Last Updated on November 18, 2025 by Ugurkan Demir
When the spine undergoes auto fusion of vertebrae, it can change how it moves and feels. This can affect our daily lives. Conditions like ankylosing spondylitis can cause spinal autofusion. This means vertebrae fuse together naturally, without surgery.
At Liv Hospital, we know how important it is to understand autofusion spine and its impact on spine health. This condition, where vertebrae fuse together, needs careful care and advanced treatments.
We aim to offer top-notch healthcare, supporting patients from around the world. In this article, we’ll look into the causes, effects, and treatments for spinal autofusion. We want to help patients find reliable care.
Autofusion is when the vertebrae in your spine naturally fuse together. This can happen for many reasons, like inflammatory diseases, injuries, or being stuck in one place for a long time.
The fusion of vertebrae happens slowly over time. It’s the body’s way of healing from injury or disease. Inflammatory conditions like ankylosing spondylitis can cause vertebrae to grow together.
When vertebrae fuse, they can become fully or partially joined. This can make your spine less flexible and less mobile. Knowing how autofusion works is key to finding the right treatment.
Normally, your spine has separate and mobile vertebrae. This lets you move and bend easily. But with autofusion, your spine becomes stiffer. This can make it harder to move and may lead to other problems.
The main difference is the loss of normal spinal motion. This can also cause more stress and wear on the areas around the fused vertebrae.
Several factors contribute to spinal autofusion. These include inflammatory conditions, traumatic injuries, and prolonged immobilization. Knowing these causes is key to managing the condition and its effects on the spine.
Inflammatory conditions, such as ankylosing spondylitis, are a major cause of spinal autofusion. Ankylosing spondylitis is a type of arthritis that mainly affects the spine. It can also involve other joints. This condition causes chronic inflammation, leading to vertebrae fusion over time. Ankylosing spondylitis can cause the spine to fully fuse, greatly affecting mobility and quality of life.
The body’s immune system attacks the spine in ankylosing spondylitis. This leads to pain, stiffness, and eventual fusion of the vertebrae. Early diagnosis and treatment can help manage symptoms and slow disease progression.
Traumatic injuries to the spine can also cause autofusion. The body’s natural healing response can lead to vertebrae fusion. The chance of autofusion after a traumatic injury depends on injury severity and overall health.
Common traumatic injuries that can lead to autofusion include:
These injuries can trigger inflammation, leading to bone deposition and potentially autofusion.
Prolonged immobilization can also cause spinal autofusion. This can be due to illness, injury, or surgery. Without normal motion and stress, the body may start bone remodeling. This process can result in vertebrae fusion over time.
Bone remodeling is a natural process for bone health. But, prolonged immobilization can lead to unwanted autofusion. Understanding bone remodeling’s role in autofusion helps in preventing or managing the condition.
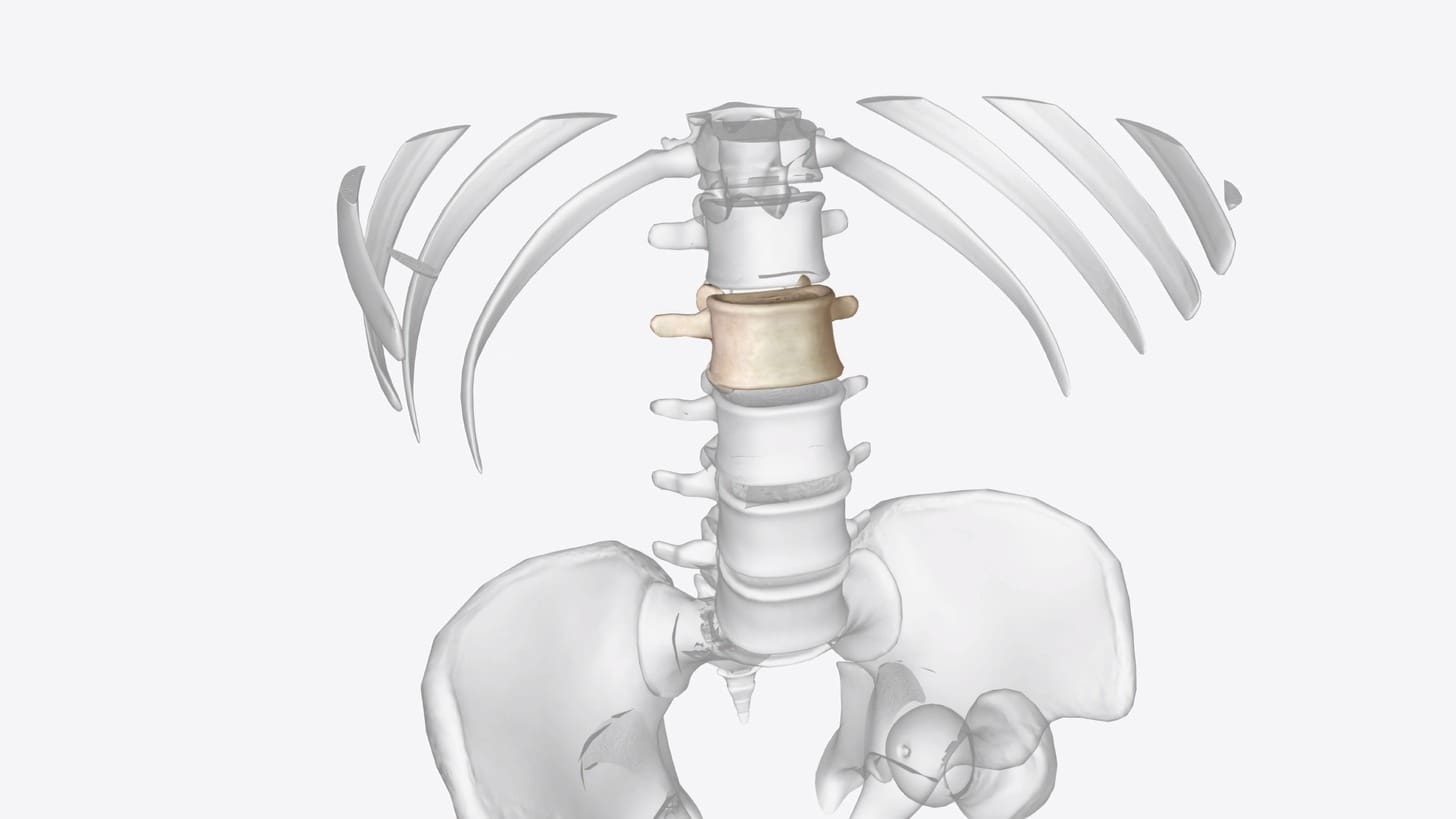
Autofusion can happen in the cervical, thoracic, or lumbar spine. Each area is affected differently by this condition.
Cervical autofusion is when vertebrae in the neck fuse naturally. This can make it hard to move your neck and may cause stiffness. It can also make simple tasks like turning your head or looking up more challenging.
The impact on neck mobility is significant. We need to think about how it might affect you in the long run, like the risk of more problems in other parts of your spine.
In the lower back, fused vertebrae can change how your body moves. This can affect your posture and how you walk. The lower back carries a lot of your body’s weight, so fusion here can lead to pain or discomfort.
It’s important to understand how fused vertebrae in the lower back work. This helps us manage what you can expect and plan the best treatment for you.
| Region | Common Effects of Autofusion | Potential Complications |
|---|---|---|
| Cervical | Reduced neck mobility, stiffness | Adjacent segment disease, limited range of motion |
| Lumbar | Altered biomechanics, postural changes | Lower back pain, gait disturbances |
| Thoracic | Potential impact on rib cage mobility, breathing | Respiratory issues, chronic pain |
Thoracic spine autofusion affects the rib cage area. This can impact how you breathe and move your rib cage. It’s a key area to watch for any breathing problems.
People with thoracic spine autofusion need close monitoring. This helps prevent or manage any breathing issues that might arise.
The auto fusion of vertebrae happens through bone growth and remodeling. These processes slowly join two vertebrae together. Scientists are working hard to understand this complex process.
Bone growth and remodeling are key for a healthy spine. In auto fusion, they help join vertebrae. Bone remodeling is a dance between cells that break down and build bone.
“The balance between breaking down and building bone is vital for the spine,” experts say. But in auto fusion, this balance is off, causing vertebrae to fuse abnormally.
The time it takes for vertebrae to fuse naturally varies. Many things can affect this, like the reason for fusion, inflammation, and injuries.
Knowing how auto fusion of vertebrae works is key to treating it. Healthcare providers can help patients more by understanding these mechanisms.
The symptoms of auto fusion of vertebrae can vary. They include pain patterns, mobility limitations, and postural changes. These symptoms can make daily activities hard.
Pain is a common symptom of autofusion. It often feels like chronic back pain that spreads to other areas. The pain gets worse with movement and better with rest.
Knowing how pain changes is key to managing it well.
As autofusion gets worse, it can really limit how you move. The extent of these limits depends on where and how much the spine fuses. For example, cervical autofusion can make it hard to move your neck.
Lumbar autofusion can make your lower back less flexible and mobile.
Postural changes are also common in autofusion. When vertebrae fuse, your spine becomes less flexible. This can cause your body to adopt an abnormal posture.
This can put strain on other parts of your body.
Living with autofusion means adapting to these changes. Understanding the symptoms is the first step to managing them. By recognizing how autofusion affects daily life, we can help people keep their quality of life.
Diagnosing spinal autofusion requires a mix of advanced imaging and a deep look into the patient’s history. We’ll explain how we do it, so patients know what’s happening.
Imaging is key in spotting spinal autofusion. We use different methods to see the spine and how much fusion has happened.
| Imaging Modality | Primary Use in Diagnosing Spinal Autofusion | Key Benefits |
|---|---|---|
| X-rays | First check of bone fusion | Fast, easy to get, and not too expensive |
| MRI | Looks at soft tissues and nerves | Clear images of soft tissues and nerves |
| CT scans | Close look at bones and fusion | Sharp bone images, great for planning surgery |
Imaging is just part of the story. We also look at the patient’s symptoms, medical history, and physical check-ups. This helps us understand how the condition affects them.
Our clinical assessment checks how well the patient moves, their pain, and any nerve problems. Looking at the patient’s history helps us find out what might have caused the condition, like old injuries or diseases.
By mixing imaging results with clinical findings and patient history, we can pinpoint spinal autofusion. Then, we can plan the best treatment.
When we talk about spinal fusion, we’re looking at two main options: autofusion and surgical spinal fusion. It’s important for both patients and doctors to know the differences. This helps in making the right choice for spinal health.
Autofusion happens naturally, without surgery, due to inflammation, injuries, or long periods of not moving. It can make vertebrae fuse together, making the spine stiffer. Surgical spinal fusion, on the other hand, uses rods, screws, and bone grafts to fuse vertebrae. The main difference is that surgery is more controlled and predictable than autofusion.
A spinal expert says, “Surgical fusion makes the spine stable right away, but autofusion takes longer and is less certain.” This shows why understanding the structural differences is key.
The results of autofusion and surgical spinal fusion can differ a lot. Autofusion might fuse naturally but can also cause uneven or incomplete fusions. This might lead to ongoing pain and mobility issues. Surgical fusion is more controlled but can also have downsides, like problems with other parts of the spine. It’s important to think about these points when deciding on spinal fusion.
Looking at the long-term effects of autofusion and surgical spinal fusion, we see different things. Autofusion can change over time, possibly leading to more fusion or problems like kyphosis. Surgical fusion is usually more reliable but can also have long-term issues, like hardware failure or problems with other spine segments. Knowing these possible outcomes is key for managing patient hopes and making the right treatment choices.
“The long-term success of spinal fusion, whether through autofusion or surgery, depends on a multitude of factors, including patient health, the underlying condition, and post-procedure care.”
In summary, both autofusion and surgical spinal fusion have their own benefits and risks. Understanding these differences helps doctors and patients make better choices for spinal fusion. This ensures decisions match individual needs and situations.
Naturally fused vertebrae need a special treatment plan. This plan must fit the person’s specific needs and how severe their condition is.
For naturally fused vertebrae, the first step is often conservative management. This method aims to manage pain and keep the spine moving without surgery. It includes pain meds, lifestyle changes, and therapies like acupuncture or chiropractic care.
Physical therapy is key in this approach. It helps improve flexibility and strengthens the muscles around the spine. A good physical therapy plan can keep the spine moving and reduce stiffness.
Physical therapy is essential for treating naturally fused vertebrae. Our therapists create a custom exercise plan. This plan includes stretching, strengthening, and aerobic exercises that fit the patient’s needs and limits.
Manual therapy, like massage and joint mobilization, can also help. It improves spinal mobility and reduces pain.
If conservative management doesn’t work, or if the fusion causes serious problems, surgical intervention might be needed. Surgery can include procedures to fix neurological issues or correct deformities.
Choosing surgery depends on the patient’s health, how severe their condition is, and their wishes. We make sure patients understand the risks and benefits of surgery.
Living with spine autofusion means making many changes to manage symptoms and keep a good quality of life. It’s key to know the lifestyle changes and precautions needed every day.
People with spine autofusion often have to change their daily routines a lot. Maintaining flexibility and strengthening the muscles around the spine are very important. Here are some tips:
Pain management is also a big part of daily life. It might include medicine, physical therapy, and things like acupuncture or mindfulness meditation.
One big worry with spine autofusion is adjacent segment disease. This is when the segments next to the fused area get stressed and might degenerate. To avoid this, we suggest:
Spine specialists say, “Early action and prevention can greatly improve life for those with spine autofusion.” By following these steps, people can manage their condition better and lower the chance of problems.
We know living with spine autofusion is tough, but with the right steps, people can live active and happy lives. Our goal is to give full care and support to help people deal with these challenges.
Research is growing, and we’re learning more about autofusion and spinal health. Studies are diving into the complex ways autofusion works. They’re uncovering its causes, effects, and possible treatments. This progress is key for helping patients with autofusion.
New studies have made big strides in understanding autofusion. Research has shown that inflammation, like in ankylosing spondylitis, can start autofusion in the spine. Also, genetics play a part in who gets autofusion. Knowing these details helps us find better treatments.
New ways to treat autofusion are being developed. Conservative management like physical therapy and lifestyle changes are getting better. Researchers are also looking into new medicines to slow down autofusion. These new treatments give hope for better living for those with autofusion.
The future of autofusion research looks bright. We’ll see big advances in diagnosis, treatment, and prevention. As we learn more, we’ll have more effective and tailored treatments.
Understanding auto fusion of vertebrae is key for managing its effects on spine health and overall well-being. This article has covered the complexities of spinal autofusion. We looked at its causes, symptoms, and treatment options.
Spinal autofusion, or naturally fused vertebrae, can greatly impact a person’s quality of life. Recognizing its signs and symptoms early can lead to better outcomes. This way, we can help improve lives.
As we learn more about auto fusion of vertebrae, we can find better ways to manage it. Our aim is to offer care that meets the specific needs of those with spinal autofusion.
Raising awareness about spinal autofusion and its effects is important. It helps us improve the lives of those dealing with this condition.
Auto fusion of vertebrae, also known as spinal autofusion, is when the vertebrae in the spine naturally fuse. This often happens due to inflammatory conditions, traumatic injuries, or being stuck in one position for a long time.
Autofusion can make the spine less flexible and stiffer. How much it affects you depends on where and how many vertebrae are involved.
Common causes include inflammatory conditions like ankylosing spondylitis, injuries, and being stuck in one position for a long time. These can make the body fuse vertebrae together, changing how the spine works.
Yes, it can happen in different parts of the spine, like the neck, middle back, and lower back. Each part affects the body differently.
Doctors use X-rays, CT scans, or MRI to diagnose autofusion. They also look at your medical history and do a physical check to see how it’s affecting you.
Treatment options include physical therapy and surgery. The choice depends on how bad your symptoms are and how much fusion has happened.
Autofusion and surgical spinal fusion both aim to stabilize the spine. But they differ in how they’re done and their effects on mobility and long-term health.
Yes, making changes in your daily life can help manage autofusion. This includes adjusting your activities and taking care of your spine’s health.
Bone remodeling is key in autofusion. It’s the body’s natural process of breaking down and building bone, leading to vertebrae fusing over time.
Yes, there’s ongoing research into new treatments for autofusion. These include new therapies and ways to improve rehabilitation for people with the condition.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!