gene to their children. The chance of passing on the disease or trait depends on the genotypes of both parents.
The way Sickle Cell Disease is passed down is based on genetics. When both parents are carriers, there’s a:
Knowing how Sickle Cell Disease is transmitted helps families plan for the future. It’s important for making decisions about family planning and prenatal care.
Understanding the genetic basis of Sickle Cell Disease helps us see why it’s not contagious. It also shows how it’s passed down through generations. This knowledge is key for managing the disease and supporting those affected.
Sickle Cell Disease is a genetic disorder that affects how red blood cells make hemoglobin. The HbS gene mutation is the main cause. This mutation leads to abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
The HbS gene mutation happens in the HBB gene. This gene tells our bodies how to make a part of hemoglobin. A single nucleotide change in this gene causes the red blood cells to sickle under certain conditions.
The HbS gene mutation is a change in the HBB gene. This change leads to abnormal beta-globin. This abnormal beta-globin causes the red blood cells to sickle.
Having this mutation can cause Sickle Cell Disease if you inherit two copies of the mutated gene. If you inherit only one copy, you might be a carrier. Carriers usually don’t show symptoms but can pass the mutated gene to their kids.
Sickle Cell Disease follows an autosomal recessive pattern. This means you need to get a mutated HBB gene from both parents to have the disease. Carriers have one normal and one mutated gene. They don’t show symptoms but can pass the mutated gene to their kids.
The pattern of inheritance is as follows:
While the HbS gene mutation is common, other genetic variations can affect the disease’s severity. For example, having other abnormal hemoglobin genes can lead to different forms of Sickle Cell Disease.
Understanding these variations is key to predicting disease outcomes. It helps tailor management plans for each patient. Genetic counseling is also important for families to understand the risks for future generations.
It’s important to know the difference between Sickle Cell Disease and Sickle Cell Trait. Both are linked to the sickle cell gene but differ in health effects and genetic inheritance.
Sickle Cell Disease is a genetic disorder that affects hemoglobin production. It leads to sickled red blood cells and various health problems. Sickle Cell Trait, however, is when someone has one normal and one sickle cell gene. They are carriers but usually don’t show symptoms like those with Sickle Cell Disease.
People with Sickle Cell Disease have two sickle cell genes, one from each parent. Those with Sickle Cell Trait have one normal and one sickle cell gene. This genetic difference is key to understanding health risks and passing the condition to children.
Sickle Cell Trait is more common, especially in African, Mediterranean, and Middle Eastern populations. About 1 in 13 African Americans has it. While it’s usually harmless, it can cause health issues in certain situations like intense exercise or high altitudes.
Carrying the Sickle Cell Trait usually doesn’t cause health problems. But, it can lead to complications in specific situations like dehydration, intense exercise, or high altitudes. It’s crucial for those with the trait to know these risks and take steps to avoid them.
Also, the trait affects family planning. Carriers should understand the risks of passing the trait or Sickle Cell Disease to their children. Genetic counseling can help those planning a family with Sickle Cell Trait.
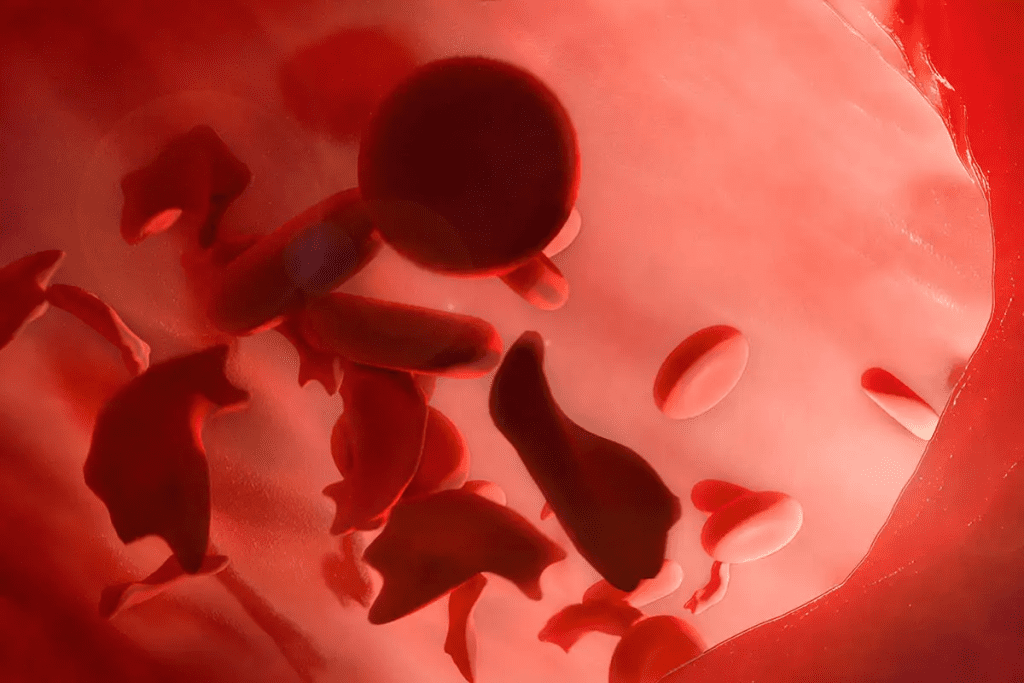
Sickle Cell Disease shows many symptoms, including sickle cell crises. These signs can differ from person to person. It’s key to know the common symptoms to manage the disease well.
Symptoms of Sickle Cell Disease vary in children and adults. Common signs include anemia, infections, and pain episodes. Pain crises happen when sickled red blood cells block blood vessels.
In kids, symptoms might include slow growth and development. Adults often face more infections and issues like acute chest syndrome.
A sickle cell crisis is a serious emergency needing quick help. Warning signs are severe pain, trouble breathing, and fever. Quick medical care is vital to avoid serious problems.
“Early recognition and treatment of sickle cell crises can significantly improve outcomes for individuals with Sickle Cell Disease.”
People with Sickle Cell Disease face long-term health issues. These include organ damage, vision problems, and more infections. Regular medical check-ups and care can lessen these risks.
Sickle Cell Disease is often found early in life, thanks to newborn screening programs. This early catch is key for managing the disease well and starting care early.
Sickle Cell Disease is usually found in infancy or early childhood. Many countries have newborn screening to spot it soon after birth.A top hematologist says, “Early detection through newborn screening is a big step in managing Sickle Cell Disease. It lets us start treatment early and manage the disease better.”
“Newborn screening for Sickle Cell Disease has changed how we handle this condition. It lets us treat it before symptoms get bad.”
If not caught at birth, diagnosis might come later in childhood or adulthood. This is often due to symptoms like frequent infections, anemia, or pain episodes.
There are several ways to diagnose Sickle Cell Disease. The main test is hemoglobin electrophoresis, which sorts different hemoglobins in the blood. Other tests include:
These tests confirm the diagnosis and tell what type of Sickle Cell Disease you have.
It’s important to understand your test results. A diagnosis of Sickle Cell Disease means you have HbS hemoglobin. The results will also show if you have Sickle Cell Trait or another disease type.
Interpreting Test Results: Your doctor will explain the results in detail. They will talk about what it means for your health and your family’s. It’s crucial to ask any questions or concerns to fully grasp your diagnosis.
Getting a Sickle Cell Disease diagnosis can be tough. But with the right support and care, people can live full lives. We stress the need for comprehensive care and support to manage the disease well.
To find out if someone has Sickle Cell Disease, doctors use several tests. These tests help figure out if the disease is present, how severe it is, and what treatment is needed.
Blood tests are key in diagnosing Sickle Cell Disease. They check a blood sample for abnormal hemoglobin.
Complete Blood Count (CBC): A CBC is often the first test done. It shows the blood’s health, including if there’s anemia, which is common in those with Sickle Cell Disease.
Hemoglobin electrophoresis is a test that looks at the different types of hemoglobin in the blood. It’s vital for diagnosing Sickle Cell Disease and telling it apart from other hemoglobinopathies.
This test is great because it can spot the exact type of hemoglobinopathy, like Sickle Cell Disease (HbS) or others.
DNA testing finds the genetic mutations that cause Sickle Cell Disease. It’s especially useful for testing before a baby is born and for finding carriers.
DNA testing gives detailed genetic info. It helps with family planning and genetic counseling.
| Test Type | Purpose | Key Features |
| Blood Tests | Diagnose Sickle Cell Disease | Detects abnormal hemoglobin, assesses anemia |
| Hemoglobin Electrophoresis | Identify hemoglobin types | Distinguishes between different hemoglobinopathies |
| DNA Testing | Detect genetic mutations | Useful for prenatal diagnosis and carrier identification |
We’re here to guide you through the process of getting tested for sickle cell disease. This includes finding a testing center and understanding your results. Testing is key if you have a family history of the condition.
Finding a testing center is easy. Start by talking to your primary care doctor. They can point you to a lab or testing facility nearby. Hospitals and clinics also offer these tests. Look online for certified labs in your area.
Make sure the lab is accredited and knows how to test for sickle cell disease.
Tips for Finding a Testing Center:
At the testing center, you’ll have a simple blood test. A healthcare professional will take a blood sample from your arm. The blood goes to a lab for analysis.
The results usually take a few days to a week. This depends on the lab and the tests done.
It’s important to follow any pre-test instructions. This ensures your results are accurate.
Many insurance plans cover sickle cell disease testing. This is especially true if you have a family history or symptoms. Check with your insurance to see what’s covered.
Some plans might need pre-approval or have special requirements. Always call your insurance to ask about their policies on sickle cell disease testing.
Steps to Verify Insurance Coverage:
Newborn screening is key in finding sickle cell disease early. It uses a simple blood test, often with other tests for newborns.
Finding sickle cell disease early is vital. It lets doctors start treatment right away. The Centers for Disease Control and Prevention (CDC) says early screening can greatly reduce health problems and death. Early action can stop serious issues, making life better for kids.
The test for sickle cell disease is a heel prick blood test. It looks for abnormal hemoglobin, a sign of the disease. This test is done early in a baby’s life.
If a newborn tests positive, more tests confirm the disease. This lets doctors create a care plan for the child.
“Early diagnosis through newborn screening enables healthcare providers to monitor the child’s health closely and intervene promptly if any complications arise,” notes a leading pediatric hematologist.
After, care includes regular visits, shots, and sometimes antibiotics to prevent infections.
Nursing diagnosis and care are key in managing Sickle Cell Disease. Nurses can greatly improve life quality for those with this condition through effective care.
Nurses often face several common nursing diagnoses when caring for Sickle Cell Disease patients. These include:
An expert says, “Nursing care for Sickle Cell Disease must address physical, emotional, and psychological needs. This holistic approach is key to quality care.”
Nursing interventions are designed to meet each patient’s unique needs. For those in a sickle cell crisis, care may include:
A good care plan is tailored to the patient’s history, health, and preferences. Working with other healthcare teams is crucial for complete care.
Teaching patients about their condition is vital in nursing care for Sickle Cell Disease. Learning how to manage pain, prevent infections, and stay healthy empowers them. Support groups offer valuable resources and connections for those with Sickle Cell Disease.
Nursing professionals are essential in improving Sickle Cell Disease care. Through compassionate and informed care, nurses can significantly impact the lives of those affected.
Carrying the Sickle Cell trait means more than just knowing you have it. It’s about understanding how it affects your health and daily life. We’ll look at health tips, exercise advice, and when to see a doctor.
Most people with Sickle Cell trait are healthy. But, there are important health tips to follow. A top hematologist says, “Carriers are usually fine but can pass the trait to their kids.” Getting genetic counseling is key, especially when planning a family.
Carriers should also know about risks from too much exercise or high altitudes. Even though the trait itself doesn’t usually cause problems, knowing these risks can help avoid issues.
Exercise is good for everyone, including Sickle Cell trait carriers. But, they should be careful, especially with hard workouts or in harsh weather.
It’s smart for carriers to talk to their doctors about exercising safely. Listening to your body and not pushing too hard is important for staying healthy and active.
Even though carriers are usually healthy, sometimes they need to see a doctor. Signs like pain, blood in urine, or muscle damage after exercise are emergencies.
Regular doctor visits can catch problems early. It’s also important to tell doctors about your Sickle Cell trait, especially before surgery or if you’re feeling off.
In short, living with Sickle Cell trait means being proactive about your health. Knowing the health tips, being careful with exercise, and knowing when to see a doctor can help you live a happy and healthy life.
Managing Sickle Cell Disease involves many steps. It includes medical treatments and changes in lifestyle. These steps are key to improving life for those with the disease.
Medical treatments are crucial for managing Sickle Cell Disease. They aim to lessen the number and severity of crises. They also help manage symptoms and prevent serious problems.
Some common treatments include:
| Medication | Purpose | Benefits |
| Hydroxyurea | Reduces frequency of painful crises | Decreases need for blood transfusions, reduces risk of complications |
| Blood transfusions | Increases normal red blood cells | Reduces risk of complications, improves overall health |
| Pain management medications | Manages pain during crises | Provides relief, improves quality of life |
Lifestyle changes are also vital for managing Sickle Cell Disease. These changes help lower the risk of serious problems. They also improve overall health.
Recommended changes include:
Managing pain is critical for those with Sickle Cell Disease. Good pain management can reduce the severity and frequency of crises.
Some strategies include:
By using medical treatments, making lifestyle changes, and managing pain, people with Sickle Cell Disease can live better lives.
Recent years have brought big changes in treating Sickle Cell Disease. These changes offer new hope to patients around the world. They are making life better for those with the disease.
Today, treatments for Sickle Cell Disease include medicines and lifestyle changes. Hydroxyurea is one medicine that helps reduce pain crises. Blood transfusions are also common. They help by adding normal red blood cells to the body.
Doctors are now making treatment plans that fit each patient’s needs. This personalized care is key to managing Sickle Cell Disease’s complex symptoms.
New treatments for Sickle Cell Disease are very promising. Gene therapy is one area of research that’s exciting. It tries to fix the genetic problem causing the disease. Many clinical trials are testing its safety and effectiveness.
Other new treatments target specific parts of the disease. For example, some drugs aim to stop sickled red blood cells from sticking to blood vessel walls. This is a big problem in Sickle Cell Disease.
| Therapy | Description | Status |
| Gene Therapy | Aims to correct the genetic mutation causing Sickle Cell Disease | In Clinical Trials |
| New Medications | Target specific aspects of the disease process, such as reducing red blood cell adhesion | In Development |
| Blood Transfusions | Helps reduce the number of red blood cells that can sickle | Established Treatment |
Gene therapy could be a cure for Sickle Cell Disease. It aims to fix the genetic problem at its source. Early trials show promising results, with some patients seeing big improvements.
We’re hopeful about gene therapy for Sickle Cell Disease. As research goes on, it could become a main treatment in the future.
For those with Sickle Cell Disease, the right support and resources are key. They can greatly improve life quality. We focus on providing care that goes beyond just medical treatment. This includes emotional, educational, and financial support.
Support groups are vital for those with Sickle Cell Disease. They offer a sense of community and understanding. Here, people can share their experiences, get emotional support, and learn from others facing similar challenges.
Some notable organizations dedicated to Sickle Cell Disease support include:
These groups offer a lot of resources. They provide educational materials, advocacy, and support networks.
Understanding Sickle Cell Disease is crucial. We recommend the following sources for accurate information:
Staying updated on Sickle Cell Disease research helps make informed care decisions.
Managing Sickle Cell Disease can be expensive. Financial assistance programs can help. They offer aid for medical expenses, travel to appointments, and more.
| Program | Description | Eligibility |
| Patient Access Network Foundation | Provides financial assistance for medications and other medical expenses | Underinsured or uninsured individuals with Sickle Cell Disease |
| The HealthWell Foundation | Offers copay assistance for medications, treatments, and related expenses | Individuals with Sickle Cell Disease who meet income and insurance criteria |
| National Organization for Rare Disorders (NORD) | Provides information and assistance for rare diseases, including Sickle Cell Disease | Varies by program |
These programs can greatly help manage Sickle Cell Disease care costs.
Understanding Sickle Cell Disease is key to better management and support. We’ve looked into its genetic roots, how it’s passed down, and the differences between Sickle Cell Disease and Sickle Cell Trait.
Early detection and proper care can greatly enhance life quality for those with Sickle Cell Disease. There are many resources out there, like support groups, educational materials, and financial help programs, to aid in managing the condition.
By learning more about Sickle Cell Disease, we can offer better care and support. This summary on Sickle Cell Disease shows how vital ongoing research, awareness, and full care are.
We aim to provide top-notch healthcare with full support for patients from around the world. We urge people to get medical advice and use the resources available to manage Sickle Cell Disease well.
Sickle Cell Disease is a genetic disorder. It affects how red blood cells make hemoglobin. This causes the cells to misshapen and break down.
No, it’s not contagious. It’s passed down through genes from parents to children.
Sickle Cell Disease happens when a person has two abnormal hemoglobin genes. Sickle Cell Trait is when a person has one normal and one abnormal gene. This makes them a carrier but usually doesn’t cause the disease.
Doctors use blood tests to diagnose it. These include hemoglobin electrophoresis and DNA testing. They look for the abnormal hemoglobin gene.
Symptoms include anemia and episodes of pain. Infections and swelling in hands and feet can also happen. Some people may face more serious issues like stroke or organ damage.
Yes, treatments are available. These include medications, blood transfusions, and pain management. New therapies like gene therapy are also being explored.
Look for testing centers at local hospitals, clinics, or organizations focused on Sickle Cell Disease. Many healthcare providers also offer testing services.
Yes, newborn screening is mandatory in many places. It’s a simple blood test to detect the disease.
Testing involves a blood draw. Results take a few days to weeks. Your doctor will discuss the results and any next steps with you.
Yes, there are many support groups. They offer resources, education, and emotional support for those affected by Sickle Cell Disease.
Management includes medical treatments, lifestyle changes, and pain management. Regular check-ups with your doctor are also important.
Yes, people with Sickle Cell Trait usually have normal lives. But they should know their carrier status and talk to their doctor about any concerns.
Generally, Sickle Cell Trait doesn’t cause big health problems. But, intense physical activity or high altitudes can lead to complications.
It’s inherited in an autosomal recessive pattern. A child needs two abnormal hemoglobin genes, one from each parent, to have the disease.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!