Last Updated on December 1, 2025 by Bilal Hasdemir
The cranial base is a complex area. It houses important structures like nerves, blood vessels, and the brain. A team of skilled surgeons and medical professionals is needed to operate here.
Skull base surgery is a detailed procedure. It involves careful navigation through crowded and complex areas. This surgery is key for treating tumors, aneurysms, and other issues that affect the base of the skull.
Key Takeaways
- The cranial base is a complex area with vital structures.
- Skull base surgery requires a multidisciplinary team.
- The procedure is critical for treating various conditions.
- It involves navigating through intricately complex anatomical areas.
- Skull base surgery can significantly impact patient outcomes.
Understanding Skull Base Surgery
Skull base surgery is a complex procedure. It requires a deep understanding of the anatomy of the skull base. This surgery treats conditions at the base of the skull, where important structures are located.
Definition and Purpose
Skull base surgery includes many procedures. It treats tumors, vascular issues, and injuries. The main goal is to fix or remove damaged tissue without harming nearby areas.
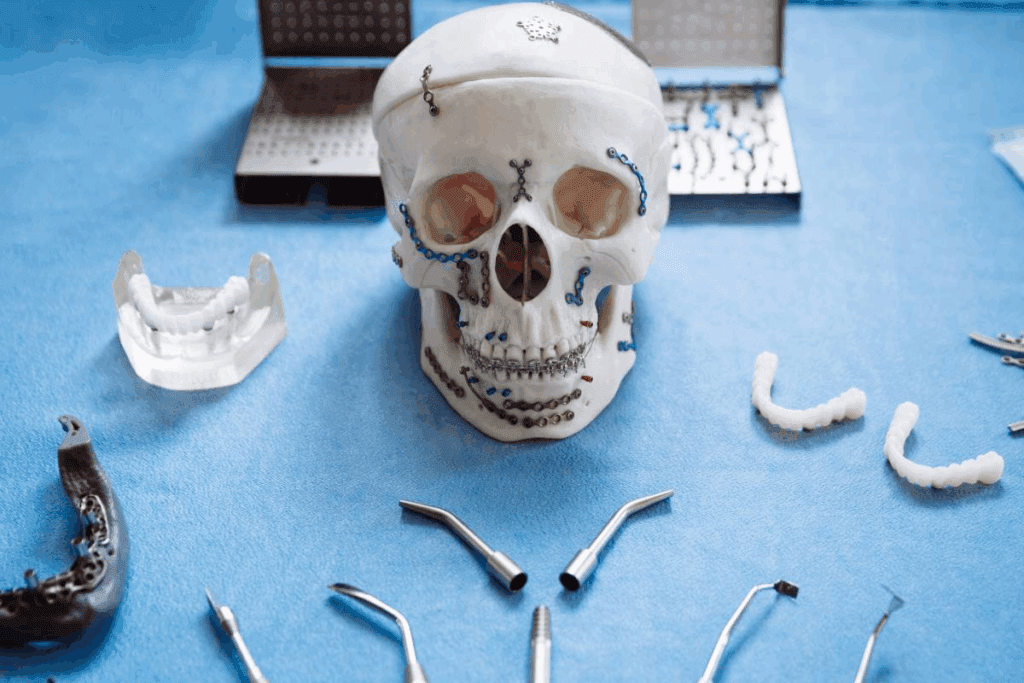
Anatomy of the Skull Base
The skull base anatomy is complex. It includes several bones at the skull’s floor. The cranial base bones are the sphenoid, temporal, and occipital bones. They allow nerves and blood vessels to pass through.
Critical Structures and Regions
The skull base has many critical structures. These include:
- Cranial nerves
- Major blood vessels
- The brainstem
These structures are closely packed, making surgery hard.
Surgical Challenges
Surgeons face many challenges in skull base surgery. These include:
- Navigating complex anatomy
- Preserving critical structures
- Managing possible complications
Indications for Skull Base Surgery
Skull base surgery is needed for many reasons. These include tumors, vascular problems, and injuries from trauma. These issues can really affect a person’s life, making it important to treat them quickly and well.
Tumors and Growths
Skull base surgery helps remove skull base tumors and growths. These can be harmless or cancerous. Symptoms include headaches, vision issues, and trouble swallowing. Taking them out surgically is usually the best way to treat them.
Vascular Abnormalities
Vascular abnormalities like aneurysms and arteriovenous malformations are also treated with skull base surgery. If not treated, they can be very dangerous. Surgery can help avoid serious problems and improve health outcomes.
Traumatic Injuries
Traumatic brain injuries sometimes need cranial base surgery. These injuries can badly damage the skull base and nearby areas. Quick surgery is often needed to stop further harm and help healing.
Pre-Surgical Evaluation and Planning
Skull base surgery needs careful planning before the surgery. This step is key to picking the right surgery and lowering risks.
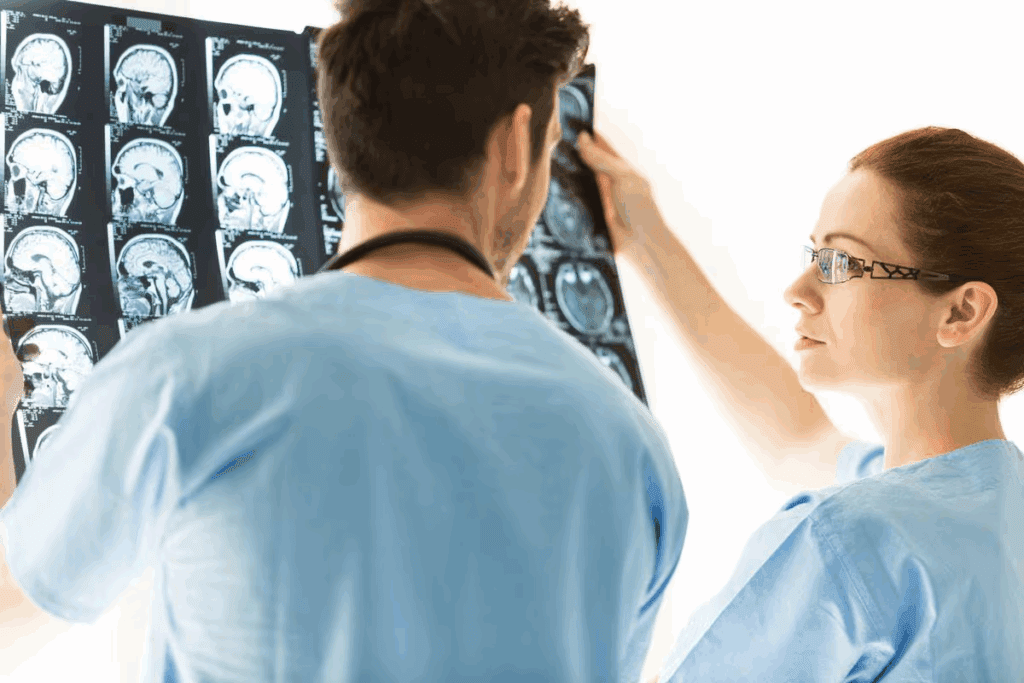
Diagnostic Imaging
MRI and CT scans are key in planning. They give clear pictures of the skull base. This helps surgeons understand the area and find any problems.
Patient Assessment
A full patient assessment is done to check the patient’s health. This includes looking at their medical history, doing a physical check, and running tests. The aim is to make the patient as ready as possible for surgery and reduce risks.
Surgical Strategy Development
After looking at the images and assessing the patient, a surgical strategy is made. This means choosing the best surgery, planning the steps, and thinking about possible problems. A good plan is essential for a successful surgery.
| Diagnostic Tool | Purpose |
| MRI | Provides detailed images of soft tissues and helps identify abnormalities. |
| CT Scans | Offers detailed images of bony structures and helps assess the extent of disease. |
| Patient Assessment | Evaluates the patient’s overall health and identifies any risks. |
Patient Preparation for Skull Base Surgery
The journey to a successful skull base surgery starts with careful patient preparation. This detailed process includes several important steps. These steps work together to ensure the best results.
Medical Optimization
Medical optimization is key in patient preparation. It checks the patient’s health and manages any conditions that might affect the surgery or recovery. This could mean changing medications, controlling blood pressure, or addressing other health issues.
Pre-operative Instructions
Clear instructions before surgery are vital. Patients get detailed advice on how to prepare. This includes fasting, managing medications, and other important tips.
Psychological Preparation
Psychological preparation is also essential. It helps patients deal with the stress and anxiety of surgery. This might include counseling, learning about recovery, and support from family and healthcare teams.
| Preparation Aspect | Description |
| Medical Optimization | Assessing and managing underlying health conditions |
| Pre-operative Instructions | Guidance on preparing for surgery, including fasting and medication management |
| Psychological Preparation | Counseling and support to cope with stress and anxiety |
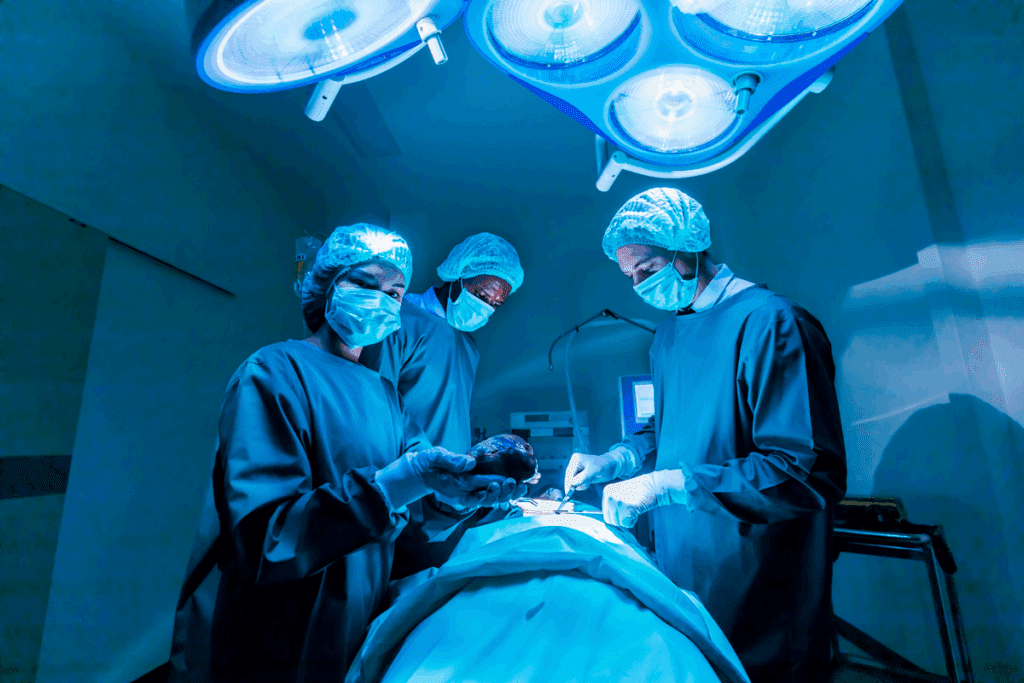
The Skull Base Surgery Procedure: Step by Step
Skull base surgery is a detailed process that requires careful planning and execution. It can be done in two main ways: endoscopic or minimally invasive surgery, and traditional or open surgery.
Anesthesia Administration
The first step in skull base surgery is anesthesia administration. Patients are given general anesthesia to keep them comfortable and pain-free. The anesthesiologist watches the patient’s vital signs closely to ensure the best conditions for the surgery.
Surgical Access Creation
Creating surgical access is key in skull base surgery. This involves making precise incisions and removing bone to reach the affected area.
Skin Incision Techniques
The type of skin incision used depends on the lesion’s location and nature. Surgeons might use endoscopic techniques for smaller incisions or traditional open surgery for larger ones.
Bone Removal Methods
Bone removal is often needed to access the skull base. The method chosen depends on the anatomy and the size of the lesion. Advanced imaging helps the surgeon pick the best bone removal method.
Tumor or Lesion Removal
The main goal of skull base surgery is to remove the tumor or lesion. The surgical team uses the access created to carefully remove the affected tissue. Advanced technology, like neuronavigation systems, helps with precision during this step.
| Step | Description | Key Considerations |
| Anesthesia Administration | General anesthesia is administered to the patient. | Monitoring vital signs, patient comfort |
| Surgical Access Creation | Incisions are made, and bone is removed to access the skull base. | Precision, minimal damage to surrounding tissue |
| Tumor or Lesion Removal | The affected tissue is dissected and removed. | Precision, use of advanced technology |
Surgical Approaches to the Skull Base
The skull base can be reached through several surgical paths. These include the anterior, lateral, and posterior routes. The choice of approach is key to the success of the surgery.
Anterior Approaches
Anterior approaches are used for conditions in the front of the skull base. They include:
- Transsphenoidal approach: Often used for pituitary tumors.
- Transfacial approach: May be used for tumors or lesions in the nasal cavity or sinuses.
These methods give direct access to the front of the skull base. They help avoid brain retraction and damage to nearby structures.
Lateral Approaches
Lateral approaches are for lesions on the sides of the skull base. Common lateral approaches include:
- Retrosigmoid approach: Used for tumors or vascular lesions near the cerebellopontine angle.
- Preauricular infratemporal fossa approach: Provides access to the infratemporal fossa and surrounding areas.
Lateral approaches give a wide view of the side of the skull base. They help in removing complex lesions.
Posterior Approaches
Posterior approaches are for conditions at the back of the skull base. These include:
- Suboccipital approach: Commonly used for tumors or vascular lesions in the posterior fossa.
- Far lateral approach: Provides access to the lateral and anterior aspects of the foramen magnum and the lower clivus.
Posterior approaches are vital for treating lesions in the back of the skull base. They allow for safe and effective treatment.
Advanced Technology in Skull Base Surgery
Advanced technologies are changing skull base surgery, making it more precise and safe. These technologies have greatly improved results for patients with complex skull base issues.
Neuronavigation Systems
Neuronavigation systems are key in skull base surgery. They give surgeons real-time feedback on their tools’ position compared to the patient’s anatomy. This boosts the accuracy of surgeries and lowers the chance of problems.
Intraoperative Imaging
Intraoperative imaging lets surgeons see the surgical area in real-time. This helps them adjust during the surgery. It’s very useful in skull base surgery because of the complex and delicate anatomy.
Surgical Robotics and Instrumentation
Surgical robotics and advanced tools have made surgeons more precise in skull base surgery. These advancements allow for less invasive procedures. This means patients recover faster and have better results.
The mix of these advanced technologies has greatly improved skull base surgery. It offers new hope to patients with complex conditions. As technology keeps getting better, we’ll see even more progress in surgery and patient care.
The Multidisciplinary Surgical Team
Skull base surgery is complex and needs a team effort. A team of different medical experts is key to success.
Neurosurgeons and ENT Specialists
Neurosurgeons and ENT specialists lead the team. Neurosurgeons know the brain and nervous system well. ENT specialists are experts in the ear, nose, and throat.
Together, they work to treat problems at the skull base.
Anesthesiologists and Nursing Staff
Anesthesiologists make sure patients are comfortable and safe. The nursing staff takes care of the patient before, during, and after surgery.
They watch over the patient and meet any needs that come up.
Support Specialists
Support specialists like radiologists and rehabilitation therapists are also important. They help with imaging and recovery. This ensures the patient gets all-around care.
| Specialist | Role in Skull Base Surgery |
| Neurosurgeons | Navigate and operate on the brain and nervous system |
| ENT Specialists | Provide expertise on ear, nose, and throat anatomy |
| Anesthesiologists | Ensure patient comfort and safety during surgery |
Potential Risks and Complications
Skull base surgery has risks that need to be known and managed. The surgery is complex and delicate. Knowing the possible complications helps in making informed choices.
Neurological Complications
Neurological problems can happen because of the surgery’s close location to important nerves. Damage to these areas can cause weakness, numbness, or paralysis. It’s important for both doctors and patients to understand these risks.
Infection and CSF Leak Risks
Infection is a risk with any surgery, including skull base surgery. CSF leaks can also happen, leading to infections like meningitis. It’s vital to manage these complications quickly to avoid long-term problems.
Long-term Considerations
Long-term effects include possible long-term neurological issues and the need for more surgeries. Patients should think about these when deciding on skull base surgery. Regular check-ups are key for watching and handling any ongoing issues.
Knowing the risks and complications helps patients make better choices about their treatment. This way, they can make informed decisions about their care.
Recovery Process After Skull Base Surgery
Recovering from skull base surgery is a detailed process. It includes care right after surgery and rehabilitation. Each patient’s recovery plan is made to fit their needs for the best results.
Immediate Post-Operative Care
Right after surgery, it’s important to watch the patient closely. They are kept in the ICU to catch any problems early. This helps prevent serious issues.
Hospital Stay Duration
How long a patient stays in the hospital depends on the surgery and their health. Most patients stay for a few days to a week or more.
Rehabilitation Needs
Rehabilitation is a big part of getting better. It helps patients regain their strength and skills. This includes physical, speech, and swallowing therapy.
Physical Therapy
Physical therapy is key to getting back on your feet. A physical therapist creates a plan just for you. This helps you regain your strength and mobility.
Speech and Swallowing Therapy
Some people need help with speaking and swallowing after surgery. These therapies are customized to meet each patient’s needs. They help improve communication and eating safely.
| Rehabilitation Therapy | Purpose | Benefits |
| Physical Therapy | Regain mobility and strength | Improved physical function, reduced risk of complications |
| Speech Therapy | Improve communication skills | Enhanced communication, improved quality of life |
| Swallowing Therapy | Address swallowing difficulties | Safe eating and drinking, reduced risk of aspiration |
Post-Operative Care and Follow-Up
After skull base surgery, taking care of yourself is key. This includes managing your meds, knowing what activities to avoid, and keeping up with doctor’s visits. You might also need imaging tests to check on your healing.
Medication Management
Managing your meds right after surgery is very important. You’ll likely take meds for pain, to prevent infection, and to reduce swelling. Always follow your doctor’s instructions and tell them about any side effects.
Activity Restrictions and Return to Normal Life
Right after surgery, you’ll need to avoid heavy lifting and bending. Your doctor will tell you when it’s okay to start doing more. They’ll also help you figure out when you can go back to work.
Follow-Up Appointments and Imaging
Regular check-ups are important to make sure you’re healing well. Your doctor might use MRI or CT scans to check on your surgery site. This helps them see how you’re doing and if everything is healing as it should.
| Follow-Up Care Aspect | Description | Importance |
| Medication Management | Adhering to prescribed medications for pain, infection, and swelling | High |
| Activity Restrictions | Avoiding heavy lifting, bending, or strenuous activities | High |
| Follow-Up Appointments | Regular check-ups with healthcare providers | High |
| Imaging Studies | MRI or CT scans to monitor healing and detect complications | High |
A leading neurosurgeon says, “The time after surgery is just as important as the surgery itself. Good care and follow-up are key for the best results and to avoid problems.”
“The key to a successful recovery after skull base surgery lies in the meticulous post-operative care and follow-up. It’s a team effort between the patient and the healthcare providers.”
— Medical Expert, Neurosurgeon
Conclusion
Skull base surgery is a complex and delicate procedure. It needs a team of experts and advanced technology for success. From the start to after the surgery, a detailed approach is key.
A multidisciplinary team including neurosurgeons, ENT specialists, anesthesiologists, and nurses is essential for successful skull base surgery. They work together to ensure the best care and results. Advanced tools like neuronavigation systems make the surgery safer and more precise.
Patients who get skull base surgery can see big improvements. They face fewer risks and can get back to their daily lives faster. The use of new technology and teamwork has changed the game for those with complex conditions.
Knowing how skull base surgery works and the role of a team helps patients. It lets them make better choices and get the best results.
FAQ
What is skull base surgery?
Skull base surgery is a complex procedure. It involves operating on the base of the skull. This area is at the bottom of the skull cavity.
It’s done to remove tumors, vascular issues, or injuries in this sensitive area.
What are the indications for skull base surgery?
Skull base surgery is needed for several reasons. This includes tumors, vascular problems, and injuries. These issues might need surgery to prevent more damage or to ease symptoms.
How is the skull base anatomy relevant to surgery?
The skull base is a complex area. It has many openings for the spinal cord, blood vessels, and nerves. Knowing the anatomy is key for surgeons to safely operate in this area.
What diagnostic imaging techniques are used for skull base surgery planning?
To plan skull base surgery, doctors use MRI, CT scans, MRA, MRV, and PET scans. These images help surgeons understand the condition’s extent. They plan a strategy tailored to each patient’s needs.
How are patients prepared for skull base surgery?
Patients get ready for surgery through medical checks, pre-op instructions, and mental preparation. This approach makes sure patients are physically and mentally ready for the surgery.
What are the different surgical approaches to the skull base?
There are several surgical approaches to the skull base. These include anterior, lateral, and posterior methods. The choice depends on the condition’s type and location.
What is the role of advanced technology in skull base surgery?
Advanced technology is vital in skull base surgery. It includes neuronavigation systems, intraoperative imaging, and surgical robots. These tools help surgeons perform complex surgeries safely and effectively.
What are the possible risks and complications of skull base surgery?
Skull base surgery can have risks like neurological problems, infection, and CSF leaks. Patients should know these risks to make informed decisions about their care.
What is the recovery process like after skull base surgery?
Recovery after skull base surgery involves immediate care, hospital stay, and rehabilitation. This includes physical, speech, and swallowing therapy. Patients gradually return to normal activities with their medical team’s guidance.
What is the importance of post-operative care and follow-up after skull base surgery?
Post-operative care and follow-up are key after skull base surgery. They ensure a smooth recovery and catch any issues early. This includes managing medications, activity restrictions, and follow-up appointments and imaging studies.
What is the role of a multidisciplinary team in skull base surgery?
A multidisciplinary team is essential in skull base surgery. It includes neurosurgeons, ENT specialists, anesthesiologists, and nurses. This team ensures patients get complete care and the surgery is done safely and effectively.
Are there any long-term considerations after skull base surgery?
Yes, long-term care is important after skull base surgery. This includes regular imaging to check for growths. Patients need to be aware of these considerations to manage their condition well.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2913918/