Last Updated on December 1, 2025 by Bilal Hasdemir
Skull base surgery is a complex and delicate procedure. It needs precision and expertise. The surgery’s length can vary a lot based on several factors. Get the shocking facts on skull base osteomyelitis cureSkull Cancer: Causes, Symptoms & Treatment. Learn the critical factors that make this complex operation surprisingly long.
Did you know the surgery’s length depends on the case’s complexity and the surgical approach? Advanced surgical techniques and experienced surgeons are key to success and the operation’s length.
Treating conditions like osteomyelitis through skull base surgery requires careful planning. It’s important for patients and medical professionals to understand what affects the surgery’s duration.
Key Takeaways
- The duration of skull base surgery varies based on the complexity of the case.
- The surgical approach used significantly influences the length of the surgery.
- Osteomyelitis treatment through surgery requires precise planning.
- Advanced surgical techniques and experienced surgeons are critical.
- Understanding the factors influencing surgery duration is essential for patients.
Understanding Skull Base Osteomyelitis
The skull base is a complex area at the bottom of the skull. It can get infected, leading to a serious condition called osteomyelitis. This infection can cause inflammation in the bone and lead to severe problems.
Definition and Anatomy of the Skull Base
The skull base is the floor of the skull, made up of several bones. It houses important structures like blood vessels, nerves, and the brainstem. Knowing about this area is key to treating skull base infection.
Causes and Risk Factors of Skull Base Infections
Osteomyelitis at the skull base usually comes from bacteria or fungi. People with diabetes, weakened immune systems, or past head and neck infections are at higher risk. Spotting these risk factors early is vital for treating cranial osteomyelitis effectively.
Common Symptoms and Diagnostic Methods
Symptoms of skull base osteomyelitis include severe headaches, fever, and neurological problems. Osteomyelitis symptoms can also be pain and feeling unwell. Diagnostic methods like MRI and CT scans help find the infection’s extent and plan treatment.
Managing skull base osteomyelitis well needs a detailed plan. This includes using the right diagnostic methods and starting cranial osteomyelitis treatment quickly. Understanding the causes, symptoms, and how to diagnose helps doctors treat patients better.
The Skull Base Osteomyelitis Cure: Comprehensive Treatment Approaches

Treating skull base osteomyelitis requires different strategies. These range from non-surgical methods to surgery, based on how severe the condition is. Each treatment plan is made to fit the patient’s health, the infection’s spread, and the type of bacteria involved.
Conservative Management Options
For most cases, starting with non-surgical treatments is best. This mainly includes using antibiotics to fight the infection. Choosing the right antibiotic is key, based on lab tests to target the bacteria effectively. Along with antibiotics, managing pain and keeping an eye on the patient’s health are also important.
| Treatment Component | Description | Importance |
| Antibiotics | Targeted therapy based on culture and sensitivity | High |
| Pain Management | Use of analgesics to control pain | Medium |
| Monitoring | Regular assessment of infection and response to treatment | High |
When Surgical Intervention Becomes Necessary
If non-surgical treatments don’t work or the infection is very bad, surgery might be needed. Surgery aims to remove infected tissue, drain abscesses, and fix any skull base damage. The choice to have surgery depends on weighing the risks and benefits for each patient.
Multidisciplinary Treatment Teams
Using a multidisciplinary team approach helps a lot in treating skull base osteomyelitis. This team includes experts like infectious disease doctors, neurosurgeons, ear, nose, and throat specialists, and radiologists. Working together, they provide complete care from start to finish, improving patient results.
Duration of Skull Base Surgery: Timeframes and Variables
Knowing how long skull base surgery takes is key for getting ready and recovering. The time needed for surgery changes a lot. This depends on how complex the case is, the surgical method, and the patient’s health.
Factors Affecting Surgical Duration
The type of skull base issue being treated greatly affects surgery time. Cases with tumors or big infections take longer. Also, the surgeon’s skill and the techniques used play a role.
Key factors affecting surgical duration include:
- The extent of the disease or condition
- The chosen surgical approach (endoscopic, open, or minimally invasive)
- The patient’s anatomical characteristics
- The presence of any complications or unexpected findings during surgery
Average Timeframes for Different Surgical Approaches
Each surgical method has its own average time. For example, endoscopic procedures are usually quicker than open craniotomies. Endoscopic surgeries can last from 2 to 6 hours. Open surgeries can take 4 to 12 hours or more, depending on the complexity.
| Surgical Approach | Average Duration |
| Endoscopic Endonasal | 2-6 hours |
| Open Craniotomy | 4-12 hours |
| Minimally Invasive | 3-8 hours |
Anesthesia and Immediate Post-Operative Monitoring
Anesthesia is very important in skull base surgery. The type and amount used must ensure safety and comfort. After surgery, patients are closely watched in an ICU. This is to handle any immediate issues.
The length of skull base surgery is a big part of the treatment plan. It affects how patients prepare and recover. Knowing what affects surgery time helps doctors better care for their patients.
Preparation for Skull Base Surgery
Getting ready for skull base surgery is a detailed process. It aims to ensure the best results. This includes preoperative tests, managing medications, and educating patients.
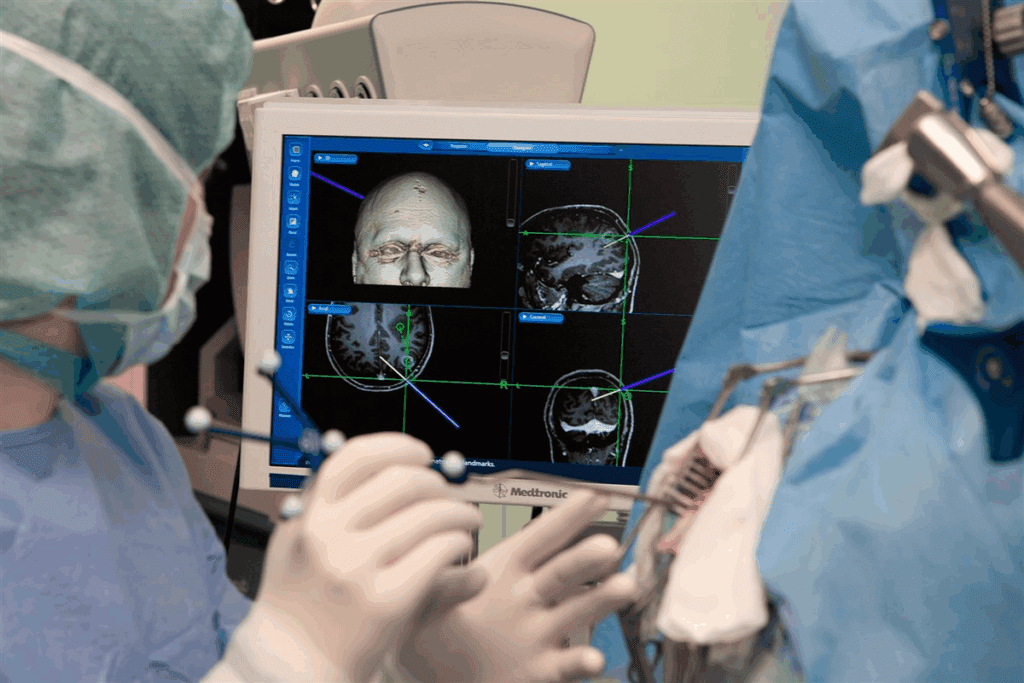
Preoperative Testing and Evaluation
Preoperative testing is key. It involves imaging like MRI and CT scans, blood work, and more. These tests check the patient’s health and the bone infection’s extent.
Medication Management Before Surgery
Managing medications is also important. Patients might need to change or stop some drugs. This is to avoid problems during surgery or healing.
Patient Education and Expectations
Teaching patients is vital. They need to know what to expect before, during, and after surgery. This includes the surgery itself, risks, and recovery time. Well-informed patients can follow instructions better and recover well.
Surgical Approaches and Techniques for Skull Base Infections
Skull base infections need careful surgery. This can include endoscopic methods or craniotomies. The right surgery depends on the infection’s size and where it is, and the patient’s health.
Endoscopic Endonasal Approaches
Endoscopic endonasal surgery is now common for skull base infections. These minimally invasive techniques use the nose to reach the infection. This can mean less scarring and quicker healing.
Open and Minimally Invasive Craniotomy Techniques
For bigger or harder-to-reach infections, craniotomy is used. This involves opening the skull to get to the infection. It lets surgeons clean and drain the area well.
Surgical Debridement for Osteomyelitis Treatment
Debridement is key in treating osteomyelitis. It removes infected bone and tissue. This stops the infection from spreading and helps the bone heal. How much is removed depends on the osteomyelitis’s severity.
| Surgical Approach | Indications | Benefits |
| Endoscopic Endonasal | Localized infections accessible through nasal passages | Minimally invasive, less recovery time |
| Open Craniotomy | Extensive infections or those not accessible endonasally | Direct access to infected area, thorough debridement possible |
| Minimally Invasive Craniotomy | Selected cases between endonasal and open craniotomy | Balances invasiveness with need for direct access |
Antibiotic Therapy in Skull Base Osteomyelitis Management
Understanding antibiotic therapy is key to managing skull base osteomyelitis. Antibiotics are vital in controlling the infection and preventing complications.
Intravenous Antibiotics: Types, Duration, and Administration
Intravenous antibiotics are often the first choice for treating skull base osteomyelitis. They quickly reach high levels in tissues. Common ones include piperacillin-tazobactam, ceftazidime, and meropenem.
The treatment lasts from 4 to 6 weeks, depending on the infection’s severity and the patient’s response.
Administering intravenous antibiotics requires close monitoring. This ensures they work well and don’t cause harm. Doctors check kidney function, liver enzymes, and blood counts regularly.
Transitioning to Oral Antibiotics
When the patient starts to get better, switching to oral antibiotics might happen. Oral antibiotics like ciprofloxacin or amoxicillin-clavulanate are used. The decision to switch depends on the patient’s health, the infection’s extent, and the bacteria involved.
Managing Antibiotic Resistance in Chronic Cases
Dealing with antibiotic resistance in chronic cases is tough. To tackle this, doctors use broad-spectrum antibiotics and combination therapy. They also work with infectious disease specialists.
It’s important to keep a close eye on how the infection responds to treatment. Adjusting the antibiotic plan as needed is critical.
Adjunctive Treatments for Skull Base Osteomyelitis
Adjunctive treatments are key in treating skull base osteomyelitis. They work alongside main treatments to improve patient results and lower the chance of problems.
Hyperbaric Oxygen Therapy Benefits and Protocol
Hyperbaric oxygen therapy (HBOT) is a helpful treatment for skull base osteomyelitis. It boosts oxygen to infected areas, helping them heal and lessening infection severity. The usual treatment includes 20-40 sessions, each lasting 60-90 minutes at 2-3 atmospheres pressure.
HBOT offers several benefits:
- It helps wounds heal faster
- It lowers bacterial counts
- It improves tissue oxygen levels
Management of Necrotizing Otitis Externa and Ear Infections
Necrotizing otitis externa is a serious issue from skull base osteomyelitis. It needs quick and effective treatment. This includes aggressive antibiotic therapy and surgical debridement to fight the infection and stop tissue damage.
| Treatment Approach | Description |
| Antibiotic Therapy | Initial empirical treatment followed by culture-directed therapy |
| Surgical Debridement | Removal of necrotic tissue to prevent spread of infection |
Specialized Approaches for Fungal Skull Base Osteomyelitis
Fungal osteomyelitis of the skull base is tough to treat. It needs antifungal therapy and sometimes surgical intervention. Voriconazole is often chosen because it works well in the central nervous system.
Effective management includes:
- Quick diagnosis through culture and histopathology
- Starting the right antifungal treatment
- Watching for treatment success and side effects
Recovery and Rehabilitation After Skull Base Surgery
Recovering from skull base surgery is a detailed process. It needs careful care and rehabilitation after surgery. The surgery’s complexity means a thorough approach is needed for the best healing and outcomes.
Hospital Stay and Immediate Post-Operative Care
Right after surgery, patients stay in the hospital. Medical teams watch them closely. “The first days after surgery are key to spotting and fixing any issues,” says a top neurosurgeon.
Patients get help with pain, antibiotics, and more. These treatments help them recover smoothly.
Osteomyelitis Healing Process and Timeline
Osteomyelitis, a bone infection, needs long treatment. The healing mix includes antibiotics and sometimes surgery. Recovery time for osteomyelitis can be months.
Following the treatment plan is key for the best results.
Physical and Occupational Therapy During Recovery
Physical and occupational therapy are key in recovery. They help patients get stronger, balance better, and adjust to surgery changes. A custom rehab plan, led by skilled therapists, boosts recovery and long-term success.
Knowing about recovery and rehab helps patients face skull base surgery challenges. With the right care and support, people can see big improvements in their health and life quality.
Conclusion: Long-Term Outcomes and Future Directions
Understanding how to manage skull base osteomyelitis long-term is key to better patient care. Treatments like surgery and antibiotics have shown good results. They help in curing skull base osteomyelitis.
But, the chance of getting the infection again is a big worry. This shows we need to keep watching and managing patients closely. New surgical methods, like endoscopic endonasal approaches, have made things better for patients with abscesses.
Looking ahead, we might see new antibiotics and more treatments like hyperbaric oxygen therapy. These could make treatments even better.
By working to make treatments better and care more effective, we can help people with this complex condition more. Healthcare providers are on the path to better outcomes for those affected.
FAQ
What is skull base osteomyelitis?
Skull base osteomyelitis is a serious bone infection at the skull’s base. It’s usually caused by bacteria or fungi. If not treated, it can be very dangerous.
How is skull base osteomyelitis diagnosed?
Doctors use MRI or CT scans and blood tests to diagnose it. They also look at your medical history and do a physical check-up.
What are the treatment options for skull base osteomyelitis?
Treatment can include antibiotics, surgery, or hyperbaric oxygen therapy. The best option depends on the infection’s severity and your health.
How long does skull base surgery take?
Surgery time varies. It depends on the surgery’s complexity, the approach, and your health. It can last from a few hours to several hours.
What is the role of antibiotic therapy in managing skull base osteomyelitis?
Antibiotics are key in treatment. You might start with IV antibiotics and then switch to oral ones. Fighting antibiotic resistance is also important.
What is hyperbaric oxygen therapy, and how is it used in treating skull base osteomyelitis?
Hyperbaric oxygen therapy uses pure oxygen in a pressurized chamber. It helps heal and fight infection. It’s used when other treatments don’t work well.
How long does it take to recover from skull base surgery?
Recovery time varies depending on the surgery, your health, and any complications. Hospital stay can last from a few days to several weeks, followed by weeks to months of rehabilitation.
What are the long-term outcomes for patients with skull base osteomyelitis?
Outcomes vary. They depend on treatment success, your health, and following care instructions. With good management, many patients see big improvements or full recovery.
Can skull base osteomyelitis recur?
Yes, it can come back. This is often due to not treating the cause fully or inadequate treatment. Regular check-ups and care are key to prevent it.
What are the possible complications of skull base surgery?
Complications can include infection, bleeding, and damage to nearby structures. The risk depends on the surgery’s complexity and your health.
How is necrotizing otitis externa managed?
This severe ear infection is treated with strong antibiotics and sometimes surgery. Quick treatment is vital to avoid serious problems like skull base osteomyelitis.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/39332030/