Last Updated on November 27, 2025 by Ugurkan Demir

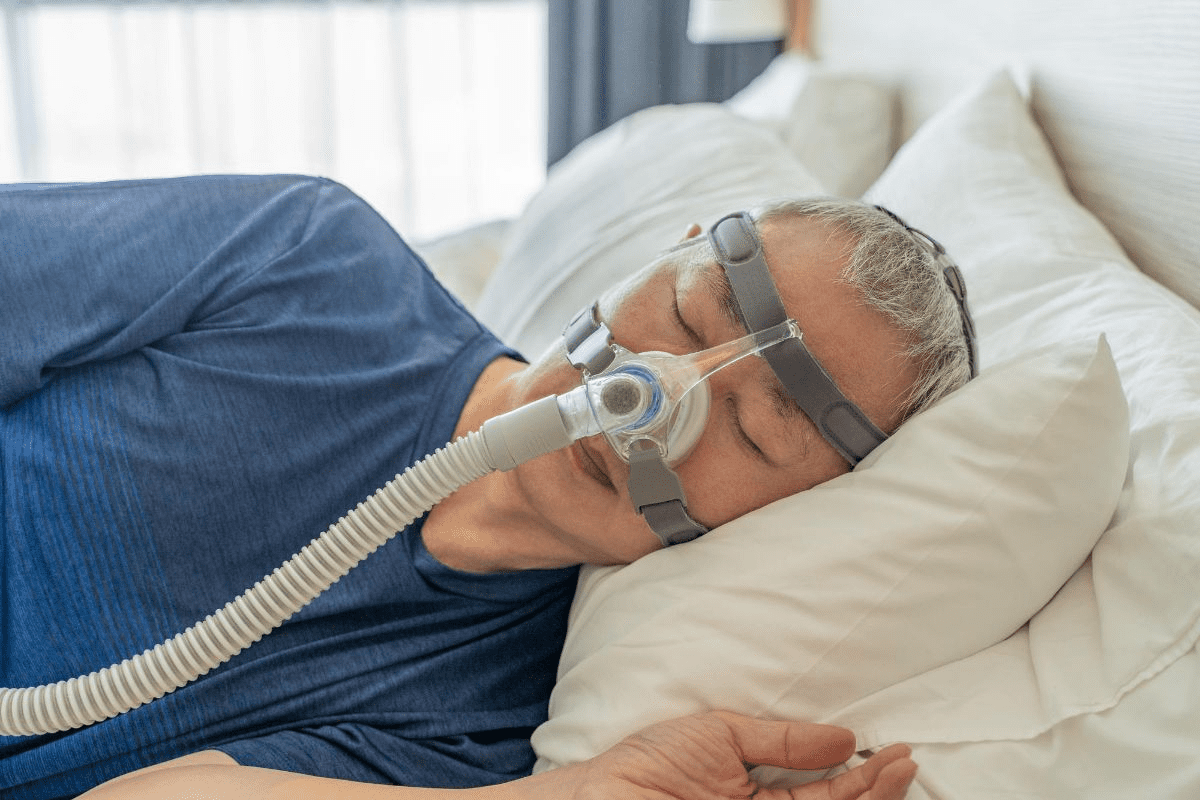
Obstructive sleep apnea (OSA) is common in adults in the United States, affecting 10-30%. Many find CPAP therapy hard to stick with because of discomfort or other issues.
Effective treatment options beyond traditional CPAP therapy are available. At Liv Hospital, we focus on personalized care. We offer a variety of alternative treatments. Our approach ensures each person gets the support and guidance they need.
We will look at seven proven alternative apnea treatments. These can greatly improve your life, from new surgical methods to simple lifestyle changes.
7 sleep apnea machine alternatives for effective treatment without the use of a traditional CPAP device.
Key Takeaways
- Obstructive sleep apnea affects a significant portion of adults in the US.
- CPAP therapy has limitations, and alternative treatments are available.
- Liv Hospital offers personalized care and extensive support.
- Seven alternative treatments will be discussed.
- Advanced surgical innovations and lifestyle adjustments are among the alternatives.
Understanding Sleep Apnea and Why People Seek CPAP Alternatives
Millions of people suffer from obstructive sleep apnea (OSA). It causes breathing to stop and start during sleep. This happens because the airway gets blocked.
What is Obstructive Sleep Apnea (OSA)?
OSA is the most common sleep apnea type. It happens when the throat muscles relax, blocking the airway. This can cause loud snoring and gasping sounds.
Many things can cause OSA, like being overweight or having a narrow airway. Lifestyle choices, like smoking, can make it worse. Knowing the cause helps find the best treatment.
The Prevalence and Health Risks of Untreated Sleep Apnea
Sleep apnea affects about 30 million adults in the U.S. If not treated, it can cause heart disease and diabetes. It also makes people more likely to have accidents because they’re tired.
Seeing a doctor is key if you think you have sleep apnea. Early treatment can make a big difference in your life.
Why Many Patients Struggle with CPAP Therapy
CPAP therapy is a common treatment for OSA. It uses a machine to push air through a mask. But, many find it uncomfortable and claustrophobic.
Studies show 30-40% of people stop using CPAP because of these issues. This is why looking for other treatments is important. It helps improve life for those with sleep apnea.
The Importance of Proper Sleep Apnea Diagnosis Before Seeking Alternatives

Getting an accurate diagnosis is key to treating sleep apnea well. It’s vital to know the details of your condition before looking for CPAP alternatives.
Every case of sleep apnea is different. There’s no one-size-fits-all solution. Let’s look at how diagnosis affects treatment choices.
Types of Sleep Apnea and Their Differences
Sleep apnea is not just one condition. It’s a range of disorders that cause breathing pauses during sleep. The main types are obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome.
- Obstructive Sleep Apnea (OSA): The most common form, caused by a physical blockage of the airway, typically due to relaxation of the throat muscles.
- Central Sleep Apnea (CSA): Occurs when the brain fails to send the appropriate signals to the muscles that control breathing.
- Complex Sleep Apnea Syndrome: A combination of OSA and CSA, also known as treatment-emergent central sleep apnea.
Knowing your type of sleep apnea is key to finding the right treatment.
Diagnostic Tests and Severity Assessment
Diagnosing sleep apnea requires both clinical evaluation and tests. The most common test is an overnight sleep study, called polysomnography (PSG).
Diagnostic Test | Description | Use in Sleep Apnea Diagnosis |
Polysomnography (PSG) | Overnight sleep study in a lab | Comprehensive assessment of sleep patterns and apnea events |
Home Sleep Apnea Testing (HSAT) | Portable device used at home | Simplified diagnosis for suspected OSA |
Multiple Sleep Latency Test (MSLT) | Daytime test measuring sleep tendency | Assesses daytime sleepiness and possible narcolepsy |
These tests help figure out how severe your sleep apnea is. This is usually measured by the Apnea-Hypopnea Index (AHI).
Working with Healthcare Providers to Find the Right Treatment
After diagnosis, working with healthcare providers is key to finding the right treatment. You might try different alternatives to CPAP, like oral appliances, positional therapy, or lifestyle changes.
We suggest asking your healthcare provider about:
- The specific type and severity of your sleep apnea
- All available treatment options, including their benefits and possible side effects
- The importance of follow-up evaluations to check if treatment is working
By working with your healthcare team, you can find a treatment that improves your life without CPAP.
Oral Appliances: Mandibular Advancement Devices (MADs)
MADs are a big step forward in treating sleep apnea, unlike traditional CPAP machines. These custom-made devices fit in the mouth. They move the jaw forward to keep the airway open while you sleep.
Mechanism of Action
MADs move the lower jaw forward. This stops the airway from collapsing. It’s key to keeping the airway open, which is harder when you’re sleeping.
By keeping the airway open, MADs cut down on apneic events. This improves your sleep quality.
Types of Oral Appliances
There are many types of oral appliances for sleep apnea. These include:
- Mandibular Advancement Devices (MADs)
- Tongue Retaining Devices (TRDs)
- Combination devices that both advance the mandible and retain the tongue
Each device is chosen based on the patient’s needs, the severity of sleep apnea, and personal preferences.
Effectiveness Compared to CPAP
Studies show MADs can be as good as CPAP for some patients. Here’s a comparison:
Treatment | Effectiveness in Reducing Apnea Events | Patient Compliance |
CPAP | High | Variable, often low due to discomfort |
MADs | Moderate to High | Generally higher than CPAP due to greater comfort |
CPAP is very effective, but some patients struggle with it. MADs are more comfortable, leading to better long-term use.
“The use of oral appliances like MADs represents a significant shift in the management of sleep apnea, providing patients a more tolerable and effective treatment option.” – Medical Expert, Sleep Specialist
Potential Side Effects and Considerations
MADs are usually well-tolerated, but there are side effects. These include:
- Jaw discomfort or pain
- Excessive salivation
- Changes in bite or dental alignment
It’s important to see a healthcare provider regularly. This helps monitor side effects and adjust treatment as needed.
In summary, MADs are a good alternative to CPAP for many sleep apnea patients. They are effective and easy to use, making them a popular choice for managing the condition.
Positional Therapy: Preventing Back Sleeping
Sleep position is key in managing sleep apnea. Many with sleep apnea have worse symptoms when sleeping on their backs. Positional therapy uses devices to stop back sleeping, helping to lessen apnea severity.
The Connection Between Sleep Position and Apnea Severity
Sleeping on one’s back can make sleep apnea worse. The tongue and soft palate can block the airway more easily in this position. By avoiding back sleeping, people might see a decrease in apnea episodes.
A study in the Journal of Clinical Sleep Medicine showed positional therapy can lower AHI scores. This makes it a good alternative to CPAP for some.
Specialized Pillows and Position Trainers
There are many devices to stop back sleeping, like special pillows and position trainers. These devices support or give feedback to encourage side-sleeping. Some pillows have wedges or contours that make back sleeping uncomfortable.
Position trainers, worn around the neck or body, vibrate or give feedback when you roll onto your back. They help train you to sleep on your side.
“Positional therapy is a valuable treatment option for patients with positional OSA, providing a non-invasive and effective alternative to CPAP therapy.”
– Medical Expert, Sleep Specialist
Wearable Devices for Position Monitoring
Wearable devices also help monitor and change sleep position. These can be worn on the wrist or on clothes. They offer a convenient way to track and adjust sleep position.
Some wearable devices also track sleep duration and quality. This gives a better understanding of sleep patterns.
Who Benefits Most from This Approach
Positional therapy works best for those with mild to moderate sleep apnea who sleep on their backs. Those with severe sleep apnea might need other treatments.
Benefit | Description |
Non-invasive | Positional therapy does not require surgery or insertion of devices into the body. |
Easy to use | Devices such as pillows and position trainers are relatively simple to use. |
Effective for mild to moderate OSA | Positional therapy can significantly reduce AHI scores in patients with positional OSA. |
Understanding how sleep position affects apnea can lead to trying positional therapy. It’s a promising option for some, improving sleep and health.
Lifestyle Modifications: Weight Loss and Beyond
Weight loss and other lifestyle changes can greatly help sleep apnea symptoms. For those with obstructive sleep apnea (OSA), healthier habits can make a big difference.
The Impact of Weight Loss on Sleep Apnea Severity
Even a 10% weight loss can lead to big improvements in sleep apnea. This is because extra weight, mainly around the neck, can block the airway. This makes apnea episodes worse.
Key Benefits of Weight Loss for Sleep Apnea Patients:
- Reduced fat around the airway
- Improved lung capacity
- Enhanced overall sleep quality
Exercise Programs Specific to OSA
Regular exercise helps with weight loss and has its own benefits for sleep apnea. Activities like walking or swimming improve heart health and lessen apnea severity.
Exercise Type | Benefits for OSA |
Aerobic Exercise | Improves cardiovascular health, reduces apnea severity |
Yoga | Enhances respiratory function, reduces stress |
Strength Training | Increases muscle mass, improves overall health |
Dietary Changes to Reduce Apnea Symptoms
Eating a balanced diet is key for weight control and health. Foods high in fruits, veggies, and lean proteins can lower inflammation. This improves sleep quality.
Avoiding Alcohol and Sedatives
Alcohol and sedatives relax throat muscles, making sleep apnea worse. Staying away from these, mainly before bed, can cut down on apnea episodes.
By making these lifestyle changes, people with sleep apnea can see big improvements in their symptoms and life quality.
Exploring Sleep Apnea Machine Alternatives: Adaptive Servo-Ventilation (ASV)
For those looking for CPAP machine alternatives, Adaptive Servo-Ventilation (ASV) is a top choice. ASV is a positive airway pressure device that changes airway pressure to match your breathing. This makes it a more adaptive way to manage sleep apnea.
Differences from Traditional CPAP
Unlike CPAP, which keeps air pressure constant, ASV adjusts it in real-time. This is great for those with complex sleep apnea or trouble with fixed pressure settings.
Candidates for ASV Therapy
ASV is best for patients with central sleep apnea, complex sleep apnea, or Cheyne-Stokes respiration. It’s also for those who can’t use CPAP or have failed it.
Benefits and Limitations
ASV’s main advantage is its ability to adapt to your breathing. This can make it more effective and easier to tolerate for some. Yet, ASV devices are more complex and need careful monitoring and adjustments.
Key Benefits and Considerations of ASV Therapy:
- Adaptive pressure delivery
- Potential for improved tolerance
- Effective for complex sleep apnea
- More complex device requiring careful monitoring
Cost and Insurance Considerations
ASV devices are often pricier than CPAP machines, and insurance coverage can differ. It’s key to talk to your healthcare provider and insurance about the costs and coverage for ASV therapy.
Feature | ASV | Traditional CPAP |
Pressure Delivery | Adaptive, real-time adjustment | Constant, fixed pressure |
Patient Population | Complex sleep apnea, central sleep apnea | Obstructive sleep apnea |
Device Complexity | More complex, advanced technology | Simpler, more established technology |
Cost | Generally higher | Variable, often lower than ASV |
Hypoglossal Nerve Stimulation: Inspire Therapy
Inspire therapy is changing how we treat sleep apnea. It uses a device to stimulate the hypoglossal nerve. This nerve controls the tongue, keeping the airway open at night.
The Implantable Device
The device has three parts: a generator, a sensing lead, and a stimulation lead. The generator goes under the skin in the chest. The sensing lead is between the ribs to watch breathing.
The stimulation lead wraps around the hypoglossal nerve. It gives gentle stimulation to prevent the tongue from blocking the airway.
The Surgical Procedure and Recovery
The surgery to implant the device takes a few hours. It’s done under general anesthesia. Small incisions are made in the chest and neck.
Most patients can go home the same day or the next. It depends on their health and the surgeon’s advice.
After surgery, there might be some pain and swelling. This can be managed with pain meds. Patients should avoid hard activities for a few weeks to heal properly.
Effectiveness Data and Patient Satisfaction
Studies show hypoglossal nerve stimulation works well for sleep apnea. A study in the New England Journal of Medicine found it reduced apnea by at least 50%.
Study Outcome | Result |
Reduction in AHI | 50% or more |
Patient Satisfaction | High |
Complications | Low |
Qualifying Criteria for This Treatment
To get this therapy, patients need moderate to severe OSA. They must not be able to use CPAP and have a certain BMI. A sleep specialist must evaluate them to see if they qualify.
Hypoglossal nerve stimulation is a promising treatment for sleep apnea. It offers relief without the need for CPAP or masks.
Surgical Options for Treating Sleep Apnea
Surgical treatments are key for those with sleep apnea who haven’t seen improvement with other methods. These surgeries aim to fix issues that block the airway while sleeping.
Uvulopalatopharyngoplasty (UPPP)
UPPP is a surgery that removes extra tissue in the throat. This includes the uvula, soft palate, and sometimes tonsils. It helps make the airway wider, which can lessen sleep apnea symptoms.
Key benefits:
- Reduces tissue obstruction
- Can improve sleep quality
- May reduce symptoms of sleep apnea
Maxillomandibular Advancement (MMA)
MMA is a more complex surgery. It moves the upper and lower jaws forward to make the airway bigger. It’s often used for those with severe sleep apnea.
Advantages:
- Significant reduction in apnea events
- Improved facial aesthetics in some cases
- Potential for long-term results
Soft Palate Procedures
Soft palate procedures, like implants, aim to make the soft palate stiffer or change its position. This helps prevent it from blocking the airway.
These surgeries are less invasive than UPPP or MMA. They might be a good choice for those with mild to moderate sleep apnea.
Nasal Surgery for Airway Obstruction
Nasal surgery, like septoplasty or turbinate reduction, can help if nasal blockage is a problem. This is because nasal blockage can contribute to sleep apnea in some cases.
Choosing a surgical option for sleep apnea needs careful thought. It’s important to talk to a healthcare provider. They can help decide the best surgery for your specific situation and health.
When to Consult Your Doctor About Sleep Apnea Treatment Options
Talking to a doctor about sleep apnea treatment is key to managing it well. We’ve looked at different options instead of CPAP therapy. It’s important to know when to ask for medical advice to get the right care.
Warning Signs That Your Current Treatment Isn’t Working
If you notice these symptoms, it’s time to talk to your doctor about changing your treatment:
- Continued daytime fatigue despite treatment
- Increased frequency of sleep disruptions
- Worsening of sleep apnea symptoms
- Discomfort or side effects from the current treatment
Seeing these signs means it’s time to see your doctor. They can help find other treatments, like a cpap machine alternative or sleep apnea treatment without cpap.
Questions to Ask Your Sleep Specialist
When you talk to your doctor, be ready with questions. This ensures you understand your options well. Ask things like:
Question | Purpose |
What are the benefits and risks of other treatments? | To know the good and bad of new treatments |
How will we check if the new treatment works? | To make sure there’s a plan for checking progress |
Are there lifestyle changes that can help with the new treatment? | To make the treatment work better |
Asking the right questions helps you make smart choices about your treatment.
The Importance of Regular Follow-up Evaluations
Regular check-ups are key to seeing if your treatment is working. These visits help your doctor:
- Check how the treatment is affecting your sleep apnea
- Change the treatment if needed
- Deal with any side effects or concerns
By working with your doctor and going to regular check-ups, you can make your treatment better. This improves your life quality.
Getting help from a doctor about sleep apnea treatment is an ongoing process. Being active in your care helps you find the best alternative to cpap or treatment for you.
Conclusion: Finding the Right Sleep Apnea Treatment Path
We’ve looked at many effective ways to treat sleep apnea, other than CPAP. These include oral appliances, positional therapy, and lifestyle changes. We also talked about adaptive servo-ventilation, hypoglossal nerve stimulation, and surgery.
Finding the right treatment for sleep apnea is key to a better life. By learning about different options, patients can work with doctors to find the best treatment.
It’s important to think about what each person needs when looking for CPAP-free treatments. Regular check-ups and talking openly with doctors are essential in finding the right treatment.
Exploring these options and working with healthcare professionals can help patients beat sleep apnea. This journey is about finding a treatment that fits each person’s needs.
FAQ
What are the alternatives to CPAP therapy for sleep apnea?
Alternatives include oral appliances like Mandibular Advancement Devices (MADs), positional therapy, and lifestyle changes. Other options are Adaptive Servo-Ventilation (ASV), hypoglossal nerve stimulation therapy, and surgery.
How do oral appliances like MADs work to treat sleep apnea?
MADs move the lower jaw forward. This keeps the airway open, reducing sleep apnea episodes.
What is positional therapy, and how can it help with sleep apnea?
Positional therapy stops you from sleeping on your back. This can worsen sleep apnea. Special pillows and devices help you stay in a better position.
Can lifestyle changes really help alleviate sleep apnea symptoms?
Yes, changes like losing weight, exercising, and avoiding alcohol can help. So can dietary changes and not using sedatives.
What is Adaptive Servo-Ventilation (ASV), and who is it suitable for?
ASV adjusts to your breathing. It’s good for complex sleep apnea or when CPAP doesn’t work.
How does hypoglossal nerve stimulation therapy work?
This therapy implants a device that moves the tongue. It keeps the airway open during sleep.
What surgical options are available for treating sleep apnea?
Surgery includes Uvulopalatopharyngoplasty (UPPP), Maxillomandibular Advancement (MMA), and soft palate procedures. Nasal surgery also helps with airway blockage.
How do I know if my current sleep apnea treatment is not working?
Signs include constant sleepiness, loud snoring, and sleep disruptions. Talk to your doctor if you notice these.
What questions should I ask my sleep specialist about alternative treatments?
Ask about treatment effectiveness, side effects, and if it’s right for you. Also, what to expect during treatment.
Why are regular follow-up evaluations important for sleep apnea treatment?
Follow-ups let your doctor check if treatment is working. They can make changes and address any issues.
Are there any new or emerging treatments for sleep apnea that I should be aware of?
Yes, new treatments and technologies are being developed. Keep up with your doctor or medical resources for the latest information.
Reference
National Center for Biotechnology Information. (2025). How to Treat Sleep Apnea Without CPAP 7. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3738032