Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know that nearly 250,000 adults in the United States are diagnosed with spinal stenosis each year? Many of them need surgery to feel better.
Spinal stenosis makes the spine’s spaces narrow. This puts pressure on nerves, causing pain and trouble moving. If other treatments don’t help, surgery is a good choice. It can change lives by making it easier to move and less painful.
Our medical team is here to help you fully. We make sure you get the best care for your condition. There are many surgery options, and we pick the best one for you.
Key Takeaways
- Spinal stenosis affects a significant number of adults in the US annually.
- Surgery is considered when conservative treatments fail.
- Various surgical options are available for treating spinal stenosis.
- Personalized care is crucial for effective treatment.
- Surgical intervention can significantly improve quality of life.
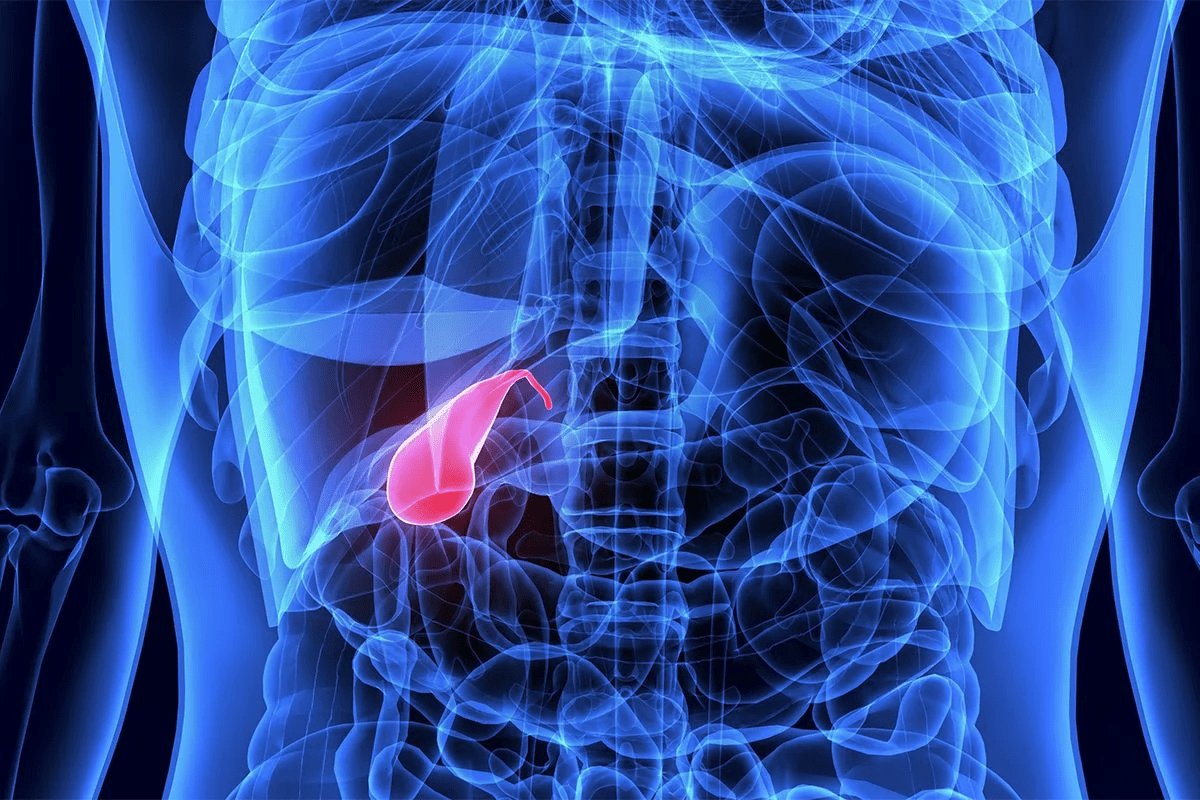
Understanding Spinal Stenosis
Spinal stenosis is a condition where the spaces in the spine narrow. This can put pressure on nerves, causing pain and limited movement.
Definition and Pathophysiology
Spinal stenosis happens when the spine’s spaces narrow, pressing on nerves. The Medical organization says it can be caused by aging, herniated discs, and injuries. It can affect different parts of the spine.
The condition involves degenerative changes, congenital factors, and sometimes injuries. As we get older, our spines naturally change, leading to stenosis. These changes include bulging discs and bone spurs, narrowing the spinal canal.
Common Causes of Spinal Stenosis
Several factors lead to spinal stenosis. Some common causes are:
- Age-related wear and tear: Aging causes degenerative changes in the spine.
- Herniated discs: Bulging discs can compress nerves.
- Spinal injuries: Traumatic injuries can cause or worsen stenosis.
- Congenital conditions: Some are born with conditions that affect the spine.
Knowing these causes helps doctors diagnose and treat spinal stenosis. They can then create treatment plans to help patients feel better.
Types of Spinal Stenosis
It’s important to know the different types of spinal stenosis for proper treatment. Each part of the spine has its own type, with unique symptoms and treatments.
Cervical Spinal Stenosis
Cervical spinal stenosis happens in the neck. It can press on the spinal cord, causing numbness, weakness, or tingling in the arms or legs. Early diagnosis is critical to avoid lasting damage.
Lumbar Spinal Stenosis
Lumbar spinal stenosis is in the lower back. It’s the most common and can cause lower back pain, numbness, or leg cramps. Conservative treatment options are tried first, before surgery.
Thoracic Spinal Stenosis
Thoracic spinal stenosis is rare and in the mid-back. It can lead to chest or abdomen pain, and in severe cases, affect bladder or bowel function. Prompt medical attention is needed for severe symptoms.
Every type of spinal stenosis needs a specific treatment plan. Healthcare providers must understand each patient’s condition to create an effective treatment.
Getting the right diagnosis and treatment can greatly improve life for those with spinal stenosis. We’ll look at symptoms and how to diagnose them next.
Symptoms and Diagnosis
A detailed medical illustration showcasing the key symptoms of spinal stenosis. In the foreground, a cross-section of the spinal column reveals a narrowed spinal canal, compressing the spinal cord and nerve roots. Middle ground depicts a person experiencing radiating leg pain, numbness, and weakness – classic symptoms of this condition. The background features a clean, clinical environment with subtle anatomical overlays, highlighting the affected vertebrae and nerve pathways. Lit by soft, directional lighting to emphasize depth and volume, this image conveys the technical nature of the subject while also conveying the patient’s physical experience in a clear, informative manner.
Spinal stenosis can really affect your daily life. It’s when the spinal canal gets narrower. This can cause many symptoms that make life harder.
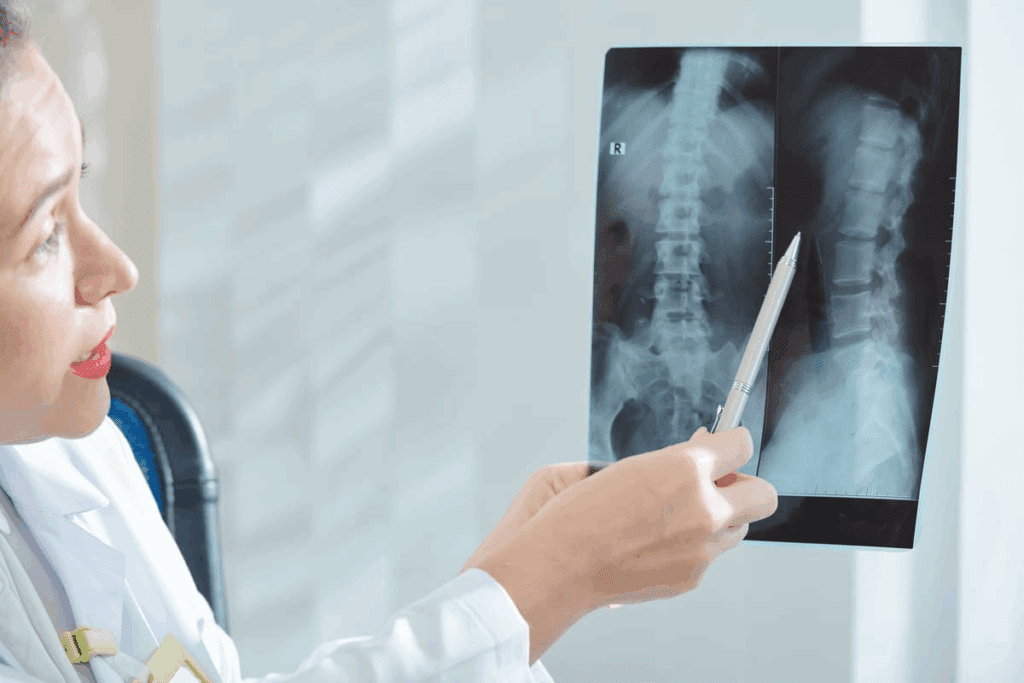
Diagnostic Procedures
To diagnose spinal stenosis, doctors use physical exams, medical history, and imaging tests. They check muscle strength, reflexes, and how you feel sensations to see if nerves are damaged.
Tests like MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans help see the spinal canal. MRI shows soft tissues well, while CT scans are good for bones. These tests help find where the canal is narrowing.
“Accurate diagnosis is the cornerstone of effective treatment for spinal stenosis. By combining clinical evaluation with advanced imaging techniques, healthcare providers can develop a comprehensive understanding of the condition and tailor treatment accordingly.”
Differential Diagnosis
It’s important to rule out other conditions that might cause similar symptoms. This includes diseases like peripheral artery disease or diabetic neuropathy. A detailed diagnostic process helps make sure patients get the right treatment.
By knowing the symptoms and using different tests, doctors can diagnose and treat spinal stenosis well. This improves patients’ lives and outcomes.
Non-Surgical Treatment Options
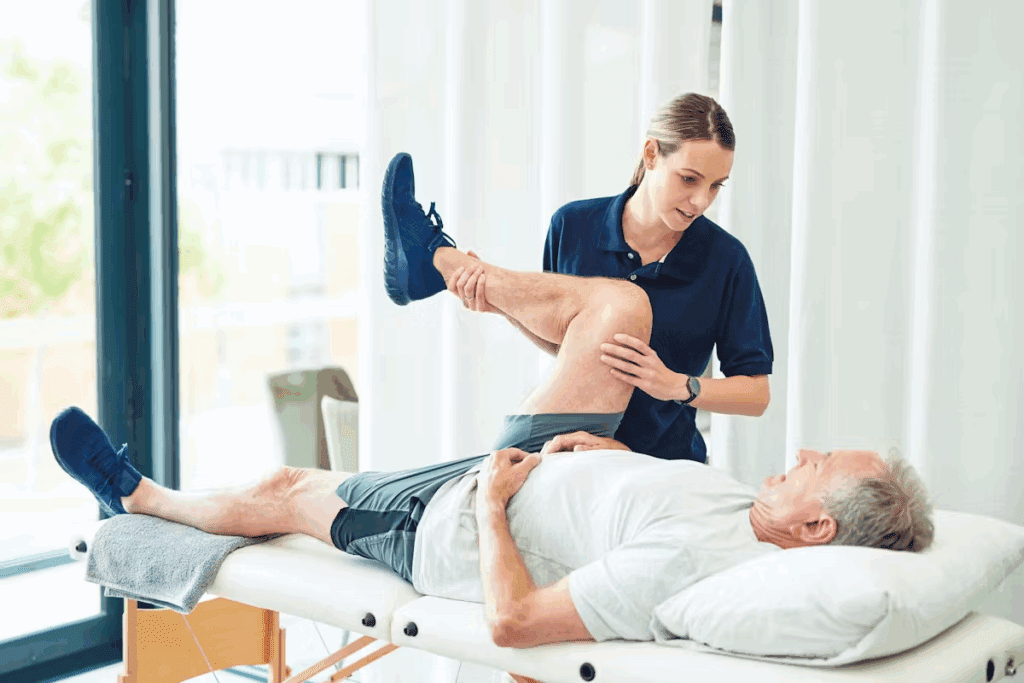
A physical therapist carefully guiding a patient through a series of targeted exercises to alleviate the symptoms of spinal stenosis. The patient is seated on a padded treatment table, surrounded by a bright, clean and welcoming clinic environment. Warm, diffused lighting illuminates the scene, creating a sense of calm and focused attention. The therapist’s hands gently demonstrate proper movement and posture, with an expression of empathy and expertise. The patient’s face reflects a mix of effort and relief, as they engage in the rehabilitation process. The overall mood is one of collaborative care, with a focus on restoring function and quality of life through non-surgical means.
Non-surgical treatments are key in managing spinal stenosis. They help improve life quality. These treatments are often the first step in treating the condition and can offer a lot of relief.
Medications for Symptom Management
Medications are a big part of non-surgical treatment plans for spinal stenosis. We use different medicines to manage pain and inflammation. This includes over-the-counter pain relievers, oral steroids, and medicines for nerve pain. Effective pain management is key to improving life quality and helping with physical therapy.
For example, NSAIDs like ibuprofen are used to reduce inflammation and pain. In severe cases, gabapentin or pregabalin may be given to treat nerve pain.
Physical Therapy Approaches
Physical therapy is a key part of non-surgical treatment for spinal stenosis. A tailored physical therapy program can improve mobility and strengthen muscles. Physical therapists use exercises, manual therapy, and teach about posture and body mechanics.
Our physical therapists create a personalized exercise program for each patient. This includes exercises for core strength, flexibility, and spinal alignment.
Steroid Injections and Nerve Blocks
Steroid injections and nerve blocks are options for extra pain relief. Steroid injections reduce swelling and relieve nerve pressure. Nerve blocks interrupt pain signals by injecting local anesthetics or steroids around nerves.
These injections are done under fluoroscopic guidance for accuracy. While they offer relief, they are used carefully due to steroid side effects.
When Surgery Becomes Necessary
A meticulously detailed surgical scene depicting a spinal stenosis treatment procedure. In the foreground, the patient’s exposed back lies under bright surgical lighting, with skilled hands of the surgeon and their team performing the intricate operation. The middle ground showcases the delicate instruments and equipment used, casting subtle shadows. In the background, a sterile, clinical environment with pristine white walls and medical monitors, conveying a sense of professionalism and expertise. Convey the gravity and precision required for this critical procedure, while maintaining a clean, technical aesthetic befitting the subject matter.
When other treatments don’t work, surgery might be needed for spinal stenosis. This helps to ease symptoms and improve life quality. Doctors look at how bad the symptoms are and if other treatments helped.
Indications for Surgical Intervention
Surgery is an option for those with severe pain or nerve problems. NYU Langone says surgery is for those with worsening symptoms or pain that won’t go away with other treatments.
The main goal of surgery is to take pressure off the spinal cord or nerves. This helps to reduce pain and improve how well you can move. Surgery is considered when:
- Other treatments haven’t helped enough.
- There’s a lot of nerve compression causing symptoms.
- Pain is very bad and stops you from doing daily things.
Failure of Conservative Treatment
First, doctors try non-surgical treatments like physical therapy and medicine. But if these don’t work, surgery might be next.
A study shows how important it is to pick the right patients for surgery. The table below shows when surgery is likely needed.
| Indication | Description | Clinical Significance |
| Progressive Neurological Deficits | Worsening neurological symptoms such as numbness, weakness, or loss of bladder/bowel control. | High |
| Severe Pain | Pain that interferes with daily activities and is not adequately managed with conservative treatments. | High |
| Significant Nerve Compression | Compression of nerves causing significant symptoms or neurological deficits. | High |
In summary, surgery is an option when other treatments don’t work or if nerves are badly compressed. Knowing when surgery is needed is key to making the right treatment choice.
Surgical Procedures for Spinal Stenosis
A high-resolution photo of a spinal stenosis surgery in progress. The patient is lying on an operating table, with the surgeon’s hands and surgical instruments visible in the foreground, performing a laminectomy procedure to remove bone and relieve pressure on the spinal cord. The background shows the sterile surgical suite, with medical equipment and lighting fixtures creating a clinical atmosphere. The image should convey the technical precision and focused intensity of the procedure, while maintaining a sense of depth and realism.
Spinal stenosis surgery includes different methods, like decompression and stabilization. The type of surgery depends on how severe the stenosis is and the patient’s health.
Overview of Surgical Approaches
Surgeries for spinal stenosis aim to ease pressure on the spinal cord or nerves. Decompression surgery removes bone or tissue that presses on nerves. We’ll look at the various surgical methods and when they’re used.
Decompression vs. Stabilization Procedures
Decompression surgeries, like laminectomy or laminotomy, remove pressure on nerves. On the other hand, stabilization procedures, such as spinal fusion, stabilize the spine when it’s unstable. The choice between these depends on the patient’s condition.
Minimally Invasive vs. Traditional Open Surgery
Minimally invasive surgery is becoming more common for spinal stenosis. It uses smaller cuts and causes less damage than open surgery. Minimally invasive surgery can lead to quicker recovery and less pain. But, it’s not right for every case, depending on the complexity and the surgeon’s skill.
We’ll dive deeper into the details of these surgeries next. This will help us understand the treatment options for spinal stenosis better.
Laminectomy Procedure
A detailed surgical illustration of a laminectomy procedure, showcasing the intricate spinal anatomy and the step-by-step surgical technique. The image should depict a crisp, high-resolution medical illustration viewed from an angled perspective, highlighting the vertebrae, spinal cord, and the removal of the lamina to relieve spinal stenosis. The lighting should be soft and evenly distributed, emphasizing the technical precision of the procedure. The color palette should be muted, with a focus on anatomical accuracy and clarity. The overall composition should convey a sense of medical professionalism and educational value, suitable for inclusion in a medical article on spinal stenosis treatment.
The laminectomy procedure is a common surgery for spinal stenosis. It involves removing the lamina, a bony plate, to relieve nerve pressure. This is according to the Medical organization.
What is a Laminectomy?
A laminectomy is a surgery to treat spinal stenosis symptoms. It removes part or all of the lamina. This creates more space in the spinal canal, reducing pressure on nerves.
Surgical Technique
The laminectomy surgery has several steps:
- Making an incision in the back to access the spine.
- Removing the lamina to decompress the spinal canal.
- In some cases, additional procedures such as discectomy (removal of a herniated disc) may be performed.
The technique used depends on the patient’s condition and the surgeon’s judgment.
Expected Outcomes
The laminectomy can greatly relieve symptoms like pain, numbness, and weakness. These symptoms occur in the legs or arms, depending on the stenosis location. The procedure improves mobility and reduces pain.
| Outcome | Description | Timeline |
| Pain Relief | Reduction in pain due to decompression of nerves | Immediate to several weeks |
| Improved Mobility | Enhanced ability to perform daily activities | Several weeks to months |
| Return to Normal Activities | Gradual return to pre-surgery activities | Several months |
Following post-operative instructions is crucial for a good recovery and outcomes.
Laminotomy: A Less Invasive Alternative
Laminotomy is a new way to treat spinal stenosis. It’s less invasive than traditional methods. This method removes part of the lamina, which is the bony plate covering the spinal canal. This helps reduce pressure on the spinal cord and nerves, easing pain and discomfort.
Procedure Details
The laminotomy procedure is precise and minimizes tissue damage. Surgeons make a small incision in the back. They use special tools to remove part of the lamina.
This method helps decompress nerves without harming the spine too much. It’s very adaptable to each patient’s needs. The amount of lamina removed depends on the severity and location of the stenosis.
Benefits and Limitations
Laminotomy has many advantages. It has a shorter recovery time compared to more invasive surgeries. This is because it causes less tissue damage. Patients often experience less pain and can get back to their activities faster.
Benefits of Laminotomy:
- Less invasive with smaller incisions
- Reduced risk of spinal instability
- Shorter recovery period
- Less post-operative pain
But, laminotomy isn’t right for everyone. It might not work for those with severe stenosis or unstable spines. The success of the procedure also depends on the surgeon’s skill and the patient’s condition.
| Procedure | Invasiveness Level | Recovery Time | Spinal Stability Impact |
| Laminotomy | Minimally Invasive | Shorter | Less Impact |
| Laminectomy | More Invasive | Longer | Potential for Instability |
In conclusion, laminotomy is a good option for treating spinal stenosis. It balances effectiveness with minimal invasiveness. While it has its limits, its benefits make it a good choice for many patients.
Foraminotomy for Nerve Root Decompression
Foraminotomy can greatly help with spinal stenosis symptoms. It makes the foramen wider. This lets nerves exit the spinal canal without pressure.
Surgical Approach
The surgery aims to be as small as possible. We use advanced imaging to guide it. This ensures the nerve is freed from bone or tissue.
The patient is positioned for the best access. Specialized retractors are used. They help keep tissue damage low, speeding up recovery.
Ideal Candidates
Those with nerve root compression symptoms are best for foraminotomy. We look at each case carefully. We consider symptom severity, health, and past treatments.
It’s for those who didn’t get better with other treatments or have big nerve problems. Our team talks with patients to find the best treatment. They make sure patients know the benefits and risks.
Spinal Fusion Surgery
For those with spinal instability, spinal fusion surgery is a top choice. It joins two or more vertebrae together. This is done using bone grafts and hardware, as the Medical organization advises. It’s for those with big spinal deformities or instability.
When Fusion is Recommended
Spinal fusion is suggested when other treatments don’t work. It’s for those with big spinal instability or deformity. We look at many things before suggesting it, like how bad the symptoms are and the patient’s health.
- Significant spinal instability or deformity
- Severe symptoms that impact daily life
- Failure of conservative treatments
Fusion Techniques and Materials
There are many ways and materials for spinal fusion surgery. The choice depends on the patient’s condition and the surgeon’s choice.
Fusion Techniques:
- Posterior lumbar interbody fusion (PLIF)
- Transforaminal lumbar interbody fusion (TLIF)
- Anterior lumbar interbody fusion (ALIF)
Materials Used:
- Bone grafts (autograft or allograft)
- Metal hardware (screws, rods, cages)
Long-term Outcomes
Spinal fusion surgery can greatly improve life in the long run. It can make symptoms better, increase mobility, and improve quality of life. But, like any surgery, there are risks and complications to talk about.
It’s key to talk fully with your healthcare provider about the benefits and risks of spinal fusion surgery.
Minimally Invasive Surgical Options
For those with spinal stenosis, new surgery options are available. These options are less invasive than traditional surgery. Our team has seen great progress in these methods, leading to less damage and faster healing.
Endoscopic Procedures
Endoscopic procedures use a small camera and tools through tiny cuts. This method causes less damage and less pain after surgery. Our doctors use it to free up nerves and ease spinal cord pressure.
- Smaller cuts mean less scarring
- Less muscle harm means quicker healing
- Smaller wounds lower infection risk
Tubular Retractor Systems
Tubular retractor systems are another new way to treat spinal stenosis. They use a tube to move muscles aside, giving access to the spine with less muscle damage. This is great for those needing more extensive surgery.
These systems let our surgeons work precisely on the problem area, with little impact on other tissues.
Advantages Over Traditional Surgery
Minimally invasive surgery has many benefits over traditional methods:
- Healing happens faster with less tissue harm
- Less pain and discomfort after surgery
- Smaller cuts mean less scarring
- Lower chance of complications and infections
Choosing these new surgical options means patients can have shorter hospital stays and get back to their lives sooner. We’re excited about how these advancements will keep improving patient care and happiness.
Preparing for Spinal Stenosis Surgery
Getting ready for spinal stenosis surgery is key to a smooth and successful experience. Proper preparation can greatly affect the surgery’s outcome and your recovery.
Medication Management
Managing medications is also crucial. Patients need to:
- Tell their doctor about all medications they’re taking
- Stop certain medications that could risk bleeding or interfere with surgery
- Change medication dosages as advised by their healthcare provider
Following the surgeon’s advice on medication is key to avoiding risks during and after surgery.
What to Expect on Surgery Day
Knowing what to expect on surgery day can help reduce anxiety. On surgery day:
- Patients arrive at the hospital or surgical center a few hours before surgery
- They get ready for surgery by changing into a gown and getting IV lines
- The surgical team reviews the procedure, answers questions, and makes sure the patient is ready
Understanding the steps to prepare for spinal stenosis surgery helps patients navigate the process better. It’s a team effort between the patient and healthcare team for the best results.
Anesthesia Options for Spine Surgery
Choosing the right anesthesia option is a key decision for spine surgery. The type of anesthesia affects your surgery experience and recovery. We help patients pick the best anesthesia plan, considering their health, surgery type, and personal wishes.
General Anesthesia
General anesthesia is often used for spine surgeries, like those for spinal stenosis. It makes you completely asleep during the surgery. This is great for complex or long surgeries. Our skilled anesthesiologists use a mix of intravenous and inhaled anesthetics.
Choosing general anesthesia depends on your health, surgery complexity, and comfort with being asleep.
Regional Anesthesia Considerations
Regional anesthesia numbs a specific body area. For spine surgery, it might numb the spine area. It can lead to less pain and quicker recovery for some surgeries.
But, it’s not right for everyone. Your medical history, surgery type, and preferences matter. Our anesthesiologists and the surgical team decide if it’s a good choice for you.
In summary, picking between general anesthesia and regional anesthesia for spine surgery is complex. We consider many factors and use the latest technology and techniques. Our goal is to ensure the best results for our patients.
Recovery and Rehabilitation
Recovery and rehabilitation are key after spinal stenosis surgery. They need careful planning and execution. A good rehabilitation program is vital for the best results.
Immediate Post-Operative Period
The first days after surgery are crucial. Patients are watched closely for any problems. Managing pain is a top priority.
We stress the importance of following instructions closely. This helps avoid risks.
Physical Therapy Protocols
Physical therapy is essential in the recovery process. It helps patients regain strength and mobility. Each patient gets a physical therapy plan tailored to their needs.
Our therapy includes exercises to improve posture and reduce pain. We work with physical therapists to give patients the best care.
Timeline for Return to Activities
The time it takes to get back to normal varies. It depends on the surgery and the patient’s health. Usually, it takes a few weeks to a few months.
Patients should avoid heavy lifting and bending at first. They should slowly get back to activities. Healthcare professionals will monitor them to ensure a smooth recovery.
Following a structured rehabilitation plan helps patients get the best results after surgery. We are dedicated to supporting patients through the recovery and rehabilitation process.
Potential Risks and Complications
It’s important to know the risks and complications of spinal stenosis surgery. Surgery can help with symptoms, but there are possible problems. Knowing these can help you make a better choice.
Common Surgical Complications
Complications can happen during or after surgery. These include infection, nerve damage, and bleeding. Infections might need antibiotics or more surgery. Nerve damage can cause pain, numbness, or weakness.
Common Surgical Complications:
- Infection
- Nerve damage
- Bleeding
- Reaction to anesthesia
Long-term Risks
Long-term risks include spinal instability, stenosis coming back, and chronic pain. Spinal instability might need more surgery. Stenosis coming back can happen if the surgery doesn’t fully fix the problem.
| Long-term Risk | Description | Management |
| Spinal Instability | Instability of the spine post-surgery | Additional surgery for stabilization |
| Recurrence of Stenosis | Return of stenosis symptoms | Further surgical intervention or conservative management |
| Chronic Pain | Persistent pain after surgery | Pain management through medication or therapy |
Risk Factors for Poor Outcomes
Some factors can make outcomes worse after surgery. These include age, health, and other medical conditions. Older people or those with health issues like diabetes or heart disease might be at higher risk. Knowing these can help in planning better care before and after surgery.
Risk Factors:
- Advanced age
- Presence of comorbidities
- Poor overall health
- Smoking
Emerging Technologies in Spinal Stenosis Surgery
The field of spinal stenosis surgery is seeing big changes with new technologies. These advancements aim to make surgeries better, cut down recovery times, and improve patients’ lives.
Artificial Disc Replacement
Artificial disc replacement is a new method. It replaces a bad or worn-out disc with a man-made one. This helps keep the spine moving, which might lower the chance of problems in other parts.
Benefits of Artificial Disc Replacement:
- Preservation of spinal motion
- Reduced risk of adjacent segment disease
- Potential for faster recovery
Robotic-Assisted Surgery
Robotic-assisted surgery is another big step forward in treating spinal stenosis. This tech makes surgeries more precise, allowing for better placement of implants and fewer complications.
Advantages of Robotic-Assisted Surgery:
- Enhanced precision
- Improved accuracy in implant placement
- Reduced risk of surgical complications
As these new technologies keep getting better, we’ll see even more progress in treating spinal stenosis. Patients will have more effective and less invasive options.
Conclusion
Knowing about surgical treatments for spinal stenosis is key for those looking for relief. We’ve covered what spinal stenosis is, its symptoms, how it’s diagnosed, and treatment options.
Surgery is considered when other treatments don’t work. We talked about different surgeries like laminectomy and spinal fusion. We looked at their benefits and risks.
The right surgery depends on where and how bad the stenosis is, and the patient’s health. New, less invasive surgeries are now options. They promise quicker recovery and less damage.
In conclusion, every case is different, and the best treatment is personalized. Understanding surgery options helps patients make informed choices. They can work with their doctors to find the best outcome.
FAQ
What is spinal stenosis and how is it treated?
Spinal stenosis is when the spinal canal gets narrower. This puts pressure on the spinal cord and nerves. Treatment can include medicines, physical therapy, steroid shots, or surgery, based on how bad it is.
What are the common symptoms of spinal stenosis?
Symptoms include back pain, leg pain, and sciatica. You might also feel numbness, tingling, or weakness in your legs. These feelings can change based on where and how bad the stenosis is.
What is the difference between laminectomy and laminotomy?
Laminectomy removes a big part of the vertebra to relieve pressure. Laminotomy is less invasive, taking out a smaller part. It helps keep more of the vertebra intact.
When is spinal fusion surgery recommended?
You might need spinal fusion surgery if your spine is unstable or deformed. It’s also used when just removing pressure isn’t enough to fix symptoms.
What are the benefits of minimally invasive spinal surgery?
This type of surgery has smaller cuts, less damage to tissue, and less blood loss. It also means you can recover faster than with traditional surgery.
What can I expect during the recovery period after spinal stenosis surgery?
You’ll likely stay in the hospital for a short time. Then, you’ll need to rest and do physical therapy to get your strength and mobility back.
What are the potential risks and complications of spinal stenosis surgery?
Risks include infection, bleeding, nerve damage, and instability. The chance of these problems depends on the surgery type and your health.
How do I prepare for spinal stenosis surgery?
Get ready with pre-op tests, manage your meds, and follow your doctor’s instructions. This helps make sure your surgery goes well.
What anesthesia options are available for spinal stenosis surgery?
You can choose between general anesthesia and regional anesthesia. The choice depends on the surgery, your health, and your surgeon’s preference.
Can spinal stenosis be treated without surgery?
Yes, many cases can be treated without surgery. Options include medicines, physical therapy, and steroid injections, based on your symptoms and how severe they are.
What is foraminotomy and who is it suitable for?
Foraminotomy is a surgery that relieves nerve root pressure. It’s for people with symptoms like radiculopathy due to nerve compression.
How does spinal stenosis affect mobility?
It can make it hard to walk or stand for long because of pain, numbness, and weakness in the legs.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10447186/