Last Updated on November 26, 2025 by Bilal Hasdemir

sleep next to chemo patient
When a loved one is getting chemotherapy, we all worry about safety. It’s normal to feel scared and unsure.
Many people wonder: is it safe to be around someone getting chemotherapy? The answer varies. It depends on the chemotherapy type and the person’s health.
We’ll look into the safety aspects. We’ll also talk about sleeping next to someone getting chemotherapy. This includes whether it’s safe to sleep beside a chemo patient.
Key Takeaways
- Chemotherapy safety precautions are crucial when in close contact with a patient.
- The type of chemotherapy affects the safety of close contact.
- Understanding the risks helps in making informed decisions.
- Precautions can minimize risks associated with chemotherapy.
- Guidance is available for those concerned about safety.
Understanding Chemotherapy and Its Effects

Chemotherapy is a key treatment for cancer. It destroys cancer cells but can also harm healthy cells. It’s important to understand how it works.
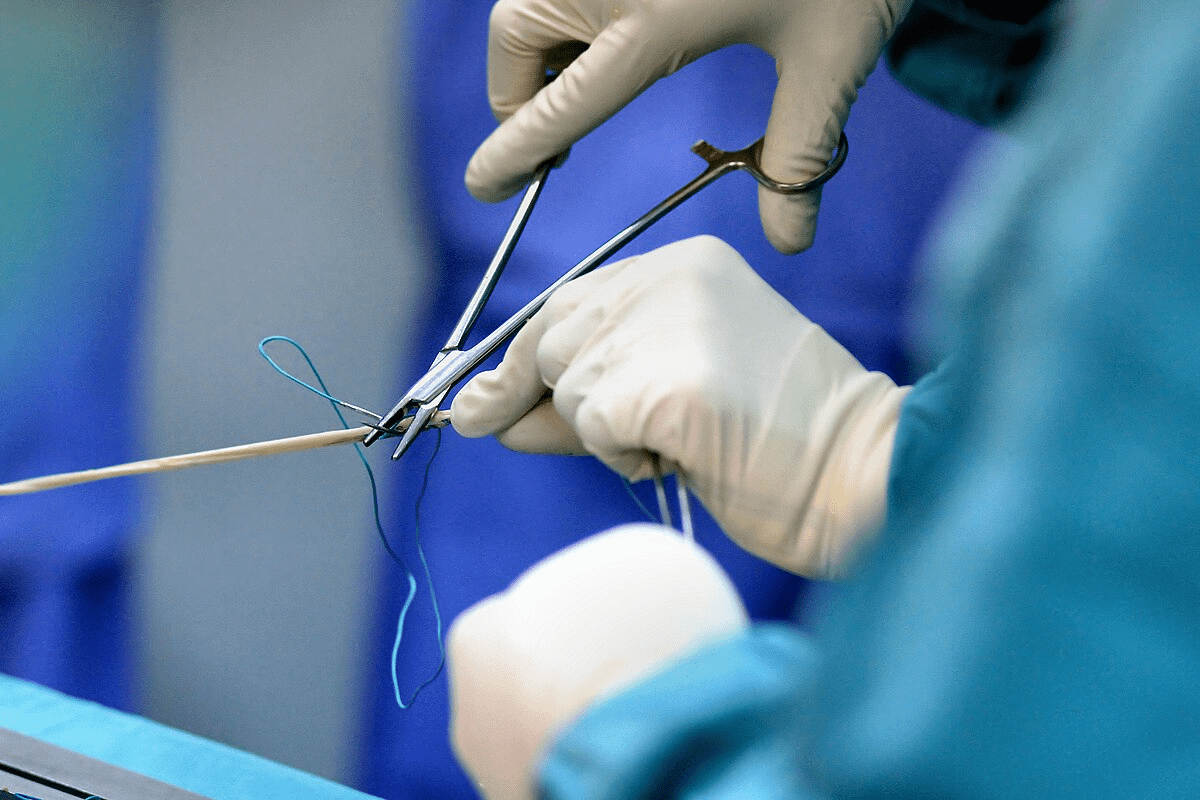
How Chemotherapy Works in the Body
Chemotherapy targets cells that grow fast, like cancer cells. But it also affects other fast-growing cells, like hair and the digestive tract. This is why chemotherapy can cause many side effects.
Chemotherapy drugs aim to kill or slow down cancer cells. The type of drug used depends on the cancer type, stage, and the patient’s health.
Common Side Effects of Chemotherapy
Chemotherapy can make you feel tired, nauseous, and cause hair loss. It also increases the risk of infections. The severity of these side effects varies among patients.
- Fatigue: Feeling extremely tired or weak
- Nausea and Vomiting: Chemotherapy can cause stomach upset
- Hair Loss: Many chemotherapy drugs cause hair to fall out
- Increased Risk of Infections: Chemotherapy can weaken the immune system
Myths vs. Facts About Chemotherapy Exposure
Many myths surround chemotherapy exposure. Some believe being near someone getting chemotherapy can expose you to the drugs. In reality, chemotherapy drugs are not transmitted through casual contact or proximity.
However, chemotherapy drugs can be found in urine, feces, and vomit after treatment. It’s important to practice good hygiene when handling these fluids to avoid exposure.
Understanding chemotherapy’s effects and debunking myths about exposure can ease concerns. By knowing the facts, we can better support those undergoing treatment.
Is It Safe to Sleep Next to a Chemo Patient?
It’s natural to worry about sleeping near someone who’s going through chemotherapy. We need to look at the medical advice, the role of bodily fluids, and when we should take precautions.
Medical Consensus on Proximity to Chemo Patients
Doctors mostly say it’s okay to be near someone getting chemo. But, there are rules to follow, especially about bodily fluids. The American Cancer Society says it’s key to avoid touching urine, stool, or vomit for the first 48 hours after treatment.
Understanding Bodily Fluids and Chemotherapy
Chemotherapy drugs can get out through different bodily fluids. It’s important to be careful to avoid touching these fluids. For example, wearing gloves and washing your hands well after touching urine, stool, or vomit can lower the risk of exposure.
Also, make sure to flush the toilet twice after use. Wash any dirty clothes or linens by themselves from other laundry. These steps can help lower the chance of getting exposed to chemotherapy agents.
Timeline: When Precautions Are Most Important
The first 48 to 72 hours after chemo treatment are the most critical. This is when the drugs in bodily fluids are most concentrated. Knowing this time frame helps plan and take the right steps to avoid exposure.
Even after this period, it’s still important to keep up with good hygiene. Understanding and following these guidelines helps keep everyone safe while still showing support and closeness during tough times.
Potential Risks of Close Contact During Chemotherapy
When someone is on chemotherapy, you might worry about being close to them. This includes sharing a bed. Chemotherapy uses strong drugs to fight cancer, affecting the body in many ways.
Types of Chemotherapy Drugs and Their Risk Levels
Chemotherapy drugs are grouped by risk level. Some are very risky because they are strong and can spread through bodily fluids. For example, some drugs can get out through urine, sweat, and other secretions, risking those nearby.
The risk of these drugs varies a lot. High-risk drugs need extra care to avoid exposure. Knowing the drugs used and their risks is key.
Routes of Potential Exposure
There are several ways to get exposed to chemotherapy drugs:
- Direct contact with bodily fluids like urine, feces, or vomit
- Skin-to-skin contact with the patient
- Sharing personal items like towels or razors
Knowing these ways helps lower risks. Wearing gloves when touching bodily fluids and not sharing personal items can help a lot.
Special Considerations for Pregnant Women and Children
Pregnant women and kids need extra care when near someone on chemotherapy. They might be more at risk because they are more sensitive and vulnerable.
Pregnant women should talk to their doctor about the risks of chemotherapy drugs. Kids should stay far away, and steps should be taken to limit their contact with the patient’s fluids.
By knowing the risks and taking steps to avoid them, we can keep everyone safe. This includes the person on chemotherapy and their loved ones.
Recommended Precautions When Sharing a Bed
When sharing a bed with someone getting chemotherapy, safety and comfort are key. Chemotherapy uses strong drugs to fight cancer. It’s usually safe to be near someone getting chemo, but there are steps to take to avoid risks.
General Hygiene Practices
Good hygiene is essential when sleeping with a chemo patient. Frequent handwashing is a simple yet effective way to lower the risk of exposure to chemo drugs or their byproducts.
- Wash your hands well with soap and water after using the bathroom, before eating, and after touching the patient or their bodily fluids.
- Encourage the chemo patient to wash their hands often too.
- Keep the bedroom tidy and avoid clutter that can harbor bacteria or other germs.
Handling Bodily Fluids Safely
Chemotherapy drugs can be found in urine, feces, and vomit. It’s important to handle these fluids safely to avoid exposure.
- Wear gloves when dealing with bodily fluids or touching items soiled with them.
- Use a disinfectant to clean any surfaces that have come into contact with bodily fluids.
- Flush the toilet twice after the patient has used it to reduce drug residue.
When Separate Sleeping Arrangements Might Be Necessary
In some cases, it might be better to sleep in separate beds. This is especially true if the patient is having severe side effects or if the chemo drugs are very toxic.
- Talk to healthcare professionals to understand the risks and decide what’s best.
- Think about sleeping in separate beds during the most intense chemo phases.
- Be ready to change your sleeping arrangements based on the patient’s health and treatment plan.
Can You Sleep With Someone on Chemo? Immune System Considerations
Sleeping next to someone on chemotherapy needs careful thought about their immune system. Chemotherapy weakens the immune system a lot. This makes patients more likely to get sick.
Protecting the Chemo Patient from Infections
To keep the chemo patient safe, it’s key to reduce their risk of getting sick. Here are some ways to do it:
- Practice Good Hygiene: Washing hands often is very important, especially before touching the patient.
- Avoid Crowds and Sick People: Try to stay away from crowded places and people who are sick.
- Clean the Environment: Clean and disinfect things that people touch a lot often.
Protecting Yourself from Potential Exposure
Even though catching cancer or chemotherapy is very rare, you can still take steps to lower your risk:
- Use Gloves: Wear gloves when you handle body fluids, like during medical care or cleaning up after the patient.
- Wash Clothing and Bedding: Always wash the patient’s clothes and bedding by themselves to avoid spreading germs.
Signs of Compromised Immunity to Watch For
It’s important to watch for signs of a weak immune system in both you and the chemo patient. Look out for:
- Fever or chills
- Frequent or severe infections
- Unusual fatigue or weakness
By knowing these signs and taking the right steps, you can help keep both yourself and the chemo patient safe from the risks of a weak immune system.
Emotional Aspects of Sleeping Arrangements During Cancer Treatment
The emotional side of sleeping arrangements during cancer treatment is key for both patients and their loved ones. It’s vital to think about the emotional side when we talk about care and support.
The Psychological Benefits of Physical Closeness
Being close during cancer treatment has many psychological benefits for both the patient and their partner. It brings comfort, reassurance, and security, which are very important during tough times. Sleeping together can release oxytocin, known as the “love hormone,” which helps with bonding and relaxation.
For those getting chemotherapy, having a loved one nearby can reduce loneliness and anxiety. It’s crucial for partners to know their presence is a big emotional support.
Addressing Fears and Anxieties About Contact
Even though closeness is good, we must talk about fears and anxieties about touching someone with chemotherapy. Worries about getting sick or being exposed to drugs are common. Talking openly and learning about safety can help ease these worries.
Talking to healthcare providers about these risks and precautions is a good idea. This way, couples can make smart choices about where to sleep.
Maintaining Intimacy During Treatment
Maintaining intimacy during cancer treatment is crucial for both partners’ emotional health. While we often think of physical touch, emotional closeness is just as important. Sleeping together can help keep that emotional bond strong.
Couples should find ways to keep their emotional connection alive. This can be through touch, talking, or just being there for each other. They need to adapt to the changes that come with cancer treatment.
Practical Sleeping Arrangements for Comfort and Safety
Setting up the right sleeping space is key for comfort and safety. This is especially true when someone is going through chemotherapy. It’s important to think about how to keep the sleeping area comfortable and safe for both the patient and their partner.
Bedding Considerations and Laundering Practices
Choosing the right bedding and how often to wash it is crucial. Machine-washable bedding that can handle hot water is best. It’s also good to change sheets often, especially if the patient sweats a lot or has open wounds.
Washing bedding in hot water once a week is a good rule. If the patient sweats a lot or leaks fluids, you might need to wash it more often.
| Bedding Consideration | Recommendation |
| Material | Machine-washable, breathable fabrics |
| Washing Frequency | At least once a week, or more often if needed |
| Water Temperature | Hot water |
Managing Night Sweats and Other Symptoms
Night sweats are common when someone is on chemotherapy. Using moisture-wicking bedding can help keep both partners dry. Keeping the bedroom cool can also help reduce night sweats.
If the patient has pain or discomfort, changing how they sleep or using extra pillows can help. This can make them more comfortable.
Creating a Restful Environment for Both People
Creating a peaceful sleep space is more than just the bedding. Keeping the room quiet and at a good temperature is important. Blackout curtains or a white noise machine can also help improve sleep.
It’s also vital to think about emotional comfort. Maintaining intimacy through gentle touch or just being there can offer emotional support during tough times.
“A restful environment is not just about physical comfort; it’s also about creating a space where both partners feel emotionally supported and secure.”
Communication Strategies with Your Partner About Sleeping Needs
Talking openly is key when you’re sleeping next to someone going through chemo. Cancer treatment changes how both partners sleep. It’s important to work together to find ways to sleep better.
Having Difficult Conversations About Space and Comfort
Talking about where to sleep can be tough. But, it’s crucial to share your feelings and needs. Partners should schedule regular check-ins to talk about how they’re doing and what changes might help.
It’s also important to think about the emotional side of sleeping together. Cancer patients often feel anxious or scared about their treatment. Their partner’s support can really help ease these feelings.
Respecting Changing Needs Throughout Treatment
Cancer treatment changes, and so do the patient’s needs. Being flexible is important when it comes to sleeping. Partners should be ready to change their approach as needed.
- Watch for changes in the patient’s condition and adjust sleeping plans.
- Be open to trying different sleeping setups to find what works best.
- Keep talking to make sure both partners are comfortable and supported.
Working as a Team to Find Solutions
Creating a sleeping plan that works for both partners takes teamwork. By working together and keeping communication open, couples can overcome the challenges of cancer treatment. They can find solutions that meet their needs.
Getting help from healthcare professionals is also a good idea. They can offer advice on managing chemo side effects and other cancer treatment aspects.
Supporting a Loved One Through Chemotherapy at Night
Supporting a loved one through chemotherapy at night needs understanding, patience, and smart strategies. Knowing the challenges they face helps you support them better.
Responding to Nighttime Side Effects
Chemotherapy can lead to side effects like nausea, pain, or discomfort at night. It’s important to be ready to handle these issues.
- Keep anti-nausea medication handy.
- Use relaxation techniques, such as deep breathing or meditation, to help alleviate anxiety.
- Ensure the room is at a comfortable temperature to help manage night sweats.
Creating Helpful Routines
Having a routine can bring comfort and stability to someone going through chemotherapy. Here are some ideas:
- Develop a calming pre-sleep routine, such as reading or listening to soothing music.
- Encourage your partner to stay hydrated throughout the day to reduce nighttime discomfort.
- Plan for rest periods during the day to help manage fatigue.
Creating a schedule together can make you both feel more in control and ready for chemotherapy’s challenges.
When to Seek Medical Help for Nighttime Issues
While many side effects can be managed at home, some need medical help. Know when to seek help for these signs:
| Symptom | Action |
| Severe pain or discomfort | Contact your healthcare provider for guidance. |
| Uncontrolled nausea or vomiting | Seek immediate medical attention. |
| Difficulty breathing or shortness of breath | Call emergency services or go to the emergency room. |
Being alert and proactive in managing side effects and knowing when to seek help can greatly improve your partner’s comfort and safety during chemotherapy.
Advice from Oncology Nurses on Sleeping Next to Chemo Patients
Caregivers and partners often ask oncology nurses for advice on caring for loved ones during chemotherapy. These nurses, with their vast experience, share important tips on safely sharing a bed with someone getting chemo.
Professional Recommendations for Home Care
Oncology nurses stress the need for good hygiene to avoid risks. They advise washing hands often, especially after touching bodily fluids. Also, clean any surfaces or bedding that might have come into contact with these fluids.
Key Hygiene Practices:
- Wash hands thoroughly with soap and water after using the bathroom, before eating, and after touching the patient or their bodily fluids.
- Use gloves when handling bodily fluids or contaminated items.
- Clean and disinfect surfaces and equipment regularly.
They also suggest knowing the patient’s treatment schedule and the types of chemotherapy drugs. This information helps determine the level of caution needed.
| Chemotherapy Drug Type | Precautions | Duration |
| High-Risk Chemotherapy | Avoid direct contact with bodily fluids; use protective gear. | Typically 24-48 hours post-treatment |
| Low-Risk Chemotherapy | Standard hygiene practices; minimal precautions. | Varies; consult healthcare team |
Questions to Ask Your Healthcare Team
It’s vital for caregivers and partners to talk openly with their healthcare team. Oncology nurses suggest making a list of questions. Some examples include:
- What are the specific risks associated with the patient’s current chemotherapy regimen?
- How long should precautions be taken after treatment?
- Are there any specific hygiene practices or precautions we should follow at home?
Resources for Caregivers and Partners
Oncology nurses also recommend looking for resources and support for caregivers. This can include online forums, support groups, and educational materials from reputable cancer organizations.
“Having access to reliable information and support can make a significant difference in the caregiving experience,” notes an oncology nurse.
For more guidance, many cancer centers offer workshops or counseling services for caregivers and partners.
Real-Life Experiences: How Couples Navigate Sleeping During Chemo
Chemotherapy can change a couple’s routine, including sleep. But, many couples show how they adapt and stay strong. They share how to keep intimacy alive while staying safe.
Case Studies and Personal Stories
Many couples have talked about sleeping with one partner getting chemo. For example, Sarah and Mike from New York. They used separate bedding and kept things clean to stay together safely.
Stories like Sarah and Mike’s show it’s possible to stay close during chemo. They teach us about the value of talking and being flexible.
Common Challenges and Solutions
Managing chemo side effects like night sweats and tiredness is a big challenge. But, couples have found ways. They use breathable bedding and calm bedtime routines to help.
| Challenge | Solution |
| Night Sweats | Breathable Bedding |
| Fatigue | Calming Bedtime Routine |
Lessons Learned from Cancer Survivors and Their Partners
Cancer survivors and their partners say emotional support is key during chemo. They point out that safety is important, but so is keeping emotional closeness.
Special Considerations for Different Types of Cancer Treatments
Cancer treatment includes many therapies, each with its own needs and lifestyle changes. It’s key to know how these treatments differ, especially in safety and daily life adjustments.
Radiation Therapy vs. Chemotherapy Considerations
Radiation therapy and chemotherapy are two main treatments. They work differently and have different safety concerns. Chemotherapy kills cancer cells all over the body. Radiation therapy targets specific cancer areas.
Chemotherapy can spread to others through body fluids. But, radiation therapy doesn’t usually pose a risk to others once it’s done.
| Treatment Type | Mode of Action | Safety Considerations |
| Chemotherapy | Systemic treatment using drugs | Potential exposure through bodily fluids |
| Radiation Therapy | Localized treatment using radiation | No risk to others after treatment completion |
Targeted Therapies and Immunotherapies
Targeted therapies and immunotherapies are more specific cancer treatments. Targeted therapies target cancer cell traits. Immunotherapies boost the body’s fight against cancer.
These treatments have different side effects and safety concerns than traditional chemotherapy. Some immunotherapies can cause immune-related side effects that need careful management.
Combination Treatments and Their Impact on Daily Life
Many patients get combination treatments, mixing chemotherapy, radiation, targeted therapy, or immunotherapy. It’s important to know how these treatments work together to manage side effects and adjust daily life.
Combination treatments can have complex effects on the body. They may need careful monitoring and adjusting daily routines to handle fatigue, side effects, and other challenges.
Understanding the unique aspects of different cancer treatments helps patients and caregivers face therapy challenges. It allows them to make informed decisions about their care.
Conclusion
As we wrap up our talk on sleeping next to a chemo patient, it’s clear that careful thought and safety steps are key. We’ve looked at how chemotherapy affects the body, the risks involved, and how to stay safe and supportive during treatment.
Our key points summary shows how important it is to know about chemotherapy’s effects, manage risks, and keep a safe and caring space. By following the advice in this article, people can handle the challenges of sleeping next to a chemo patient with confidence.
In the end, being cautious, talking openly, and showing kindness are vital in supporting loved ones through chemotherapy. We stress the need for ongoing talks between patients, caregivers, and doctors to get the best results.
FAQ
Is it safe to sleep next to someone undergoing chemotherapy?
It’s usually safe to sleep next to someone getting chemotherapy. But, it’s important to follow some safety steps. This includes keeping clean and handling fluids carefully.
How long after chemotherapy can I resume normal sleeping arrangements?
When you can go back to normal sleeping depends on the chemotherapy type and treatment plan. The biggest safety steps are during and right after treatment.
What are the risks of exposure to chemotherapy drugs through bodily fluids?
Chemotherapy drugs can be in urine, stool, and vomit. Not handling these safely can be risky. But, you can lower the risk by keeping clean.
Are there specific chemotherapy drugs that pose a higher risk when in close contact?
Yes, some chemotherapy drugs are more dangerous than others. They can harm through exposure. Your doctor can tell you about the risks of the drugs being used.
How can I protect myself from potential exposure when sleeping next to a chemo patient?
To stay safe, wash your hands often, especially after touching fluids. Wearing disposable gloves when needed can also help.
Can sleeping next to a chemo patient affect my immune system?
Sleeping next to a chemo patient doesn’t directly harm your immune system. But, it’s key to protect them from germs because their immunity is weak.
What are the signs of compromised immunity in a chemo patient?
Look out for fever, chills, a long cough, or infection signs at injection sites. Tell your doctor if you see these.
How can we maintain intimacy during chemotherapy treatment?
Keep intimacy alive by talking openly, being flexible, and finding safe ways to be close. Emotional connection is also important through shared moments and talks.
Are there special considerations for pregnant women or children when it comes to sleeping next to a chemo patient?
Pregnant women and kids need extra care because they’re more sensitive to chemotherapy. Always talk to a doctor for advice.
What bedding considerations and laundering practices are recommended for households with a chemo patient?
Use washable bedding and hot water to wash it after each treatment. Separate the patient’s laundry and use disposable items when you can.
When should we consider separate sleeping arrangements during chemotherapy?
You might need separate beds if the patient has bad side effects like night sweats or vomiting. Talk to your doctor for the best advice.
How can we create a restful environment for both the chemo patient and their partner?
Make a calm space by managing symptoms, reducing noise, and keeping it comfy for both. Use blackout curtains and keep the room at a good temperature.
What resources are available for caregivers and partners of chemo patients?
There are support groups, counseling, and educational materials from cancer groups and doctors. These can help you care for your loved one during treatment.
References
- National Cancer Institute. (2023). Chemotherapy and You: Support for People With Cancer. U.S. Department of Health and Human Services.https://www.cancer.gov/publications/patient-education/chemotherapy-and-you
- American Cancer Society. (2024). Chemotherapy Safety for Caregivers.https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/chemotherapy/caregiver-safety.html