Last Updated on November 27, 2025 by Ugurkan Demir
Sleep apnea affects millions worldwide, disrupting lives and causing significant health concerns. For those diagnosed with obstructive sleep apnea, traditional treatments like CPAP therapy may not always provide relief. In such cases, sleep apnea surgery can be a viable alternative.
There are various surgical procedures available, including UPPP, genioglossus advancement, and maxillomandibular advancement. Understanding these options is key. At Liv Hospital, we guide patients through the process, ensuring a personalized approach to treatment.
Choosing the right surgery for sleep apnea involves considering the severity of the condition, anatomical factors, and overall health. We help patients navigate these decisions to reclaim restful nights and improve their quality of life.
How to choose the right sleep apnea surgery, reviewing options like UPPP, genioglossus advancement, and Inspire.

Obstructive Sleep Apnea (OSA) is becoming more common. It’s a serious health issue that needs to be understood better. OSA happens when breathing stops and starts during sleep because of an airway blockage.
OSA affects millions worldwide, across all ages. It’s linked to heart disease, diabetes, and other health problems. It can also lead to less productivity, higher healthcare costs, and more accidents.
Knowing about OSA’s global impact is key. It helps healthcare workers and leaders create plans for early detection and treatment.
Airway blockage in OSA comes from several factors. These include:
Knowing these causes helps in creating effective treatments for OSA.
Untreated OSA can cause serious health issues, including:
Untreated OSA’s health risks show why seeking medical help is important. Early treatment can greatly improve life quality for those with OSA.

It’s important to know the difference between non-surgical treatments and apnea surgery for sleep apnea. Sleep apnea, mainly obstructive sleep apnea (OSA), affects millions. It disrupts sleep quality and health.
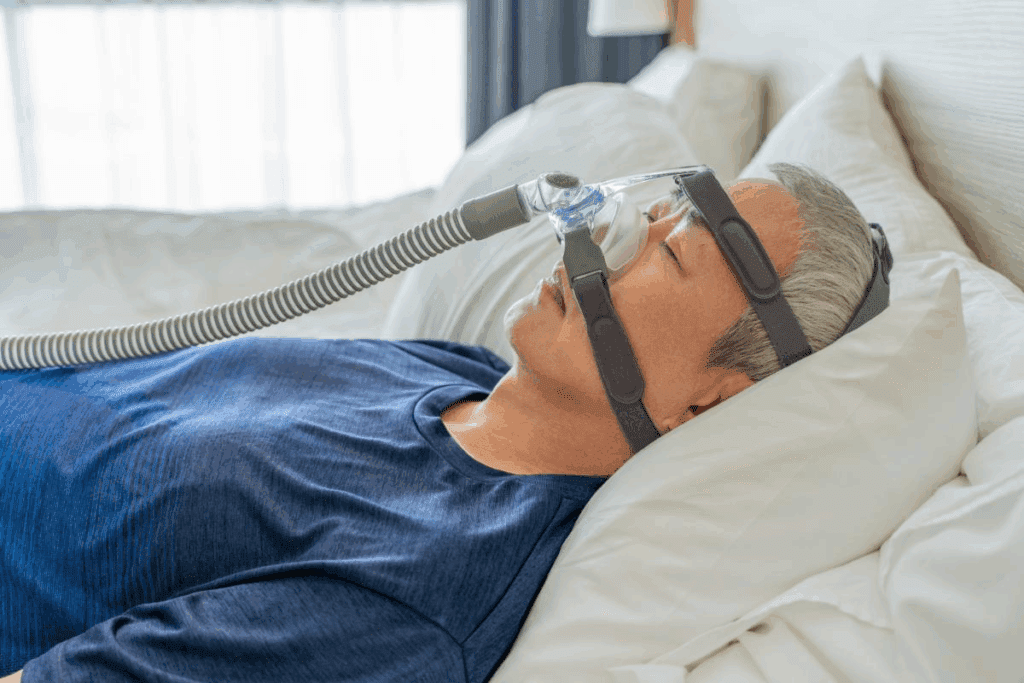
Non-surgical treatments are often the first choice for sleep apnea. CPAP (Continuous Positive Airway Pressure) therapy is a common and effective treatment for OSA. But, CPAP therapy has its own challenges.
CPAP therapy uses a mask over the nose and/or mouth connected to a machine. The machine sends pressurized air to keep the airway open. While it works well for many, it can be uncomfortable for others. People often complain about mask discomfort, machine noise, and feeling trapped.
CPAP therapy doesn’t fix the underlying problems that cause sleep apnea. For some, it’s not a lasting solution or it doesn’t fully get rid of sleep apnea symptoms.
For those who struggle with CPAP or find it doesn’t work, surgery is an option. Surgery aims to fix the physical blockages that cause sleep apnea. It might offer a more lasting solution.
Choosing surgery means a detailed evaluation, including sleep studies and airway checks. These help find where the blockages are. There are many surgeries, from simple to complex ones like maxillomandibular advancement.
Knowing the limits of CPAP therapy and the benefits of surgery helps patients and doctors make better choices. This way, they can find the best treatment for sleep apnea.
For obstructive sleep apnea, a detailed check-up is key to find the best surgery. Every patient is different, so a careful look is needed. This ensures the treatment fits their needs perfectly.
Sleep studies are vital for spotting sleep apnea and how bad it is. Polysomnography (PSG), or an overnight sleep study, is the top choice for diagnosing. It tracks brain waves, muscle activity, and heart rate while a person sleeps. This gives a full picture of their sleep.
These studies help us see how often apneic events happen, how much oxygen drops, and how sleep is affected. This info is key for figuring out how severe sleep apnea is and what treatment to choose.
Along with sleep studies, checking the airway is also important. Nasopharyngoscopy lets us see the upper airway and check its shape and how it works in different states, like when awake or asleep.
Tools like cephalometric radiographs and computed tomography (CT) scans give us more details about the airway’s bones and soft tissues. These help us understand the complex parts of the airway involved in sleep apnea.
Finding where the blockages are is key to picking the right surgery. We use sleep study and airway check data to find these spots.
This detailed info lets us create a treatment plan just for the patient. This might include surgeries for blockages in the nose, palate, tongue, or other areas.
Surgical options for sleep apnea include many types. These target the nasal passages, palate, tongue, and skeletal structure. We’ll dive into these to see how they help with sleep apnea symptoms.
Nasal procedures help if nasal blockage causes sleep apnea. They might include septoplasty for a deviated septum, turbinate reduction to shrink turbinate bones, and more. These surgeries aim to improve airflow through the nose.
These procedures can greatly improve sleep for some. But, it’s key to check if nasal blockage really causes sleep apnea through detailed tests.
Palatal procedures focus on the soft palate and uvula. These can block the airway in sleep apnea. A common one is Uvulopalatopharyngoplasty (UPPP), which removes excess tissue. Other methods include laser-assisted uvulopalatoplasty (LAUP) and palatal implants.
These surgeries aim to widen the airway by adjusting or removing tissues in the throat. The right procedure depends on the patient’s anatomy and sleep apnea severity.
Tongue-based interventions target the tongue’s role in sleep apnea. They include genioglossus advancement and hyoid suspension. These move the tongue or hyoid bone forward to open the airway.
These surgeries can be very effective for those with tongue obstruction. They can greatly reduce sleep apnea severity.
Skeletal surgeries, like maxillomandibular advancement (MMA), move the upper and lower jaws forward. This enlarges the airway. MMA is very effective for many, improving sleep apnea symptoms a lot.
MMA is often for those with severe sleep apnea who’ve tried other treatments. It needs careful planning, considering the patient’s face and health.
Uvulopalatopharyngoplasty, or UPPP, is a surgery for sleep apnea. It removes tissue in the mouth and throat to open the airway. This helps lessen sleep apnea symptoms.
The UPPP surgery removes the uvula and parts of the soft palate. Sometimes, the tonsils are also removed. Different techniques are used to make recovery easier and reduce risks.
UPPP can be tailored to fit each patient’s needs. Surgeons adjust the surgery based on the patient’s anatomy and sleep apnea severity.
Not everyone with sleep apnea is a good fit for UPPP. The best candidates have sleep apnea caused by palate obstruction. Their anatomy must also be suitable for the surgery.
Patients undergo detailed tests to see if UPPP is right for them. These tests include sleep studies and airway exams. They help find out if UPPP can help.
UPPP success varies. Some patients see big improvements, while others don’t notice as much.
Success Rate Category | Description | Percentage of Patients |
Significant Improvement | Patients showing a substantial reduction in sleep apnea symptoms | 40% |
Moderate Improvement | Patients experiencing some reduction in sleep apnea symptoms | 30% |
Limited Improvement | Patients with minimal or no significant change in sleep apnea symptoms | 30% |
It’s important to know these details. They help set realistic expectations and make informed choices about UPPP surgery.
Tongue-based procedures are key in treating obstructive sleep apnea. They aim to fix the tongue’s role in blocking the airway. We’ll look at these procedures, their benefits, and possible risks.
This technique moves the genioglossus muscle forward. This muscle is key for sticking the tongue out. It stops the tongue from blocking the airway at night.
Benefits: Opens the airway better, cuts down on sleep apnea.
Potential Complications: Swelling, pain, and changes in tongue feeling.
This method uses radio waves to shrink the tongue base. It’s a small procedure that helps reduce tongue blockage.
Benefits: It’s less invasive, heals fast, and lowers sleep apnea.
Potential Complications: Swelling and pain might happen.
This procedure lifts the hyoid bone to move the tongue and hyoid forward. It makes breathing easier.
Benefits: Stabilizes the airway, works well with other treatments.
Potential Complications: Swelling and changes in swallowing might occur.
Procedure | Benefits | Potential Complications |
Genioglossus Advancement | Improves airway patency, reduces apnea episodes | Swelling, pain, changes in tongue sensation |
Radiofrequency Ablation | Less invasive, quicker recovery, effective in reducing apnea episodes | Temporary swelling, pain |
Hyoid Suspension | Enhances airway stability, can be combined with other procedures | Swelling, changes in swallowing |
MMA surgery moves the upper and lower jaws to widen the airway. It helps those with sleep apnea a lot. It’s best for those with severe sleep apnea who haven’t found relief elsewhere.
The procedure moves the upper and lower jaws forward to open the airway. It uses bone cuts and devices to keep the jaw in place. An oral and maxillofacial surgeon with orthognathic surgery skills performs it.
The surgeon cuts the jawbones to move them forward. Then, plates, screws, or other devices hold the jaw in its new spot. This stops the airway from collapsing during sleep, cutting down on sleep apnea.
MMA surgery has a high success rate, 80% to 90%. It works well for many patients, reducing sleep apnea symptoms a lot.
Its success comes from fixing the airway blockage that causes sleep apnea. Moving the jaw opens the airway, making it harder for it to block during sleep.
Recovery from MMA surgery varies based on health and procedure complexity. Patients usually face swelling, bruising, and pain after surgery.
They might need pain meds and eat soft foods for weeks. Avoiding hard work for a while is also advised. Most can get back to normal in a few weeks, but full recovery takes months.
Following the surgeon’s advice is key for a smooth recovery. Regular check-ups help track healing and address any issues.
For those with sleep apnea who can’t use CPAP, Hypoglossal Nerve Stimulation (HGNS) is a good choice. It’s a new way to treat sleep apnea. A device is implanted to help keep the airway open while you sleep.
The HGNS device is under the skin. It has three parts: a lead, a generator, and a sensor. The lead is around the hypoglossal nerve, the generator is in the chest, and the sensor is between the ribs. It helps keep the airway open by stimulating the nerve at the right time.
Not everyone with sleep apnea can get HGNS. To qualify, you need:
Studies show HGNS works well for those who can’t use CPAP. It helps 70% to 80% of these patients. They see better sleep, feel more awake during the day, and live better lives.
Study | Success Rate | Patient Population |
STAR Trial | 66% | CPAP-intolerant patients |
HGNS System Trial | 78% | Patients with moderate to severe OSA |
Knowing how HGNS works helps doctors find the right patients. This way, they can offer a good treatment option for those with few other choices.
Obstructive sleep apnea often needs a multilevel surgical approach. This method is customized for each patient’s unique anatomy and blockages. It combines several surgeries to tackle different parts of the upper airway.
Multilevel surgery aims to treat all parts of the airway. It includes the nose, palate, tongue, and bones. By combining sleep apnea surgeries, we can tackle the complex anatomy better. This might lead to better results for patients.
The choice of procedures depends on the patient’s tests, like sleep studies and airway exams. This custom plan helps meet each patient’s needs, aiming for the best results.
When planning multilevel surgery, we think about the order of procedures. We decide if to do them all at once or in stages. This depends on the case’s complexity and the patient’s health.
Staging is key to lower risks and better recovery. By planning the order and timing, we aim to reduce complications and improve results.
Recovery from sleep apnea surgery with multiple procedures is longer and more complex. Patients should expect swelling, discomfort, and airway changes during recovery.
But, with the right care, many patients recover well and see big improvements in their sleep apnea. It’s vital for patients to follow instructions and attend follow-ups for a smooth recovery.
Choosing the right surgery for sleep apnea is a big decision. Each patient’s situation is different. So, a plan that fits them best is key.
The first step is to find out where the airway is blocked. We do this with detailed tests and exams.
Table: Obstruction Patterns and Corresponding Surgical Procedures
Obstruction Pattern | Surgical Procedure |
Nasal Obstruction | Nasal Surgery (e.g., septoplasty, turbinate reduction) |
Oropharyngeal Obstruction | Uvulopalatopharyngoplasty (UPPP) |
Tongue-Based Obstruction | Tongue-Based Procedures (e.g., genioglossus advancement) |
The severity of sleep apnea matters too. Mild cases might need simpler treatments. Severe cases might need more.
We look at the Apnea-Hypopnea Index (AHI) to see how severe it is. This helps us choose the right surgery.
We also think about the patient’s health and any reasons a surgery might not be right. Some health issues might make certain surgeries not possible.
How a patient lives and recovers is important too. We talk about how long it will take to get better, what care is needed, and how it might affect daily life.
By looking at all these things, we can make a treatment plan that really works for each patient. This way, they have the best chance of success.
Thinking about sleep apnea surgery means knowing the risks and complications. It’s key to weigh the good against the bad. Each surgery for sleep apnea has its own set of possible problems.
Each surgery for sleep apnea has its own side effects. For example, Uvulopalatopharyngoplasty (UPPP) might cause a sore throat or trouble swallowing. Genioglossus Advancement could lead to swelling or tongue changes. Knowing these side effects helps manage what to expect and how to care for yourself after surgery.
Medical Expert, a top sleep surgeon, says,
“The key to successful sleep apnea surgery lies not just in the procedure itself, but in the complete care before, during, and after the operation.”
Though rare, serious problems can happen with sleep apnea surgery. These include infections, bleeding, or bad reactions to anesthesia. Some surgeries might cause airway obstruction or permanent changes in speech or swallowing. It’s important to talk about these risks with your doctor.
Some sleep apnea surgeries can change your airway’s shape for good. For example, Maxillomandibular Advancement (MMA) can change your face and teeth. It’s important to know these long-term effects to be ready for any changes.
In summary, sleep apnea surgery has big benefits but also risks and complications. Knowing these helps patients make better choices. Always talk to your doctor to understand these complexities.
Choosing the right sleep apnea treatment is very important. It depends on how severe the sleep apnea is, the body’s structure, and overall health.
We looked at different surgical options, from nasal procedures to more complex surgeries. Each has its own benefits and risks. The success of sleep apnea surgery depends on a treatment plan made just for the patient.
Getting a full check-up is key to finding the best treatment. Working with healthcare experts helps patients make smart choices. This leads to better health and a better life.
In short, sleep apnea surgery can be very effective for the right patients. It’s all about picking the right treatment and getting the right care. This way, patients can manage their sleep apnea and sleep well every night.
Sleep apnea surgery is a set of procedures aimed at treating obstructive sleep apnea (OSA). It works by removing blockages in the upper airway. This helps improve breathing while sleeping.
There are several types of sleep apnea surgery. These include nasal procedures, palatal surgeries like UPPP, and tongue-based interventions. Skeletal surgeries like maxillomandibular advancement (MMA) and hypoglossal nerve stimulation (HGNS) are also available.
Choosing the right surgery involves a detailed diagnostic process. This includes sleep studies and airway exams. The goal is to find the specific blockage. The choice depends on the blockage, disease severity, patient health, and lifestyle.
UPPP is a surgery that removes excess throat tissue to widen the airway. It’s best for those with sleep apnea caused by soft palate obstruction.
MMA surgery moves the upper and lower jaws to enlarge the airway. It has a success rate of 80-90% for the right patients.
HGNS implants a device that moves the tongue to keep the airway open. It’s for those who can’t use CPAP therapy and have moderate to severe OSA.
Risks and complications vary by procedure. They can include pain, swelling, bleeding, infection, and impacts on speech or swallowing.
Surgery can greatly improve or cure sleep apnea for many. The success depends on the surgery type, OSA severity, and individual factors.
Yes, there are many surgical options for OSA. These range from soft tissue surgeries to skeletal advancements.
Multilevel surgery combines procedures to address obstructions at different airway levels. It offers a more complete treatment for sleep apnea.
Recovery time varies by surgery type and extent. It can range from a few weeks to several months for complex surgeries like MMA.
Yes, non-surgical treatments include CPAP therapy, oral appliances, and lifestyle changes. These are often tried before or with surgery.
CPAP therapy is a common first treatment. It delivers pressurized air through a mask to keep the airway open during sleep.
Surgery suitability depends on other health conditions and their impact on risk. A thorough evaluation by healthcare professionals is needed.
Tongue-based procedures, like genioglossus advancement and radiofrequency ablation, can be effective. Their success rate varies, but they help some patients.
Severity is determined through sleep studies, like polysomnography. These measure apneic events and oxygen levels during sleep.
National Center for Biotechnology Information. (2025). How to Choose Sleep Apnea Surgery A Complete. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11476387/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!