Last Updated on November 27, 2025 by Bilal Hasdemir
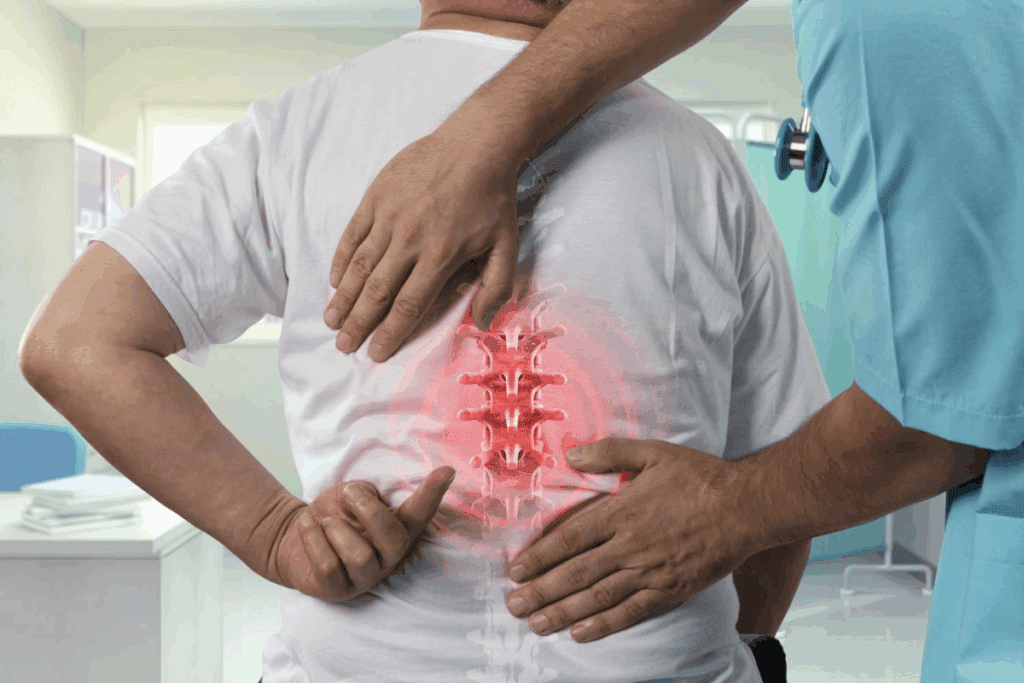
Going through spinal fusion surgery can be scary, mainly because of the pain. This surgery joins two or more vertebrae together. It means a long recovery time.
Patients looking for advanced medical care need all the info they can get. Spine surgery options differ, but spinal fusion surgery is known for being very painful. This is because it’s quite invasive and takes a long time to recover.
Key Takeaways
- Spinal fusion surgery is a complex and painful procedure.
- The recovery period for spinal fusion surgery is significant.
- Understanding spine surgery options is key for patients.
- Comprehensive support is vital for international patients seeking advanced medical treatments.
- Spinal fusion surgery involves joining two or more vertebrae together.
The Spectrum of Spinal Surgeries and Pain

Spinal surgeries cover a wide range of procedures, each with its own pain level. The pain can change a lot, depending on the surgery type, patient health, and care after surgery.
How Pain Varies Across Spinal Procedures
Different spinal surgeries have different pain levels. For example, lumbar fusion and cervical fusion have different pain levels. Lumbar fusion, which joins vertebrae in the lower back, can cause a lot of pain after surgery. Cervical fusion, done in the neck, might have a different pain level because of the delicate structures involved.
The pain can also change based on the surgery method. For instance, less invasive surgeries usually cause less pain than traditional open surgeries because they damage less tissue.
Factors That Influence Post-Surgical Pain
Many things can affect how much pain you feel after spinal surgery. These include:
- The type of surgical procedure performed
- The patient’s overall health and pre-existing medical conditions
- The surgical approach used (anterior vs. posterior, minimally invasive vs. open)
- Post-operative care and pain management strategies
Knowing these factors is key to managing your expectations and getting ready for recovery. As one expert says, “Pain after spinal surgery is complex, depending on many factors, including the patient’s mental state and the surgery method.”
“The key to successful pain management lies in a complete approach that meets each patient’s unique needs.”
| Factor | Influence on Pain |
| Type of Surgery | Different surgeries have different pain profiles (e.g., lumbar fusion vs. cervical fusion) |
| Patient Health | Pre-existing conditions can affect pain perception and recovery |
| Surgical Approach | Minimally invasive surgeries generally result in less pain than open surgeries |
Common Spinal Surgeries and Their Pain Profiles
Knowing about the pain from common spinal surgeries helps patients get ready for recovery. Spinal surgeries treat different spine issues. Each surgery has its own pain levels after the operation.
Discectomy and Microdiscectomy
Discectomy and microdiscectomy relieve pressure on nerves from herniated discs. These surgeries usually have less pain after than more complex surgeries. The posterior approach is often used.
Laminectomy and Decompression
Laminectomy removes part or all of the lamina to ease pressure on the spinal cord or nerves. Decompression surgery is often done with laminectomy to reduce pressure more. The surgery’s extent and pedicle screws use can affect pain levels.
Foraminotomy
Foraminotomy enlarges the neural foramen to ease nerve pressure. It’s less invasive than spinal fusion and might have less pain after. The anterior or posterior approach can change the pain experience.
Artificial Disc Replacement
Artificial disc replacement puts an artificial disc in place of a damaged one, aiming to keep spinal mobility. It has a different pain profile than spinal fusion, possibly less pain for some.
The pain levels of these surgeries are shown in the table below:
| Surgery Type | Typical Post-Operative Pain Level | Surgical Approach |
| Discectomy/Microdiscectomy | Moderate | Posterior |
| Laminectomy/Decompression | Moderate to High | Posterior |
| Foraminotomy | Moderate | Anterior or Posterior |
| Artificial Disc Replacement | Moderate | Anterior |
Knowing these pain levels helps patients and doctors choose the best surgery.
Spinal Fusion Surgery: The Most Painful Option
Spinal fusion surgery is known for being very painful. It involves joining vertebrae together using bone grafts and metal rods. This surgery is used to stabilize the spine and relieve pain from different spinal conditions.
What Makes Fusion Uniquely Painful
Several factors make spinal fusion surgery painful. The surgery requires a big incision in the back, causing tissue damage and pain. The use of bone grafts and metal rods also irritates and inflames, adding to the pain.
The fusion process itself is painful. The bone graft material used can be uncomfortable as it heals. Also, the fused segment’s immobilization can put stress on other parts of the spine, leading to more pain.
Clinical Studies on Pain Severity
Many studies have looked into the pain from spinal fusion surgery. They show that patients often feel a lot of pain right after surgery. A study in the Journal of Neurosurgery: Spine found that pain levels were high in the first weeks but got better as the fusion healed.
Another study found that better hardware and techniques have helped, but pain is a big issue. This shows how important it is to manage pain well after surgery.
Patient-Reported Pain Metrics
Patients’ own reports of pain give us a good idea of what they go through. Many say they feel moderate to severe pain at first, but it gets better over time. Things like pre-existing pain, how much of the spine is fused, and how sensitive someone is to pain all play a role in how much pain they feel.
Knowing these things helps doctors create better pain management plans. This can make patients happier and more satisfied with their care.
Understanding the Spinal Fusion Procedure
Spinal fusion surgery is a complex treatment. It joins two or more vertebrae to stabilize the spine and ease pain.
Vertebral Fusion Process
The vertebral fusion process is key in spinal fusion surgery. It prepares the vertebrae for fusion by removing damaged discs. Then, bone grafts are used to grow new bone between the vertebrae.
Advanced imaging helps place bone grafts accurately. The success of this process depends on the patient’s health, the bone graft quality, and the surgery’s precision.
Bone Graft and Hardware Components
Bone grafts are vital in spinal fusion surgery. They can come from the patient (autograft) or a donor (allograft). The graft helps new bone grow, fusing the vertebrae. Sometimes, rods, screws, and cages are used for extra spine support.
The choice of graft and hardware depends on the patient’s condition and health. We carefully select materials and techniques for each patient’s surgery.
Surgical Duration and Its Impact on Pain
The length of spinal fusion surgery varies. Longer surgeries can cause more pain due to tissue trauma. We use advanced techniques and patient positioning to reduce surgery time and pain.
Managing pain after surgery is important. We create a pain management plan for each patient. This may include medication, physical therapy, and other interventions to help with recovery.
Lumbar Fusion Surgery Pain Considerations
It’s important for patients to know about the pain from lumbar fusion surgery. This surgery joins two or more vertebrae in the lower back. It’s often needed for spondylolisthesis and sciatica.
Challenges in Lower Back Fusion
Lower back fusion is complex due to the spine’s anatomy. It can lead to a lot of pain after surgery. The surgery needs careful planning to avoid problems and get good results.
The lower back is under a lot of stress and strain. This can affect how well the fusion works and how long it takes to recover. Things like the patient’s health, any other health issues, and the surgery method can change how much pain they feel.
Pain Differences in TLIF, PLIF, and ALIF Surgical Approaches
The way the surgery is done can change how much pain you’ll feel after. There are three main methods: Transforaminal Lumbar Interbody Fusion (TLIF), Posterior Lumbar Interbody Fusion (PLIF), and Anterior Lumbar Interbody Fusion (ALIF).
| Surgical Approach | Description | Typical Pain Level |
| TLIF | Transforaminal Lumbar Interbody Fusion involves accessing the spine through the foramen. | Moderate |
| PLIF | Posterior Lumbar Interbody Fusion involves accessing the spine from the back. | Moderate to High |
| ALIF | Anterior Lumbar Interbody Fusion involves accessing the spine from the front. | High |
Recovery Timeline and Pain Progression
The time it takes to recover from lumbar fusion surgery varies. Pain usually gets better as the spine heals. Knowing what to expect can help manage your hopes.
Right after surgery, patients often feel a lot of pain. This is managed with medicine. As time goes on, the pain usually gets less, but some discomfort may stay for months.
Understanding the pain and how it changes can help patients prepare for their surgery and recovery.
Cervical Fusion Surgery Pain Profile
Cervical fusion surgery is a complex procedure for neck conditions. It’s important for patients to know about its pain profile. This surgery joins two or more vertebrae in the neck to treat issues like herniated discs or spinal stenosis.
Neck Fusion Pain Characteristics
The pain from cervical fusion surgery varies among patients. People often feel pain in their neck, which can spread to shoulders or arms. The pain’s intensity can be mild or severe, depending on the patient’s health and the surgery method.
Several factors can affect the pain, such as the number of vertebrae fused and the patient’s condition before surgery. Effective pain management is key in the recovery to ensure comfort and a smooth healing process.
ACDF vs. Posterior Cervical Fusion Pain
There are two main cervical fusion surgeries: Anterior Cervical Discectomy and Fusion (ACDF) and posterior cervical fusion. ACDF is done from the front of the neck, while posterior cervical fusion is from the back.
Both methods can be effective, but they have different pain effects. ACDF might cause dysphagia (swallowing difficulties) and voice changes. Posterior cervical fusion might lead to neck and upper back pain and stiffness.
Swallowing and Breathing Complications
Swallowing and breathing problems are possible complications, mainly with the anterior approach. These issues come from the surgery’s closeness to the esophagus and trachea.
While these complications are rare, they can be serious. Patients are watched closely for any signs of swallowing or breathing trouble after surgery. Rehabilitation and physical therapy are vital for recovery and managing any complications.
In summary, knowing about the pain from cervical fusion surgery is key for patients. Understanding the pain characteristics and the differences in surgical approaches helps patients prepare for recovery.
Surgical Approaches and Their Impact on Pain
The choice of surgical approach is key in how much pain patients feel after spinal surgery. Different methods can change how much pain and for how long. It’s important for both patients and doctors to know these differences.
Anterior vs. Posterior Approaches
The direction of the surgery can greatly affect recovery and pain.
- Anterior Approach: This method goes through the front of the body. It might be less painful for some because it doesn’t hurt as many back muscles.
- Posterior Approach: This method goes through the back. It’s more traditional but can cause more muscle damage and pain.
Minimally Invasive vs. Open Spine Surgery
Whether the surgery is minimally invasive or open also affects pain.
- Minimally Invasive Surgery: This uses smaller cuts and less damage to tissues. It can lead to less pain and a faster recovery.
- Open Spine Surgery: This needs a bigger cut, causing more tissue damage. It might lead to more pain during healing.
Medical Conditions Requiring Spinal Fusion
Many medical conditions can make spinal fusion surgery necessary. This surgery aims to stabilize the spine and ease pain. It’s often chosen when other treatments don’t work and the condition is severe.
Degenerative Disc Disease
Degenerative disc disease happens when discs in the spine lose height and strength. This leads to pain and instability. It’s a common reason for spinal fusion, as it can greatly affect daily life.
Spondylolisthesis
Spondylolisthesis is when a vertebra slips forward over another. This can cause nerve compression and pain. Spinal fusion helps stabilize the vertebrae and stops further slippage.
Spinal Stenosis
Spinal stenosis narrows the spinal canal. This puts pressure on the spinal cord and nerves, causing pain, numbness, and weakness. In severe cases, spinal fusion is needed to relieve this pressure and stabilize the spine.
Fractures and Trauma
Spinal fractures or injuries also require spinal fusion. The surgery stabilizes the spine, allowing the bones to heal. It reduces the risk of further injury or deformity.
It’s important for patients to understand why spinal fusion surgery is recommended. Each condition poses unique challenges. Spinal fusion can be an effective way to manage pain and improve life quality.
| Condition | Description | Role of Spinal Fusion |
| Degenerative Disc Disease | Loss of disc height and integrity | Stabilize the spine, alleviate pain |
| Spondylolisthesis | Vertebra slips over the one below | Prevent further slippage, stabilize |
| Spinal Stenosis | Narrowing of the spinal canal | Relieve pressure on nerves, stabilize |
| Fractures and Trauma | Spinal fractures or injuries | Stabilize the spine, facilitate healing |
Immediate Post-Operative Pain Management
The time right after surgery is key for managing pain. It’s important for comfort and healing. Good pain control helps patients feel better and can prevent problems.
Hospital Pain Control Protocols
Hospitals have special plans for pain management right after surgery. These plans involve many healthcare professionals. They aim to reduce pain and keep patients safe.
A study in the Journal of Pain Research shows that following these plans helps. Standardized protocols mean all patients get the same care. This leads to better pain control and happier patients.
Pain is a complex phenomenon that requires a multifaceted treatment approach. By implementing standardized pain management protocols, hospitals can improve patient outcomes and reduce the risk of complications.
Medication Strategies
Medicine is a big part of managing pain after surgery. The right medicine depends on the surgery and the patient. Doctors often mix different medicines to help with pain.
| Medication Type | Examples | Primary Use |
| Opioids | Morphine, Fentanyl | Severe pain management |
| NSAIDs | Ibuprofen, Ketorolac | Moderate pain, anti-inflammatory |
| Acetaminophen | Tylenol | Mild to moderate pain, fever reduction |
Patient-Controlled Analgesia
Patient-Controlled Analgesia (PCA) lets patients give themselves medicine for pain. It helps control pain better and can use less medicine. PCA is great for severe pain after surgery.
A study in the Journal of Clinical Anesthesia shows PCA works well. Patient empowerment through PCA can lead to better results.
Regional Anesthesia Options
Regional anesthesia numbs a certain area of the body. It’s used in spinal surgery to manage pain. It’s a good choice because it doesn’t have the side effects of opioids.
- Epidural anesthesia: Involves injecting medication into the epidural space surrounding the spinal cord.
- Peripheral nerve blocks: Involve injecting local anesthetic around specific nerves to block pain signals.
Using these strategies, hospitals can improve care and results. Effective pain control is key for a smooth recovery and happy patients.
Long-Term Pain After Spinal Fusion
Some people may feel long-term pain after spinal fusion. This can be a big worry for those thinking about or who have had the surgery.
Failed Back Surgery Syndrome
Failed Back Surgery Syndrome (FBSS) is when people keep feeling pain after spinal surgery. It’s a complex condition caused by many things like not fully healing, hardware problems, or nerve damage. It can really affect someone’s life, so we need to tackle it in a big way.
Adjacent Segment Disease
Adjacent Segment Disease (ASD) is another pain problem after spinal fusion. It happens when the parts of the spine next to the fusion site start to wear out or become unstable. Early detection and intervention are key to dealing with ASD and lessening its effects on a person’s life.
Hardware-Related Pain Issues
Pain from the hardware used in spinal fusion can be a problem. This might be because the hardware doesn’t work right, is put in wrong, or the body reacts to it. We stress the need for choosing the right hardware and doing the surgery carefully to avoid these issues.
Chronic Pain Management Approaches
Dealing with chronic pain after spinal fusion needs a mix of treatments. We suggest using medicine, physical therapy, and changing lifestyle habits to help manage pain. Personalized care plans are vital to meet each patient’s specific needs.
Understanding why long-term pain happens after spinal fusion and using good management strategies can help patients. Our goal is to give full care that covers both the physical and emotional sides of getting better.
Complications That Increase Pain Levels
Spinal fusion surgery can lead to complications that raise pain levels. While it’s often effective, knowing about these issues helps manage pain better.
Infection and Inflammatory Responses
Infection is a serious issue after spinal fusion surgery. It causes pain, swelling, and redness at the site. We prevent it with antibiotics and a clean surgery area.
Hardware Failure or Malposition
Hardware failure or wrong placement can cause a lot of pain. It might need more surgery to fix. The hardware is meant to stabilize the spine but can fail or be placed wrong.
Nerve Damage and Neuropathic Pain
Nerve damage can lead to pain, numbness, or weakness. This pain is hard to manage and might need special treatment. This includes medicine and physical therapy.
Pseudarthrosis (Failed Fusion)
Pseudarthrosis means the bone didn’t fuse as hoped. It causes ongoing pain and might need more surgery. Smoking, certain health issues, and not staying immobile enough can cause it.
Knowing about these complications helps us take steps to avoid them. Working with your healthcare team can help you recover better and avoid these issues.
Rehabilitation and Physical Therapy Impact on Pain
Rehabilitation and physical therapy are key to reducing pain after spinal fusion. We know recovery is more than just surgery. It’s also about the care and therapy that come after.
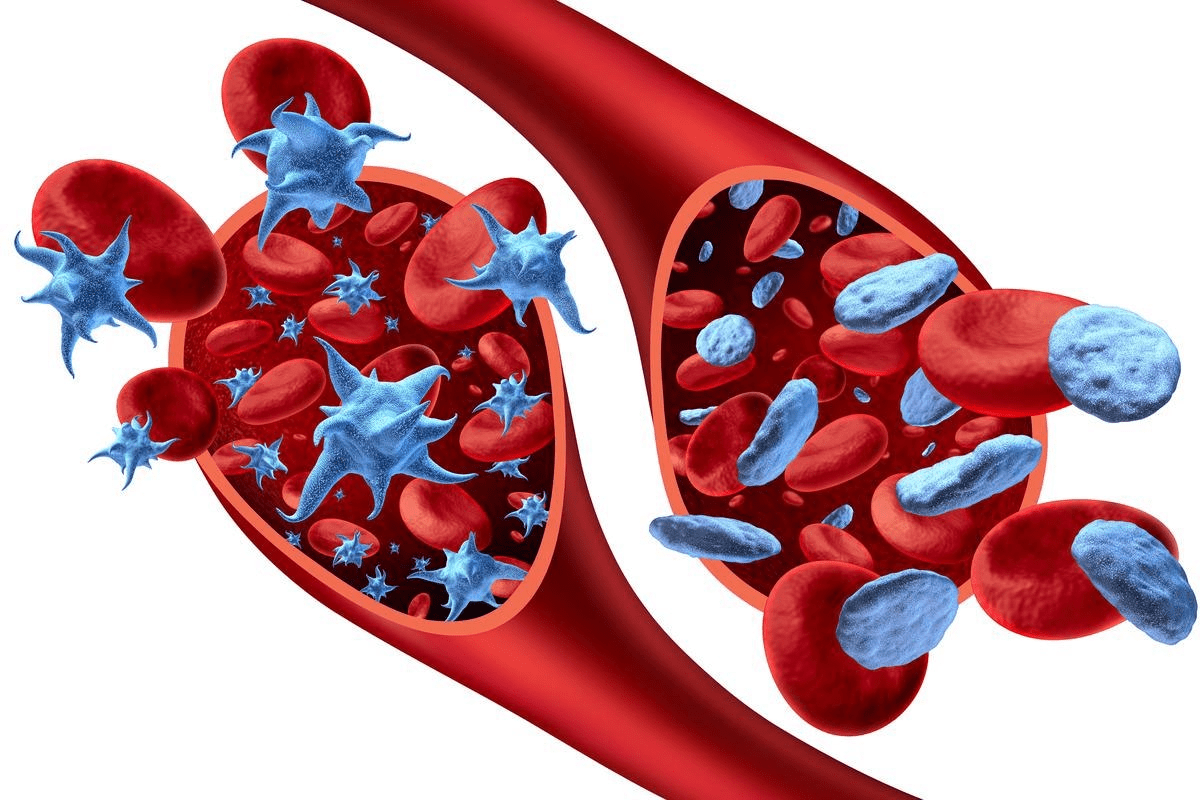
Benefits of Early Mobilization
Moving early after spinal fusion surgery is vital for a good recovery. It helps avoid blood clots, aids in healing, and reduces stiffness. Patients who move early tend to have better outcomes and less pain. We guide our patients with gentle exercises and gradual movement.
Structured Physical Therapy Protocols
Our physical therapy plans are made just for each patient. Our therapists work with patients to create a plan that meets their needs and goals. This includes exercises for back strength, flexibility, and posture.
“Physical therapy is not just about exercising; it’s about regaining function and reducing pain in a way that’s tailored to the individual’s needs and capabilities.”
Pain Reduction Through Proper Body Mechanics
Learning proper body mechanics is key to less pain after spinal fusion. Patients learn how to move, lift, and keep good posture. By doing this, patients can greatly reduce their pain and improve their life quality.
Long-Term Exercise Recommendations
For lasting success, patients should keep up with exercises that strengthen their back and improve flexibility. Low-impact activities like walking, swimming, or cycling are recommended because they’re easy on the spine but keep it strong and mobile. We teach patients how to fit these activities into their daily lives for ongoing benefits.
By focusing on rehabilitation and physical therapy, we help patients live a more comfortable and active life after spinal fusion. Our aim is to support patients through every step of their recovery. We give them the tools and knowledge to manage their pain well.
Alternatives to Spinal Fusion Surgery
Looking into alternatives to spinal fusion surgery can open up more treatment choices. Not every patient needs this surgery. We’ll look at other treatments, from non-surgical options to new technologies.
Conservative Treatment Options
First, we try non-surgical treatments for spinal issues. These include:
- Physical therapy to improve mobility and strength
- Medications like NSAIDs or muscle relaxants for pain and inflammation
- Lifestyle changes, such as losing weight or quitting smoking
- Epidural steroid injections to reduce nerve inflammation
These methods can help manage symptoms and might avoid the need for surgery.
Pain Management Interventions
For those with chronic pain, there are special treatments. These include:
- Nerve blocks and radiofrequency ablation to stop pain signals
- Spinal cord stimulation for long-term pain relief
- Intraspinal drug delivery systems for targeted pain relief
These options are great for those who can’t have surgery or want to avoid it.
Less Invasive Surgical Alternatives
For some, less invasive surgeries are better than spinal fusion. These include:
- Microdiscectomy or endoscopic discectomy for herniated discs
- Laminectomy or laminotomy to relieve nerve pressure
- Interspinous process decompression devices to increase space between vertebrae
These surgeries cause less damage and lead to faster recovery times than traditional spinal fusion.
Emerging Technologies and Procedures
Spinal surgery is always getting better, with new technologies and procedures. Some new options are:
- Artificial disc replacement surgery
- Minimally invasive spinal stabilization techniques
- Biologic treatments to help the spine heal
These new methods offer hope for better outcomes than traditional spinal fusion for some patients.
In summary, while spinal fusion is a common treatment, there are many alternatives. Patients should talk to their doctors to find the best treatment for their needs.
Preparing for Spinal Fusion Pain
Getting ready for spinal fusion surgery is key. It helps you face the challenges and recover well. Understanding what’s needed for a good outcome is important.
Mental and Psychological Preparation
Mental and psychological prep is as vital as physical prep. Those mentally ready tend to have a better outlook and coping skills during recovery. Try stress-reducing activities like meditation or yoga to calm your mind.
Cognitive behavioral therapy (CBT) helps with psychological issues. It helps you manage pain, anxiety, and other recovery challenges.
Physical Conditioning Before Surgery
Getting fit before surgery helps your recovery. Regular exercise, like walking or swimming, boosts your health and strength. Talk to your doctor about safe exercises for your condition.
Also, quitting smoking and cutting down on alcohol helps your body heal better. It lowers the risk of surgery complications.
Setting Realistic Expectations
Having realistic hopes for your surgery and recovery is key. Knowing what to expect helps you mentally and emotionally prepare. Talk to your surgeon and healthcare team about your hopes.
- Learn about the surgery and what it means
- Understand the recovery timeline and key points
- Discuss pain management options and plans
Home Preparation for Recovery
Preparing your home for recovery is important. Make your home safe and comfy for recovery. Remove hazards, set up a cozy area, and keep essentials close.
Having a support system is also key. Get family or friends to help with daily tasks. This reduces stress and lets you focus on healing.
When to Contact Your Surgeon About Pain
Knowing when to reach out to your surgeon about pain is key to good care after surgery. After spinal fusion, some pain is normal as you heal. But, it’s important to tell the difference between normal and abnormal pain to catch problems early.
Normal vs. Abnormal Pain Patterns
Normal pain after spinal fusion surgery usually gets better as you heal. But, abnormal pain is different. It can be very bad, last a long time, or get worse. Keep an eye on your pain and notice any changes or odd feelings.
Warning Signs of Complications
Some symptoms mean you need to see your surgeon right away. These include:
- Increasing pain that doesn’t get better with medicine
- Numbness, tingling, or weakness in your limbs
- Signs of infection, like fever, redness, or swelling
- Hard time controlling your bowel or bladder
Emergency Symptoms Requiring Immediate Attention
If you have severe symptoms, like sudden bad pain, trouble breathing, or signs of serious infection, get help fast. These could mean serious problems that need quick action.
Follow-up Schedule and Pain Reporting
Going to your follow-up appointments is important. We check how you’re doing, adjust your pain meds, and answer any questions. It helps us make sure you’re recovering well.
| Follow-up Visit | Typical Timeline | Pain Assessment |
| First Follow-up | 1-2 weeks post-op | Review initial recovery, adjust pain meds |
| Second Follow-up | 6-8 weeks post-op | Assess healing progress, adjust activities |
| Final Follow-up | 3-6 months post-op | Evaluate long-term recovery, address concerns |
By knowing the difference between normal and abnormal pain and when to talk to your surgeon, you can have a safer and smoother recovery.
Conclusion: Making Informed Decisions About Spinal Surgery
It’s key for patients to know what they’re getting into with spinal surgery. Understanding the surgery and recovery helps them prepare. This way, they can face the challenges and benefits with confidence.
We’ve looked at the many sides of spinal surgery. This includes the types of surgeries, risks, and benefits. Knowing these details helps patients make smart choices. It also means they can move through the healthcare system smoothly.
Being well-informed about treatment options leads to better results. When thinking about your options, talk to your doctor. This ensures you’re making the right choice for your health.
FAQ
What is spinal fusion surgery?
Spinal fusion surgery joins two or more vertebrae together. It uses bone grafts and metal rods to stabilize the spine. This helps to relieve chronic back pain.
How painful is spinal fusion surgery?
Spinal fusion surgery is quite painful. This is because of the surgery’s extent and the recovery period. Pain levels can vary based on the surgical approach and the patient’s health.
What are the common medical conditions that require spinal fusion surgery?
This surgery treats conditions causing spinal instability or chronic back pain. These include degenerative disc disease, spondylolisthesis, spinal stenosis, and fractures or trauma.
What are the differences between various surgical approaches for spinal fusion?
The surgical approach affects the pain experienced by patients. Anterior and posterior approaches have different pain levels. Minimally invasive surgery may cause less pain than open spine surgery.
How is pain managed after spinal fusion surgery?
Pain management involves several steps. These include hospital pain control, medication, patient-controlled analgesia, and regional anesthesia. These methods help reduce post-operative pain.
What are the possible complications of spinal fusion surgery?
Complications include infection, hardware failure, nerve damage, and pseudarthrosis. These can increase pain and affect the surgery’s outcome.
How can patients prepare for spinal fusion surgery to minimize pain?
Patients can prepare by mentally and physically preparing. They should set realistic expectations and prepare their home for recovery. This helps to reduce post-operative pain.
What are the alternatives to spinal fusion surgery?
Alternatives include conservative treatments, pain management, and less invasive surgeries. New technologies and procedures also offer treatment options.
When should patients contact their surgeon about pain after spinal fusion surgery?
Contact your surgeon for abnormal pain, warning signs of complications, or emergency symptoms. Follow the recommended follow-up schedule and pain reporting guidelines.
What is the role of rehabilitation and physical therapy in pain management after spinal fusion surgery?
Rehabilitation and physical therapy are key in pain management. Early mobilization and structured physical therapy help reduce pain. They promote recovery by teaching proper body mechanics.
References
- lshammari, H. S. (2023). Prevalence of chronic pain after spinal surgery: A systematic review and meta-analysis. Pain Research & Management, 2023, Article ID 4566790. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10423077/