Last Updated on December 1, 2025 by Bilal Hasdemir

Nearly 2,000 people in the United States are diagnosed with a rare type of tumor at the cranial base each year.
The complexity of cranial surgery for tumor resection comes from the delicate structures around the tumor.
The approach for skull base tumor removal depends on the tumor’s location, size, and how it affects vital structures.
Key Takeaways
- The type of surgery used depends on the tumor’s characteristics.
- Cranial surgery is a complex procedure.
- Tumor resection requires careful planning.
- The goal is to remove the tumor while preserving surrounding structures.
- Surgery is often the primary treatment option.
Understanding Skull Base Tumors
Skull base tumors are complex because of the skull base’s structure. It’s the floor of the cranial cavity, supporting the brain. It also lets nerves and blood vessels pass through.
Definition and Anatomy of the Skull Base
The skull base is made of five bones: ethmoid, sphenoid, occipital, frontal, and temporal. These bones form the cranial floor. They have many foramina, or openings, for important structures to pass through.
Common Types of Skull Base Tumors
Skull base tumors can be benign or malignant. They include meningiomas, pituitary tumors, and chordomas. Meningiomas are usually benign. They grow from the meninges, which protect the brain and spinal cord.
| Tumor Type | Nature | Origin |
| Meningiomas | Usually Benign | Meninges |
| Pituitary Tumors | Typically Benign | Pituitary Gland |
| Chordomas | Malignant | Remnants of Notochord |
A specialist says, “Knowing the tumor type is key for treatment.” This shows how important accurate diagnosis is for managing these tumors.
Diagnosing Skull Base Tumors
Diagnosing skull base tumors is a detailed process. It starts with noticing early symptoms and using advanced imaging. It also includes precise biopsies. Getting the diagnosis right is key to choosing the right treatment.

Initial Symptoms and Warning Signs
Skull base tumors can cause many symptoms. These include facial pain, headaches, dizziness, vision problems, and hearing loss. These signs can be similar to other health issues, making it hard to diagnose.
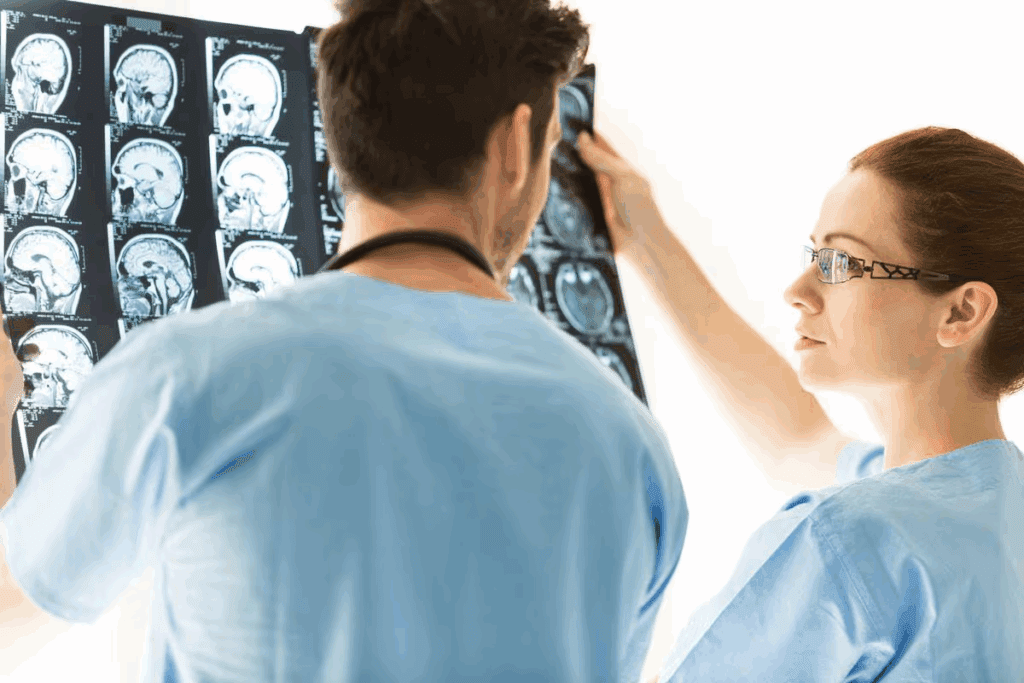
Diagnostic Imaging Techniques
Imaging is a big part of finding skull base tumors. MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans are key tools. MRI shows soft tissues well, while CT scans focus on bones. These help doctors see the tumor’s size, where it is, and how it affects nearby areas.
Biopsy Procedures and Pathological Assessment
A biopsy is vital to confirm a skull base tumor diagnosis. It involves taking a tissue sample for analysis. This analysis tells doctors the tumor’s type, how serious it is, and what treatment to use.
Pre-Surgical Evaluation Process
A detailed pre-surgical evaluation is key for checking if patients with skull base tumors can have surgery. This step includes many assessments to find the best treatment.
Determining Tumor Location and Size
Imaging techniques help find the exact location and size of the tumor. Knowing this is important for planning the surgery. MRI and CT scans give detailed info on the tumor’s size and where it is in relation to other parts.
Assessing Tumor Involvement with Critical Structures
It’s important to see how the tumor affects critical structures like nerves and blood vessels. This helps understand the surgery’s complexity. It also helps plan how to keep these important structures safe during the operation.
Patient Selection Criteria for Surgery
Choosing who can have surgery depends on several things. These include the tumor’s type, the patient’s health, and if they can handle surgery. A team of experts looks at these factors to decide the best treatment for each patient.
The Multidisciplinary Surgical Team
Skull base tumors need a team of experts for treatment. This team includes neurosurgeons, otolaryngologists, and others. They work together to care for the patient from start to finish.
Neurosurgeons and Their Role
Neurosurgeons are key in removing skull base tumors. They know how to safely take out tumors without harming the brain or skull. Their skills are vital for the patient’s safety.
Otolaryngologists and Skull Base Specialists
Otolaryngologists, or ENT doctors, are experts in the ear, nose, and throat. They help with tumors in these areas. Their knowledge is important for a successful surgery.
Supporting Medical Professionals
Other doctors like anesthesiologists, radiologists, and rehab specialists are also important. They help before, during, and after surgery. They make sure the patient gets the best care.
| Team Member | Role |
| Neurosurgeons | Surgical removal of tumors, preserving neural structures |
| Otolaryngologists | Managing tumors involving ENT areas |
| Supporting Professionals | Pre, intra, and post-operative care |
Preparing for Skull Base Tumor Surgery
Getting ready for skull base tumor surgery is a detailed process. It’s all about making sure patients are safe and the surgery goes well. This includes medical checks, imaging tests, and special instructions for patients.
Medical Clearance Requirements
Patients need to get medical clearance before surgery. This means their doctor checks their health, looks at any past medical issues, and sees if they’re ready for surgery. Getting cleared is key to spotting and fixing any possible risks.
Pre-Surgical Imaging and Planning
Imaging tests like MRI and CT scans are very important before surgery. They give the surgical team clear pictures of the tumor and the area around it. This helps them plan the best way to do the surgery.
Patient Instructions Before Surgery
Patients get specific instructions to follow before surgery. These might include what medications to take or not take, how long to fast, and other prep steps. Following these instructions is important to reduce risks and make the surgery go smoothly. The healthcare team will guide and support patients every step of the way.
Skull Base Tumor Removal: Surgical Approaches
Skull base tumor surgery uses different methods. Each method is picked based on the tumor’s size, location, and how it affects nearby areas. Choosing the right approach is key to remove the tumor safely and effectively.
Open Craniotomy Approaches
Open craniotomy means cutting the skull to get to the tumor. It’s often used for big tumors or those hard to reach. Open craniotomy lets doctors see and work on the tumor directly, which is good in some cases. The choice depends on the tumor and the patient’s health.
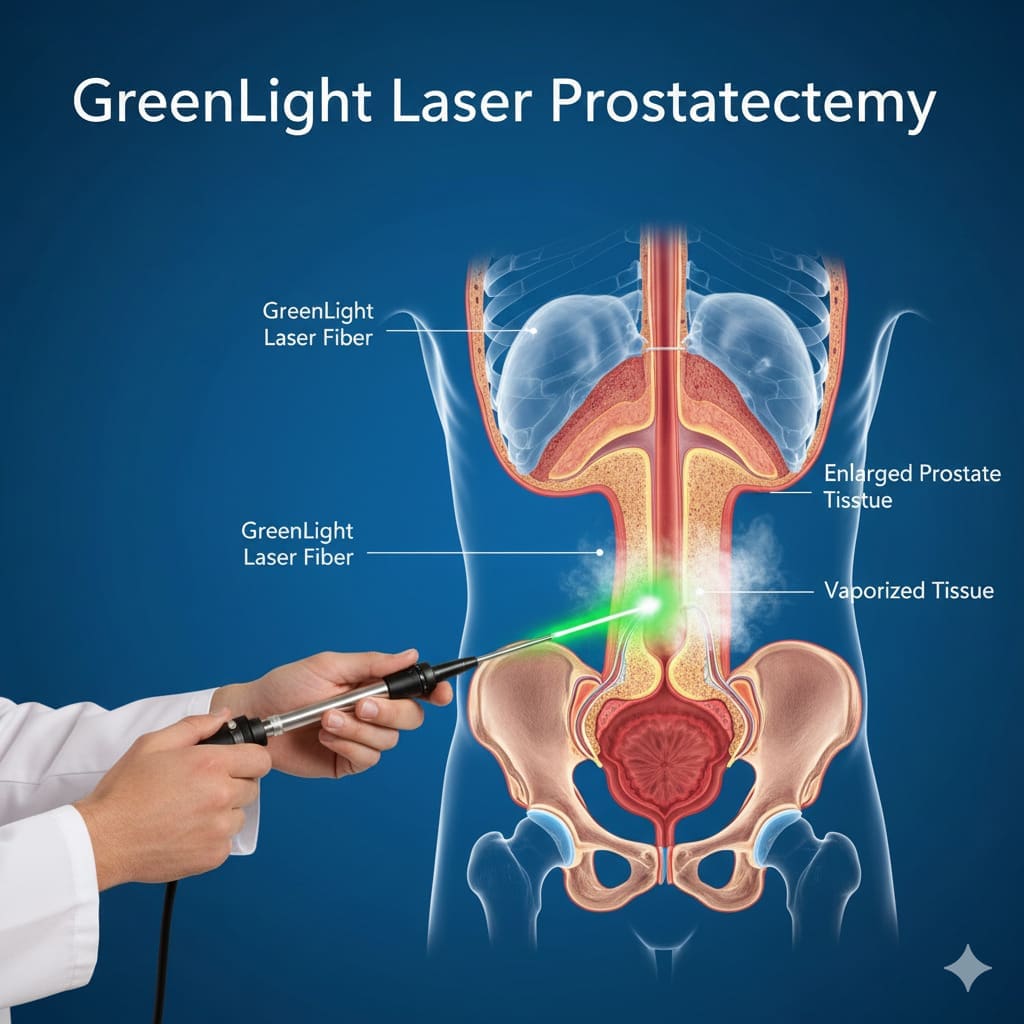
Endoscopic Endonasal Approaches
Endoscopic endonasal surgery is a minimally invasive method. It uses an endoscope through the nose to reach the tumor. This method is great for tumors in the nasal area. It has the benefits of less recovery time and less scarring. But, it needs special training and tools.
Combined and Keyhole Approaches
For some tumors, a combined approach is used. This mixes open and endoscopic methods. Keyhole surgery, with smaller cuts, is also being explored. These methods are customized for each patient and tumor.
Choosing a surgical method for skull base tumors is a team effort. Knowing about these options helps patients understand their treatment choices. It also shows why a certain surgery is recommended.
Step-by-Step Surgical Procedure
The surgical process for removing skull base tumors is very detailed and requires a lot of skill. It has many stages, each one important for removing the tumor successfully.
Anesthesia and Positioning
The first step is to give the patient anesthesia. This makes sure they are comfortable and safe during the surgery. Then, the patient is placed in a way that helps the surgeon get to the tumor easily.
Creating Surgical Access
To get to the tumor, the surgeon makes precise cuts. They might also need to move or remove some parts of the body. The method used depends on where the tumor is, how big it is, and the patient’s body.
Tumor Identification and Removal Techniques
With access to the tumor, the team uses special tools to find its edges. Then, they carefully cut out the tumor, making sure to not harm the nearby important parts.
Closure and Reconstruction
After removing the tumor, the team works on fixing the area. They might use grafts, implants, or other materials to make the area look and work like before.
| Surgical Stage | Description | Key Considerations |
| Anesthesia and Positioning | Administering anesthesia and positioning the patient for optimal access. | Patient comfort and safety, optimal access to tumor site. |
| Creating Surgical Access | Making incisions and adjusting anatomical structures to reach the tumor. | Tumor location, size, and patient anatomy. |
| Tumor Identification and Removal | Identifying tumor boundaries and removing the tumor. | Preserving surrounding critical structures. |
| Closure and Reconstruction | Closing the defect and reconstructing the affected area. | Restoring normal anatomy and function. |
Advanced Technologies in Skull Base Surgery
Advanced technologies are changing skull base surgery for the better. They make surgeries more precise and safe. New tools and methods have greatly improved how well surgeries go.
Intraoperative Navigation Systems
Intraoperative navigation systems guide surgeons in real-time. They help find important structures during surgery. This makes removing tumors more accurate and safer for nearby areas. Improved navigation is key in complex surgeries.
Intraoperative Monitoring
Intraoperative monitoring checks neural function during surgery. It spots any damage right away. This lets surgeons act fast to prevent more harm. Electromyography (EMG) and electroencephalography (EEG) are important for keeping nerves safe.
Surgical Robotics and Visualization Tools
Surgical robotics and advanced visualization tools are changing surgery. Robots give surgeons better control and precision. Tools like high-definition cameras and 3D visualization give a clearer view. As one expert said,
“The future of skull base surgery lies in the continued integration of technology and surgical expertise.”
These technologies help patients recover faster and get better care. They make skull base surgery safer and more effective.
Post-Surgical Care and Recovery
Skull base tumor surgery starts a journey of recovery. It involves careful post-operative care and watching the patient closely. The recovery process includes immediate care, a hospital stay, and rehabilitation at home.
Immediate Post-Operative Care
Right after surgery, patients go to the ICU for close watch. Careful observation is key to spot and handle any issues fast. This stage focuses on checking vital signs, brain function, and managing pain well.
Hospital Stay Duration
The time in the hospital depends on the surgery’s complexity and the patient’s health. Usually, patients stay a few days to a week. The medical team keeps an eye on the patient and gives needed care and therapy.
Rehabilitation and Home Recovery Guidelines
When they leave the hospital, patients get guidelines for home recovery. They learn about managing medicine, follow-up visits, and lifestyle changes. Rehabilitation might include physical, speech therapy, or other support to help patients get stronger and more functional.
By sticking to the post-surgical care and recovery plan, patients can heal better and get the best results.
Potential Complications and Management
Skull base tumor removal surgery has possible complications that need careful management. Understanding these is key for both patients and healthcare providers.
Common Surgical Complications
Complications can include infection, bleeding, and cerebrospinal fluid (CSF) leaks. Infection management uses antibiotics. CSF leaks might need more surgery to fix the dura mater.
“Monitoring closely and acting quickly are vital,” neurosurgeons say.
Neurological Complications
Neurological issues can happen because of the tumor’s location. These might cause facial weakness or trouble swallowing. Intraoperative monitoring and advanced surgical techniques aim to reduce these risks.
Long-Term Management Strategies
Long-term care needs a team effort, including rehab for any nerve issues. Regular check-ups are important to watch for any return of the tumor or late problems. A comprehensive care plan tailored for the patient is key for the best results.
A leading neurosurgeon notes, “Good long-term care is essential for a patient’s quality of life after surgery.”
Non-Surgical Treatment Alternatives
Skull base tumor treatment isn’t just surgery. Options like radiation therapy, chemotherapy, and observation are also available. These choices depend on the tumor’s type, size, and the patient’s health.
Radiation Therapy Options
Radiation therapy is a non-surgical way to treat tumors. It uses high-energy particles or waves to kill cancer cells. For skull base tumors, stereotactic radiosurgery and intensity-modulated radiation therapy (IMRT) are often used.
These methods are precise. They target the tumor without harming nearby healthy tissues.
| Radiation Therapy Type | Description | Benefits |
| Stereotactic Radiosurgery | Delivers high dose radiation in a single fraction | High precision, minimal side effects |
| Intensity-Modulated Radiation Therapy (IMRT) | Delivers radiation in multiple fractions, tailored to tumor shape | Effective for complex tumor shapes, reduces damage to surrounding tissues |
Chemotherapy and Targeted Treatments
Chemotherapy uses drugs to kill cancer cells. It can be effective for some skull base tumors, often used with other treatments. Targeted therapy also targets specific genes or proteins to slow tumor growth.
Observation Strategy for Certain Tumors
For slow-growing or benign tumors, watching them closely might be the best plan. This means regular imaging tests. It’s a way to act fast if the tumor grows or causes problems.
Conclusion
Removing skull base tumors is a complex task. It needs a team effort from many experts. Advances in surgery and technology have made surgical outcomes better for patients. Skilled neurosurgeons, otolaryngologists, and other medical professionals work together to care for patients.
The success of skull base tumor removal depends on several things. Accurate diagnosis, careful planning, and good post-surgery care are key. By focusing on these, doctors can help patients live better lives.
As medical tech keeps getting better, surgical outcomes will likely get even better. This means more effective treatments for patients with skull base tumors. The main goal is to keep patient care at the center, ensuring patients get all the support they need.
FAQ
What is skull base surgery?
Skull base surgery is a procedure to remove tumors or lesions at the base of the skull. It requires a team of neurosurgeons, otolaryngologists, and other experts.
How do you remove a tumor from the skull base?
Removing a tumor from the skull base involves different surgical methods. These include open craniotomy, endoscopic endonasal approaches, or a combination of both. The choice depends on the tumor’s location, size, and how it affects nearby structures.
What are the symptoms of a skull base tumor?
Symptoms of a skull base tumor can vary. They may include headaches, hearing loss, vision changes, facial numbness or weakness, and trouble swallowing. These symptoms depend on the tumor’s location and size.
How is a skull base tumor diagnosed?
Diagnosing a skull base tumor involves several steps. It includes MRI or CT scans and biopsy procedures. These help confirm the tumor’s presence and type.
What is the role of a multidisciplinary team in skull base surgery?
A team of neurosurgeons, otolaryngologists, and other experts is key in skull base surgery. They work together to provide the best care and outcomes for patients.
What are the possible complications of skull base tumor surgery?
Surgery for skull base tumors can have complications. These may include infections, bleeding, or damage to nerves. Such complications need careful management and follow-up care.
What are the non-surgical treatment options for skull base tumors?
Non-surgical treatments for skull base tumors include radiation therapy, chemotherapy, or observation. The choice depends on the tumor’s type, size, and the patient’s health.
How long is the recovery period after skull base tumor surgery?
Recovery time after skull base tumor surgery varies. It depends on the surgery’s complexity, the patient’s health, and any complications. It usually takes several weeks or months of rehabilitation.
What is the importance of intraoperative navigation systems in skull base surgery?
Intraoperative navigation systems are vital in skull base surgery. They help surgeons accurately locate and remove tumors. This minimizes damage to nearby critical structures.
Can tumors be removed from the skull base?
Yes, tumors can be removed from the skull base. The approach depends on the tumor’s characteristics and the patient’s health. The goal is to achieve the best outcomes and minimize complications.
What is the role of surgical robotics in skull base surgery?
Surgical robotics and visualization tools are increasingly used in skull base surgery. They enhance precision, dexterity, and visualization. This can improve outcomes and reduce complications.
How is the location and size of a skull base tumor determined?
The location and size of a skull base tumor are determined by diagnostic imaging. Techniques like MRI or CT scans provide essential information for planning and managing the patient’s care.
What are the benefits of minimally invasive techniques in skull base surgery?
Minimally invasive techniques, like endoscopic endonasal approaches, offer benefits in skull base surgery. They reduce trauma, lower post-operative pain, and speed up recovery. This can lead to better patient outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4899518/