Last Updated on December 1, 2025 by Bilal Hasdemir
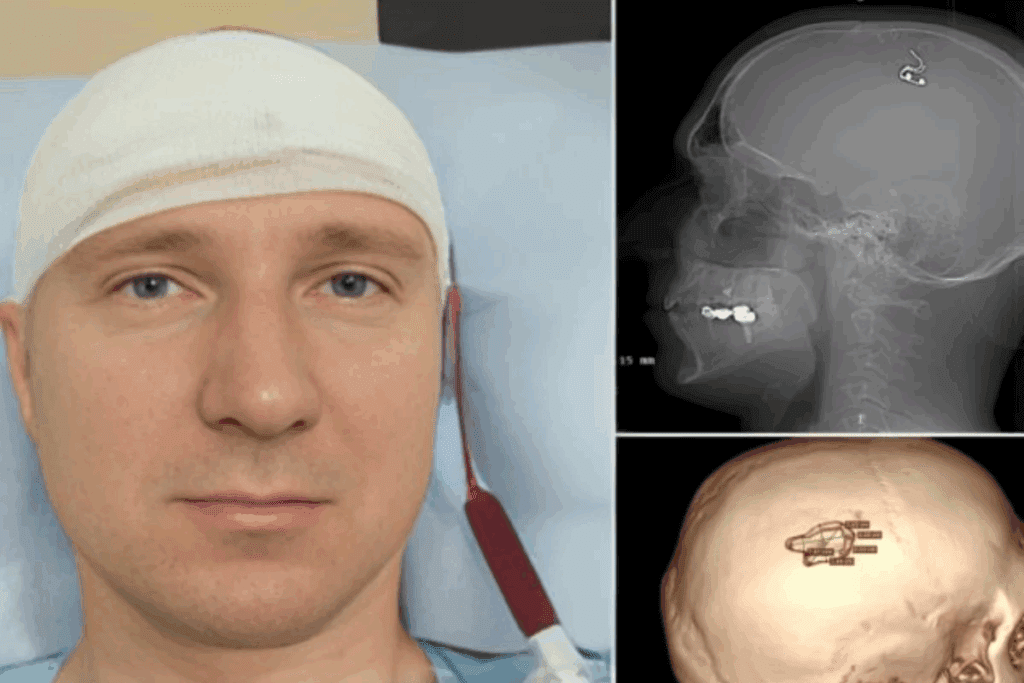
Skull base surgery is a complex procedure involving delicate operations at the base of the skull, where critical nerves and blood vessels are located.. A significant concern with this type of surgery is the risk of complications, which can have a profound impact on patient outcomes. Discover the awful skull base surgery complications. Our essential guide reveals the critical risks, from CSF leaks to nerve damage.
Operating on the skull base is challenging. This is because of the presence of critical structures like cranial nerves and major blood vessels. The complexity of this region makes it prone to various complications, including damage to these vital structures.
Understanding the risks and complications of skull base surgery is key. This knowledge helps both medical professionals and patients. It aids in making informed decisions and preparing for the possible outcomes of such a complex procedure.
Key Takeaways
- Skull base surgery is a complex procedure with significant risks.
- Complications can arise due to the delicate nature of the structures involved.
- Cranial nerve damage is a possible complication.
- Understanding the risks is vital for informed decision-making.
- Potential outcomes vary based on the surgery’s complexity.
Understanding Skull Base Surgery
Skull base surgery involves different surgical methods for various needs. It’s a complex field that needs a deep understanding of the skull base’s anatomy.

Definition and Anatomical Considerations
Skull base surgery targets the base of the skull’s complex structures. This area is home to important neurovascular structures, making surgery here very challenging.
“The skull base’s anatomy is very complex,” experts say. “It requires a team effort for planning and doing surgery.”
Common Types of Skull Base Procedures
Skull base surgeries are mainly divided into two types: endoscopic and open surgery. The choice depends on the problem, its location, and the patient’s health.
Endoscopic Approaches
Endoscopic skull base surgery uses an endoscope for a clear view. It’s less invasive, leading to less recovery time and less pain after surgery. It’s great for reaching hard-to-get areas of the skull base.
Open surgery, by contrast, involves making an incision for direct access. It’s more invasive but needed for complex or large problems.
Today, the choice between endoscopic and open surgery depends on the case. The aim is to get the best results for each patient.
Skull Base Surgery Complications: An Overview
Skull base surgery complications can greatly affect patient outcomes. These issues can stem from the surgery’s complexity and the patient’s health.
Incidence and Prevalence
Complications after skull base surgery are a big worry. Data shows that “The overall complication rate of endoscopic endonasal approaches is often quoted to be between 10 and 20%.”
This range shows a big variation in complication risk. It stresses the importance of choosing the right patient and planning carefully before surgery.
Risk Factors for Complications
Several factors can raise the risk of complications during and after skull base surgery. These include:
- Patient Health: Existing medical conditions can increase the risk of complications.
- Surgical Complexity: The procedure’s complexity and location can affect the risk.
- Surgeon Experience: The skill and experience of the surgical team are key in reducing complications.
Classification of Adverse Events
Adverse events from skull base surgery can be grouped into several types. These include neurological, infectious, and vascular complications.
| Category | Description | Examples |
| Neurological | Complications affecting the nervous system | Cranial nerve damage, stroke |
| Infectious | Infections occurring as a result of the surgery | Meningitis, wound infections |
| Vascular | Complications related to blood vessels | Hemorrhage, thrombosis |
Knowing these categories is key to preventing and managing complications effectively.
Neurological Complications
Skull base surgery can lead to neurological problems after the operation. These issues can greatly affect a patient’s life quality. They need careful management.
Cranial Nerve Damage
Cranial nerve damage is a risk in skull base surgery. The nerves around the skull base are very delicate. This makes nerve damage a big concern.
Common Affected Nerves
The nerves most at risk include the olfactory, optic, and facial nerves. Damage to these nerves can cause various symptoms.
- Olfactory nerve damage can lead to loss of smell.
- Optic nerve damage can cause visual disturbances or loss.
- Facial nerve damage can result in facial paralysis or weakness.
Clinical Manifestations
The symptoms of cranial nerve damage vary. They can include numbness, weakness, or paralysis of facial muscles. Difficulty swallowing or changes in vision or hearing are also possible.
| Cranial Nerve | Function | Potential Complication |
| I (Olfactory) | Smell | Loss of smell |
| II (Optic) | Vision | Visual loss or disturbance |
| VII (Facial) | Facial movement | Facial paralysis or weakness |
Stroke and Ischemic Events
Stroke and ischemic events are serious complications after skull base surgery. These often happen due to vascular injury during the procedure.
Risk factors for stroke include pre-existing vascular disease, the complexity of the surgery, and the patient’s health.
Seizures and Neurological Deficits
Seizures can happen due to neurological damage during skull base surgery. Other neurological deficits, like cognitive impairment or motor weakness, can also occur.
Prompt diagnosis and treatment are key to managing these complications effectively.
Cerebrospinal Fluid (CSF) Leaks and Related Issues
CSF leaks are a serious problem after skull base surgeries. They happen when cerebrospinal fluid leaks out through a hole in the dura mater. This can lead to serious issues if not treated right.
Pathophysiology and Risk Factors
CSF leaks happen when the barrier between the subarachnoid space and the body’s structures is broken. Several things can make a person more likely to get a CSF leak. These include how complex the surgery is, if they’ve had radiation therapy, and if they have certain body shapes.
Key risk factors for CSF leaks:
- Surgical complexity and extent of tissue disruption
- History of radiation therapy to the skull base
- Presence of anatomical abnormalities or defects
- Increased intracranial pressure
Diagnosis and Detection Methods
Figuring out if someone has a CSF leak takes both doctor checks and tests. Signs might be CSF coming out through the nose or ear, headaches, or meningitis.
Diagnostic methods include:
| Diagnostic Method | Description |
| Beta-2 transferrin testing | A biochemical test to detect the presence of CSF in nasal or ear secretions |
| Imaging studies (MRI, CT) | To identify the site of the leak and assess for associated complications |
| Intrathecal fluorescein injection | A technique used to visualize the leak during surgery or endoscopy |
Management and Repair Techniques
Handling CSF leaks can be done in a few ways. Sometimes, just resting and avoiding straining can help. Other times, doctors might use a special drainage method to lower pressure inside the brain.
Surgical repair techniques:
- Endoscopic endonasal repair for leaks located in the anterior skull base
- Transmastoid or middle fossa approaches for leaks in the temporal bone
- Use of graft materials (fat, fascia, or synthetic grafts) to close the defect
Fixing CSF leaks needs a team effort. Doctors from different fields work together to make sure the treatment works well.
Infectious Complications
Skull base surgery comes with risks of infections. These risks are important for both surgeons and patients. The surgery’s complex nature can lead to infections that make recovery harder.
Meningitis and Intracranial Infections
Meningitis is a serious issue after skull base surgery. It happens when bacteria get into the brain’s protective membranes. Prompt diagnosis and treatment are key to avoid brain damage.
Symptoms of meningitis include fever, headache, and a stiff neck. Other intracranial infections can cause abscesses or encephalitis. It’s important to catch these early to manage them well.
Wound Infections and Healing Issues
Wound infections are a big worry after skull base surgery. They can slow healing, cause more problems, and keep patients in the hospital longer. Things like contamination during surgery and diabetes can increase these risks.
Good wound care and watching for signs of infection are key. This includes using antibiotics and keeping the surgical site clean.
Sinusitis and Respiratory Complications
Sinusitis can happen when skull base surgery messes with sinus drainage. This can lead to breathing problems and infections spreading.
Dealing with sinusitis means making sure sinuses drain right. Sometimes, antibiotics are needed. Watching for sinusitis signs is important after surgery.
In summary, infections after skull base surgery are complex and need careful management. Knowing the risks and taking steps to prevent them can help patients recover better.
Sensory and Functional Complications
Skull base surgery can lead to various sensory and functional issues. These problems can greatly affect a patient’s quality of life after surgery.
Vision Loss and Visual Disturbances
Vision problems are common after skull base surgery. Damage to the optic nerve or nearby structures can cause vision loss. A study found that vision issues can greatly impact a patient’s life after surgery.
These vision problems can range from double vision to complete loss of sight. Managing these issues often requires a team of experts, including eye doctors and rehabilitation specialists.
Hearing Loss and Balance Problems
Hearing loss and balance issues are common after skull base surgery. The inner ear’s delicate structures are at risk during these surgeries. Hearing loss can be conductive, sensorineural, or mixed, depending on the damage.
- Conductive hearing loss is often related to middle ear damage.
- Sensorineural hearing loss involves damage to the inner ear or auditory nerve.
Balance problems can occur from damage to the vestibular system. Therapy can help manage these issues.
Facial Paralysis and Nerve Dysfunction
Facial paralysis is a major concern in skull base surgery, when the facial nerve is involved. The risk of facial nerve damage depends on the tumor’s location and the surgical method.
“The preservation of facial nerve function is a critical aspect of skull base surgery, as it significantly impacts patient quality of life.”
— Expert Opinion
Nerve dysfunction can also affect other cranial nerves. This can lead to symptoms like swallowing difficulties or speech changes.
Speech and Swallowing Difficulties
Damage to cranial nerves can cause speech and swallowing problems. Swallowing difficulties, or dysphagia, can lead to nutritional deficiencies and aspiration pneumonia.
Speech therapy and swallowing rehabilitation are key in managing these issues. A team of speech-language pathologists is essential for the best patient care.
Vascular and Systemic Complications
Skull base surgery is complex and can lead to various complications. These issues can affect patient outcomes. It’s important for healthcare providers to know the risks, symptoms, and how to manage them.
Intracranial Bleeding and Hematomas
Intracranial bleeding and hematomas are serious issues after skull base surgery. Intracranial hemorrhage can happen if blood vessels are damaged or if there’s poor hemostasis. The risk depends on the surgery’s complexity, the patient’s health before surgery, and any vascular problems.
Symptoms include headaches, confusion, and neurological problems. It’s key to use CT scans for quick diagnosis and treatment.
Blood Clots and Thromboembolism
Blood clots and thromboembolism are major vascular complications. Deep vein thrombosis (DVT) and pulmonary embolism are risks, mainly for those who can’t move much after surgery. Using anticoagulation therapy and mechanical devices can help prevent these.
It’s important to spot blood clot signs like swollen limbs or sudden breathlessness early for treatment.
Anesthesia-Related Complications
Anesthesia-related issues can happen during skull base surgery. These include allergic reactions, breathing problems, or heart issues. Careful preoperative assessment and monitoring during surgery are key to avoid these problems.
Anesthesiologists are vital in managing these risks. They create personalized anesthesia plans and watch patients closely during surgery.
In summary, managing vascular and systemic complications from skull base surgery is critical. Knowing the risks and taking preventive steps can lessen their impact.
Prevention and Management of Complications
Preventing and managing complications in skull base surgery is complex. It requires a variety of strategies to lower risks and improve patient results.
Preoperative Planning and Risk Assessment
Preoperative planning and risk assessment are key to avoiding complications. They involve a detailed look at the patient’s health history, imaging, and other important factors to spot risks.
- Detailed medical history to identify comorbidities and previous surgeries.
- Advanced imaging techniques such as MRI and CT scans to understand the anatomy and pathology.
- Risk assessment tools to predict possible complications.
Intraoperative Monitoring Techniques
Intraoperative monitoring is vital for managing issues during surgery. It helps catch problems early, allowing for quick action.
Key intraoperative monitoring techniques include:
- Electrophysiological monitoring to check nerve function.
- Intraoperative imaging to update the surgical plan as needed.
- Anesthesia monitoring to handle anesthesia-related issues.
Postoperative Care and Surveillance
Postoperative care is critical for managing complications after surgery. It involves watching the patient closely and acting fast if problems arise.
Effective postoperative care involves:
- Monitoring in an intensive care unit (ICU) for high-risk patients.
- Regular check-ups of the neurological status.
- Quick action on any complications that come up.
Rehabilitation Strategies
Rehabilitation is vital for the best results after skull base surgery. It helps patients regain lost functions and improve their quality of life.
Rehabilitation may include:
- Physical therapy to regain strength and mobility.
- Speech therapy for patients with speech or swallowing issues.
- Cognitive rehabilitation for those with cognitive problems.
By using these strategies, healthcare providers can greatly improve patient outcomes and lower the risk of complications from skull base surgery.
Conclusion
Skull base surgery is a complex and delicate procedure. It requires a deep understanding of the possible complications. These can include neurological issues, cerebrospinal fluid leaks, infections, sensory problems, and vascular issues.
It’s vital to know about these complications to give patients the best care. Recent studies show that recognizing these issues is key to managing and preventing them.
Preoperative planning, intraoperative monitoring, and postoperative care are all critical. They help reduce the risk of complications. By understanding and addressing these risks, healthcare professionals can improve patient outcomes. This ensures the best results from skull base surgery.
FAQ
What are the most common complications of skull base surgery?
Skull base surgery can lead to several complications. These include damage to nerves, stroke, and seizures. It can also cause infections like meningitis and wound infections.
What is the risk of cranial nerve damage during skull base surgery?
The risk of nerve damage varies with the surgery type and nerves involved. It’s a big concern because of the nerves’ delicate nature in the skull base.
How is a CSF leak diagnosed and treated?
Doctors use MRI or CT scans and clinical checks to find a CSF leak. To fix it, they might use surgery, either endoscopic or open.
What are the risk factors for developing meningitis after skull base surgery?
Meningitis risk after surgery includes a CSF leak, contaminated sites, and existing infections.
Can vision loss occur as a result of skull base surgery?
Yes, vision loss is a possible complication. It’s more likely if the surgery is near the optic nerve or other key visual areas.
How can intracranial bleeding be prevented during skull base surgery?
To avoid bleeding, surgeons plan carefully, use precise techniques, and monitor closely during surgery.
What are the possible long-term effects of skull base surgery on cognitive function?
Long-term effects on thinking vary by surgery and health. They might include memory or attention changes.
How can patients minimize the risk of complications after skull base surgery?
Follow post-op instructions, go to follow-ups, and tell your doctor about any issues or symptoms.
What is the role of rehabilitation in recovering from skull base surgery?
Rehabilitation is key for recovery. It helps regain function, manage symptoms, and adjust to changes.
Are there any specific risks associated with endoscopic skull base surgery?
Endoscopic surgery risks include CSF leaks, infections, and bleeding. These risks are similar to open surgery.
How can anesthesia-related complications be minimized during skull base surgery?
Minimize anesthesia risks with thorough pre-op checks, close monitoring, and precise anesthesia management.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7759428/