Last Updated on November 26, 2025 by Bilal Hasdemir
Understanding the Signs Chemotherapy Is Affecting You
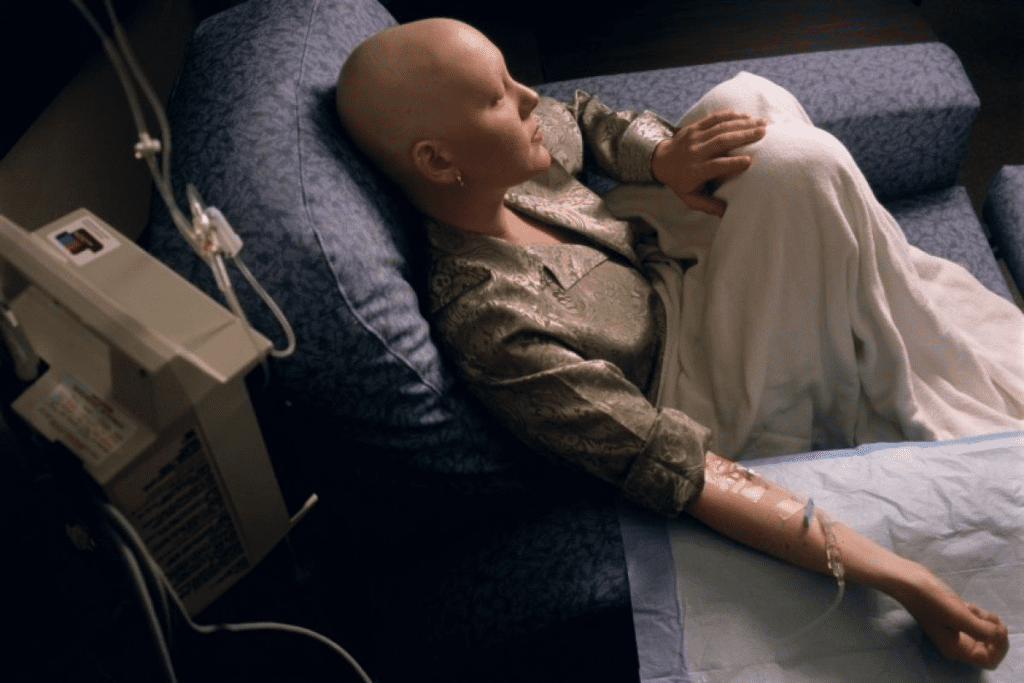
Going through chemotherapy is tough and can often feel isolating. Having a supportive friend or family member by your side can make a world of difference. Research shows that emotional support during cancer treatment can improve both recovery outcomes and mental well-being.
However, it’s equally important to understand the potential side effects of chemotherapy. While it’s a life-saving treatment, chemo can sometimes cause serious reactions. Recognizing the signs chemo is killing you ” or more accurately, signs that chemotherapy may be harming your body ” is essential for safety.
These signs might include extreme fatigue, severe infections, or unusual pain that feels different from typical treatment effects. Always communicate any concerning symptoms to your healthcare provider immediately. Early awareness and medical guidance can help ensure your treatment remains both effective and safe.
Key Takeaways
- Chemotherapy patients benefit significantly from emotional support.
- Companions can play a vital role in patient care during treatment.
- Understanding the side effects of chemotherapy is important.
- Knowing the warning signs of treatment harm is key for safety.
- Supportive care can improve patient outcomes and mental well-being.
The Role of Companions During Chemotherapy Sessions

Having someone by your side during chemotherapy can really help. They can offer emotional support and practical help. They also watch for any bad reactions, making the treatment safer and more comfortable.
Emotional Support Benefits for Patients
Companions can greatly help patients during chemotherapy treatment. Their presence can lower anxiety and stress. They can reassure, listen, and encourage, boosting a patient’s mental health.
- Reduce feelings of loneliness and isolation
- Provide emotional comfort and reassurance
- Help patients feel more connected and supported
Practical Assistance During Treatment
Companions also play a key role in chemo infusion. They help with paperwork, getting things, and talking to doctors. This lets patients focus on getting better.
- Assist with managing medication and treatment schedules
- Help with communication between patients and healthcare providers
- Provide transportation to and from treatment sessions
Monitoring for Adverse Reactions
Companions are also important for watching for side effects of chemotherapy. They can spot problems early and help quickly. Knowing the common side effects and when to get help is key.
Understanding the role of companions in chemotherapy is important. They offer emotional support, practical help, and watch for problems. This makes the experience better for patients getting cancer medications and chemotherapy treatment.
Hospital and Cancer Center Policies for Chemo Companions
Hospitals and cancer centers have rules for who can be with patients during chemotherapy. These rules help keep patients safe and comfortable. It’s important for companions to know these rules.
Standard Visitation Guidelines
Most cancer centers have rules for when and how companions can visit. Usually, one or two companions can be with the patient at a time. But, these rules can change based on the center, the patient’s health, and the treatment area.
Some centers let visitors come and go freely, while others have set hours or special waiting areas. Patients and their companions should ask about these rules when they schedule their chemotherapy.
COVID-19 Related Restrictions
The COVID-19 pandemic has added new rules at many healthcare places, including cancer centers. These include mandatory masks, temperature checks, and COVID-19 tests for visitors. Some places might also limit visitors or ask them to wait outside during treatment.
These rules can change often based on local health advice and the pandemic’s progress. Visitors need to be ready to follow these rules to keep everyone safe.
Special Considerations for Immunocompromised Patients
Patients getting chemotherapy often have weak immune systems. This makes them more likely to get sick. So, cancer centers have strict rules to prevent infections, like screening visitors for illness before they can visit.
Visitors are usually told to wash their hands often, avoid touching sick people, and stay home if they’re sick. Following these steps is key to keeping immunocompromised patients safe from infections.
| Policy Aspect | Typical Guidelines | Special Considerations |
| Visitation | One or two companions allowed | May vary based on treatment area |
| COVID-19 Restrictions | Mandatory masking, temperature checks | May include COVID-19 testing |
| Immunocompromised Precautions | Strict infection control measures | Companions advised on hygiene practices |
Preparing to Accompany Someone to Chemotherapy
Going to chemotherapy with someone is more than just being there. You need to know what’s happening and be ready for anything. Your job is to support them emotionally, help with everyday tasks, and sometimes speak up for them.
Essential Items to Bring for Patient Comfort
To make the patient comfortable, bring some key items. These might be:
- A blanket or pillow for physical comfort
- Entertainment like books, tablets, or games
- Snacks and drinks, as treatment centers often have limited options
- Comfortable clothing or a change of clothes in case of spills
What Companions Should Pack
Companions should also pack their own essentials. These can include:
- Snacks and water to keep their energy up
- Entertainment or reading material to pass the time
- A notebook and pen to write down important info or questions for the medical team
- Comfortable clothing and layers for changing temperatures in the treatment area
Being ready helps companions focus on supporting the patient without getting distracted.
Understanding Treatment Duration and Logistics
It’s important to know about chemotherapy treatment. This means understanding how long it takes, which can vary a lot. You also need to know how often and how long each session is.
Also, be aware of possible side effects and how to handle them. This way, you can support the patient better and know when to get help.
Being well-prepared and informed makes you a big help in the patient’s treatment. It makes their experience better and shows you care.
Common Types of Chemotherapy and Administration Methods
It’s important for patients and caregivers to understand the different types of chemotherapy. Each type is tailored to individual needs. Knowing how they are given can help manage side effects and expectations.
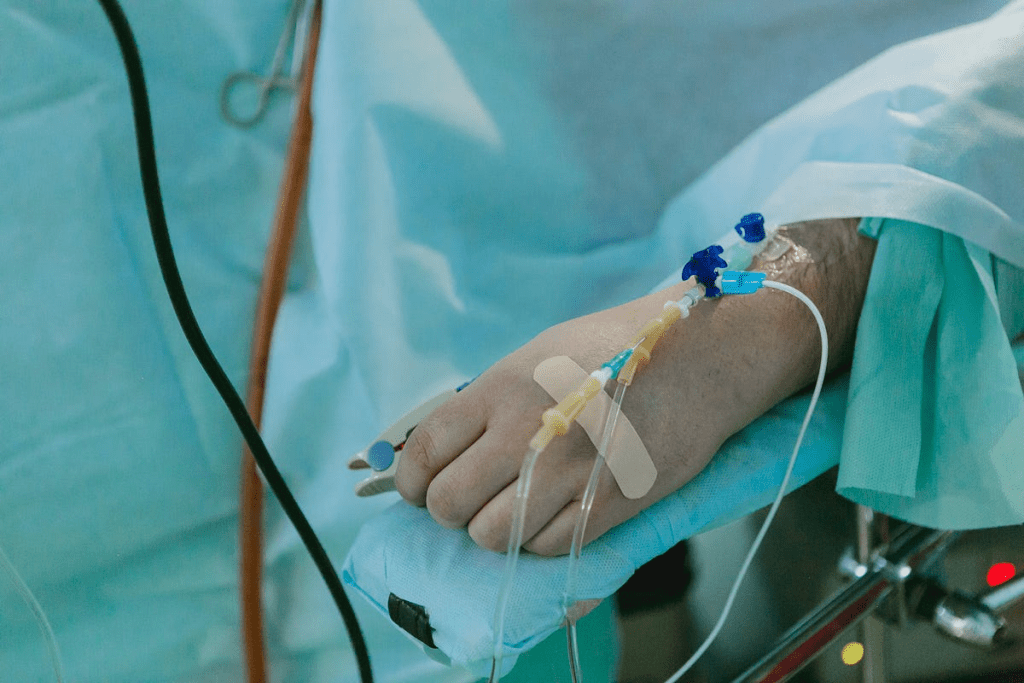
Intravenous Chemotherapy and Infusion Process
Intravenous (IV) chemotherapy is a common method. It delivers drugs directly into a vein. This way, high doses can be given quickly and effectively.
The infusion happens in a hospital or clinic. There, patients are watched for any bad reactions.
Oral Chemotherapy Pills and Compliance
Oral chemotherapy pills are another treatment option. Patients take these drugs in pill or liquid form. It’s key to follow the treatment plan closely.
Missing doses or taking the wrong amount can harm treatment results. Patients must work with their healthcare team to manage side effects and stay on track.
Chemotherapy Ports and Access Devices
Chemotherapy ports are small devices implanted under the skin. They make it easier to get chemotherapy without needing to stick needles in the skin often. They are used for patients needing long-term treatment.
Expected Side Effects During Different Chemotherapy Phases
Chemotherapy side effects change with each treatment phase. It’s key for patients and caregivers to know this. This way, they can better support each other.
Immediate Reactions During Infusion
Right when treatment starts, patients might feel anything from mild discomfort to serious allergic reactions. “I’ve seen patients who react to chemotherapy even before the infusion is complete,” says. She’s seen many side effects during this time.
Common side effects include:
- Nausea and vomiting
- Dizziness or lightheadedness
- Allergic reactions, such as rash or itching
- Infusion site reactions, like redness or swelling
First 24-48 Hours After Treatment
Right after treatment, side effects like fatigue, nausea, and hair loss are common. It’s important to manage these symptoms well. This helps the patient feel better and recover faster.
Days 3-10: Nadir Period Concerns
The nadir period is between days 3-10 after treatment. It’s when blood cell counts are lowest. This makes patients more likely to get infections, anemia, and bleeding.
It’s important to keep an eye on blood counts and watch for signs of these problems.
Long-term Cumulative Effects
Chemotherapy can also have long-term effects. These include chronic fatigue, neuropathy, and damage to organs. Knowing about these effects helps patients and caregivers prepare for the future.
Signs Chemo is Killing You: Recognizing Dangerous Complications
Chemotherapy is a lifesaver for many, but it can also cause serious problems. These complications can happen suddenly and differently for everyone. Knowing the signs can help patients and caregivers act fast when needed.
Life-Threatening Allergic Reactions
Allergic reactions are a big risk with chemotherapy. Symptoms include trouble breathing, a fast heartbeat, and low blood pressure. It’s key to tell healthcare staff right away if you feel anything strange during treatment. Anaphylaxis, a severe reaction, can happen fast.
Severe Organ Toxicity Indicators
Chemotherapy can harm vital organs like the heart, liver, or kidneys. Watch for signs like chest pain, jaundice, or changes in how you pee. Regular blood tests and doctor visits can catch these problems early.
Dangerous Levels of Immunosuppression
Chemotherapy weakens the immune system, making infections more likely. Look out for fever, a persistent cough, or extreme tiredness. It’s important to know these signs and get help right away if you see them.
When Treatment Becomes More Harmful Than Beneficial
Sometimes, the risks of chemotherapy are too high. This might happen if the treatment isn’t working or if side effects are too bad. Healthcare providers need to regularly check if continuing treatment is right.
| Complication | Symptoms to Watch For | Action to Take |
| Allergic Reaction | Difficulty breathing, rapid heartbeat, drop in blood pressure | Report symptoms immediately to healthcare staff |
| Organ Toxicity | Chest pain, jaundice, changes in urination | Inform healthcare provider; undergo regular monitoring |
| Immunosuppression | Fever, persistent cough, severe fatigue | Seek immediate medical attention |
How to Distinguish Between Normal Side Effects and Emergencies
Patients getting chemotherapy must know the difference between usual side effects and serious emergencies. Knowing this is key to keeping safe and getting the best treatment results.
Expected vs. Concerning Symptoms Chart
We’ve made a chart to help patients and caregivers tell normal side effects from emergencies. It lists common side effects and when they might be serious.
| Symptom | Normal Side Effect | Red Flag |
| Nausea | Mild to moderate, manageable with medication | Severe, persistent, or accompanied by vomiting blood |
| Fatigue | Common, improves with rest | Extreme, interferes with daily activities, or is accompanied by dizziness |
| Fever | Low-grade ( | High-grade (≥100.4 °F or 38 °C), specially if persistent or with chills |
| Bleeding or Bruising | Minor bruising | Significant or unexplained bleeding, large bruises, or petechiae |
Red Flag Symptoms Requiring Immediate Attention
Certain symptoms during or after chemotherapy need quick medical help. These red flag symptoms include:
- Severe difficulty breathing or shortness of breath
- Chest pain or tightness
- Severe abdominal pain
- Confusion or altered mental state
- Severe allergic reactions (e.g., hives, swelling, difficulty swallowing)
- High fever or chills
- Uncontrolled bleeding
If you have any of these symptoms, get medical help right away.
Using Vital Signs to Monitor Patient Status
Tracking vital signs is important during and after chemotherapy. Key signs to watch include:
- Temperature
- Pulse
- Blood pressure
- Respiratory rate
- Oxygen saturation
Keeping a log of these signs can spot issues early. For example, a rising temperature might mean infection. A drop in blood pressure could signal dehydration or another problem.
Understanding the difference between normal side effects and emergencies is key. Patients and caregivers can better handle treatment challenges. Always talk to your healthcare team if you’re worried about symptoms or health during chemotherapy.
Chemotherapy Precautions for Family Members and Caregivers
Helping a patient through chemotherapy is more than just being there emotionally. It also means creating a safe space and handling treatment materials carefully. Family and caregivers need to know how to keep the patient safe and comfortable.
Safe Handling of Bodily Fluids After Treatment
After chemotherapy, patients may have drugs in their urine, feces, vomit, and saliva. To avoid exposure, follow these steps:
- Wear gloves when handling bodily fluids or cleaning up after the patient.
- Use a toilet, not a bedpan, and flush the toilet twice after use.
- Wash hands thoroughly with soap and water after any contact with bodily fluids.
- For the first 48 hours after treatment, patients should use condoms during sexual activity.
Home Environment Modifications
Making the home safe is key for patients getting chemotherapy. Here’s what to do:
- Remove tripping hazards to prevent falls.
- Ensure good ventilation to reduce infection risk.
- Keep the environment clean, focusing on areas the patient uses.
- Prepare meals that are easy to eat and digest, as chemotherapy can cause nausea and mouth sores.
Protecting Vulnerable Household Members
Pregnant women, young children, and those with weak immune systems need extra care. Here’s how to protect them:
- Limit contact between the patient and vulnerable household members, specially during the first few days after treatment.
- Keep the patient’s laundry separate and wash it twice before others handle it.
- Avoid sharing personal items, such as utensils, razors, or toothbrushes.
Disposal of Contaminated Materials
It’s important to dispose of materials with chemotherapy drugs or bodily fluids properly. Here’s how:
- Use a designated container for disposing of contaminated materials, such as gloves, gowns, or cleaning supplies.
- Seal the container tightly and label it clearly.
- Check with local waste management for guidelines on disposing of hazardous waste.
By following these precautions, family and caregivers can greatly help patients undergoing chemotherapy. It’s a team effort that needs understanding, patience, and attention to detail.
Supporting Someone Through Chemotherapy Side Effects
Supporting a loved one through chemotherapy means understanding its side effects. Chemotherapy affects people in different ways. Knowing this can help you support them better.
Managing Nausea and Digestive Issues
Nausea and digestive problems are common with chemotherapy. To help, try these tips:
- Encourage eating small, frequent meals to ease digestion
- Keep a food diary to find and avoid foods that upset the stomach
- Use anti-nausea medications as your doctor suggests
Also, look into ginger-based products or natural remedies for nausea. But always check with a healthcare professional first.
Addressing Fatigue and Energy Conservation
Fatigue is a big problem that can really affect a patient’s life. Here’s how you can help:
- Encourage gentle exercise like walking or yoga to increase energy
- Help with daily tasks and errands to save energy
- Support rest and a regular sleep schedule
Using energy-saving strategies can really help manage fatigue.
Coping with Hair Loss and Body Image Changes
Hair loss and body changes can be tough. Here are some ways to cope:
- Look into wigs or headscarves for hair loss
- Encourage talking about body image concerns
- Support skincare routines for skin changes
Sydney Towle’s story shows how important emotional support is during these changes.
Helping with “Chemo Brain” and Cognitive Effects
“Chemo brain” is when patients feel mentally foggy or have memory problems. Here’s how to help:
- Use memory aids like calendars or reminders
- Break tasks into simpler steps to ease mental strain
- Engage in activities that challenge the mind
These tips can help lessen the mental effects of chemotherapy.
Communication Strategies Between Patients, Caregivers, and Medical Teams
Good communication is key when dealing with chemotherapy. It helps everyone involved stay informed and work together. This leads to better care for the patient.
Effective Symptom Reporting
Effective symptom reporting is very important during chemotherapy. Patients should keep a journal of their symptoms. This includes how bad they are, how long they last, and what makes them better or worse.
Caregivers are also important in this process. They can help patients remember to write down their symptoms. They can also add their own observations. This way, the medical team gets a full picture of the patient’s health.
Advocating for the Patient During Treatment
Advocating for the patient is another key part of communication. Family members and caregivers can speak up for the patient. They can ask questions, clarify treatment plans, and share concerns with the medical team.
To be a good advocate, it’s important to know about the patient’s treatment. This includes possible side effects and special needs. Being involved helps avoid misunderstandings and ensures the patient gets the best care.
Maintaining Medical Records and Treatment Journals
Maintaining accurate and complete medical records is vital. Patients should keep track of their treatment, medications, and test results. This helps healthcare providers make better decisions.
A treatment journal is also helpful. It tracks progress, notes changes in symptoms or side effects, and records questions or concerns. Keeping detailed records helps patients and caregivers take an active role in their care.
Self-Care Essentials for Chemo Companions
Being a companion to someone getting chemotherapy means taking care of yourself too. It’s not just about supporting your loved one; it’s also about keeping yourself healthy. This is because caring for someone during this tough time can be hard on both your body and mind.
Managing Caregiver Stress and Burnout
It’s key to manage stress to keep supporting your loved one well. Mindfulness, meditation, and deep breathing can help ease the stress. Knowing the signs of burnout, like feeling tired all the time or getting easily annoyed, is also important.
Take breaks, do things you love, and talk to friends or a counselor. This helps you handle the caregiving job better and keeps you healthy.
Finding Respite Care Options
Respite care gives caregivers a break, letting them rest and take care of themselves. You can find it through in-home care, adult day care, or short stays in care facilities. Finding respite care early can prevent burnout and help you keep supporting your loved one.
Look for respite care that meets your needs and the patient’s. Research local options and talk to healthcare providers to find the best fit.
Support Groups and Resources for Caregivers
Support groups are great for caregivers. They offer a place to share, get emotional support, and learn from others. You can find them at local hospitals, cancer organizations, and online.
There are also many resources to help caregivers. These include educational materials, counseling, and online forums. Exploring these can make caregiving easier and better for you.
| Resource Type | Description | Benefits |
| Support Groups | Meetings or online forums where caregivers share experiences and support one another. | Emotional support, practical advice, sense of community. |
| Respite Care | Temporary care services giving caregivers a break. | Reduces burnout, allows for personal time, improves caregiver well-being. |
| Counseling Services | Professional counseling to address caregiver stress and emotional challenges. | Reduces stress, improves mental health, enhances coping strategies. |
Alternative Support Options When In-Person Accompaniment Isn’t Possible
When you can’t be there in person, there are other ways to help chemotherapy patients. Not having a family member or friend there doesn’t mean they’re alone.
Virtual Support During Treatment
Virtual support is now a key help for those going through chemotherapy. Through video calls and messaging apps, loved ones can stay close and offer support. Virtual accompaniment helps fight off loneliness and anxiety during treatment.
To make the most of virtual support, patients and their caregivers should:
- Make sure they have a stable internet connection
- Use a device with a good camera and microphone
- Find a quiet, private spot for the virtual visit
- Have a backup plan, like a phone number, for tech problems
Professional Chemo Companion Services
For those without a support network, professional chemo companion services are a great option. These services send trained people to be with patients during treatment. They offer emotional support and help with practical tasks.
| Service | Description | Benefits |
| Emotional Support | Trained companions offer emotional comfort and company | Lessens feelings of loneliness and anxiety |
| Practical Assistance | Help with tasks like reading, note-taking, and navigating the treatment facility | Makes patients more comfortable and helps them understand their treatment |
Coordinating Care Teams Among Family and Friends
Even if you can’t be there in person, family and friends can help a lot. They can organize care teams, manage medication, and provide logistical support before, during, and after treatment.
Effective coordination means:
- Creating a shared calendar for treatment schedules and tasks
- Choosing a main contact for medical updates
- Arranging transportation and places to stay for treatment days
- Preparing meals and handling nutrition during treatment
By using these support options, chemotherapy patients can get the care they need, even without in-person help. Whether through virtual support, professional services, or coordinated care, patients can face their treatment journey with less stress and more support.
Conclusion: Balancing Supportive Care with Vigilant Monitoring
Supporting someone through chemotherapy is a delicate task. It requires giving emotional support and watching for signs of trouble. Supportive care is key for patients, helping them deal with treatment’s physical and emotional toll.
It’s also vital to watch closely for signs that chemo might be harming the patient. This includes severe side effects or allergic reactions. Knowing about chemotherapy’s side effects and red flags helps caregivers offer better support and get help when it’s needed.
By balancing supportive care with careful monitoring, caregivers can greatly improve the patient’s experience. Understanding the risks and benefits of chemotherapy lets caregivers support patients with confidence and care.
FAQ
Can I accompany someone during their chemotherapy session?
Yes, it’s good to have someone with you during chemotherapy. They can offer emotional support and watch for any bad reactions.
What are the benefits of having a companion during chemotherapy?
A companion can give emotional support and help with daily needs. They also watch for side effects, making the treatment easier for you.
Are there any restrictions on companions during chemotherapy?
Yes, rules can change, like during the COVID-19 pandemic. Some places might limit visitors to keep everyone safe.
How can I prepare to accompany someone to chemotherapy?
Bring things to make them comfortable, like snacks and games. Knowing how long the treatment will take helps too.
What are the different types of chemotherapy administration methods?
Chemotherapy can be given through an IV, as pills, or through special devices. Each method has its own effects and side effects.
What are the expected side effects during different phases of chemotherapy?
Side effects change over time. You might feel bad right away, then better, and then worse again. Long-term effects can also happen.
How can I tell if chemotherapy is causing dangerous complications?
Look out for signs like severe allergic reactions, organ damage, or when treatment starts to harm more than help.
What are the red flag symptoms that require immediate attention during chemotherapy?
Watch for signs like severe pain, trouble breathing, or unusual bleeding. Also, look out for infection signs and severe nausea.
How should family members and caregivers handle bodily fluids after chemotherapy?
Be careful with fluids that might have chemotherapy drugs. Use gloves and follow safe disposal rules to avoid exposure.
How can we support someone through chemotherapy side effects like nausea and fatigue?
For nausea, try changing what you eat and use medicine. For fatigue, rest when you need to and keep a healthy lifestyle.
What are some strategies for effective communication between patients, caregivers, and medical teams?
Report symptoms well, speak up for the patient, and keep detailed medical records. This helps everyone work together better.
How can caregivers manage their own stress and burnout while supporting a loved one through chemotherapy?
Take breaks, join support groups, and take care of yourself. This helps you avoid getting too stressed or burned out.
Are there alternative support options when in-person accompaniment isn’t possible?
Yes, you can use virtual support, hire professional caregivers, or ask friends and family to help. This way, you can get the support you need even when you can’t be there in person.
What precautions should be taken when caring for a patient undergoing chemotherapy at home?
Make your home safer by reducing infection risks. Protect others in your home and dispose of contaminated items safely. This keeps everyone safe while caring for the patient at home.
References
Hazelwood, D. M., et al. (2012). Patients with cancer and family caregivers: management of symptoms and psychosocial adaptation over time. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC3767444/