Last Updated on October 31, 2025 by Saadet Demir
Squamous cell carcinoma (SCC) of the scalp is a serious condition that needs quick medical care. This skin malignancy is more common in sun-exposed areas. It can lead to severe complications if not caught early. 5 key facts about squamous cell skin cancer on scalp, focusing on its common appearance, diagnosis, and treatment.
We know how important early detection and treatment are for the best results. In this article, we’ll talk about the main facts about diagnosing and treating SCC on the scalp. We’ll also highlight the importance of getting medical help quickly.
Early detection greatly improves survival chances. It’s key for patients to know the risks and symptoms of SCC of the scalp.
To understand Squamous Cell Carcinoma (SCC) of the scalp, we need to know its definition, classification, and the unique features of the scalp. SCC is a skin cancer that starts in the squamous cells. These are flat, thin cells on the outer skin layer.
SCC grows out of control, forming tumors. It’s classified by how it looks under a microscope. This helps doctors know how serious it is and what treatment to use.
The Broder’s classification grades SCC from I (well-differentiated) to IV (poorly differentiated). The higher the grade, the more aggressive the tumor.
| Grade | Description | Characteristics |
| I | Well-differentiated | Highly differentiated cells, minimal atypia |
| II | Moderately differentiated | Some loss of differentiation, moderate atypia |
| III | Poorly differentiated | Significant loss of differentiation, marked atypia |
| IV | Undifferentiated | Little to no differentiation, highly atypical |
The scalp has many layers, including skin and hair follicles. Its blood supply and hair follicles make it a special place for SCC. Knowing the scalp’s structure is key to treating SCC.
The scalp’s blood supply helps SCC spread. It’s also important to know how SCC moves through the scalp’s lymphatic system. This helps in managing the cancer.
In summary, to understand SCC of the scalp, we must know its definition, classification, and the scalp’s unique features. This knowledge is vital for diagnosing and treating SCC.

Looking at scalp SCC, we see a big increase in cases worldwide. This is important for doctors and health leaders everywhere.
More people are getting SCC on their scalps globally. This is due to more sun exposure, older populations, and lifestyle changes.
Global Incidence Trends: Scalp SCC cases are going up in many places. This is most true in areas with light-skinned people.
SCC is a big part of scalp cancers. It’s aggressive. Knowing this helps catch it early.
| Type of Tumor | Prevalence (%) |
| Squamous Cell Carcinoma | 40-50 |
| Basal Cell Carcinoma | 30-40 |
| Melanoma | 10-20 |
SCC on the scalp mostly hits older adults. Men get it more than women. People with light skin are at higher risk because they don’t have enough melanin to protect against the sun.
Knowing who gets SCC helps us prevent and catch it early.
Knowing the risk factors for Squamous Cell Carcinoma on the scalp is key. It helps in catching it early and preventing it. Several factors can lead to SCC, and knowing them can help manage the risk.
Ultraviolet (UV) radiation is a big risk for SCC. Being out in the sun or using tanning beds too much raises SCC risk on the scalp. Protective measures like sunscreen, clothes, and shade are vital to lower this risk.
Genetics also play a big part. If you have a family history of skin cancer or conditions like albinism, you’re at higher risk. Genetic counseling can help those with a family history.
Being immunosuppressed is another big risk. This includes people with weakened immune systems, like organ transplant recipients or those with HIV/AIDS. Other factors like past radiation, certain chemicals, and age also increase the risk.
| Risk Factor | Description | Impact |
| Ultraviolet Radiation | Prolonged exposure to UV radiation | Increases SCC risk |
| Genetic Predisposition | Family history or genetic conditions | Higher risk of SCC |
| Immunosuppression | Weakened immune system | Increased susceptibility |
It’s important for both patients and doctors to know the early signs of SCC on the scalp. Spotting these signs early can lead to quicker diagnosis and better treatment.
SCC on the scalp can look different, but often it’s a firm bump or a flat sore with a scaly crust. These spots can hurt when touched and might bleed easily. Look out for changes in size, color, or texture of a spot.
Symptoms like itching or pain in the area are also important signs. Knowing these symptoms can help spot SCC early.
Lesions from SCC on the scalp can change over time. They might start small but grow and become irregular. Watching for these changes is key to catching it early.
As SCC gets worse, the spot might get ulcerated or crusted, and bleed more. These signs show the cancer is getting aggressive.
Some signs need immediate doctor visits. Look out for fast-growing lesions, bleeding that won’t stop, or changes in color or texture. Also, if the spot becomes painful or itchy, it’s a warning sign.
| Red Flag | Description |
| Rapid Growth | Lesion grows quickly in size |
| Uncontrolled Bleeding | Bleeding that doesn’t stop |
| Color or Texture Change | Changes in the lesion’s appearance |
Knowing these red flags helps get medical help quickly. This is vital for managing SCC on the scalp effectively.
“Early detection of SCC on the scalp significantly improves treatment outcomes. Awareness of the clinical presentation and early warning signs is key to this early detection.”
— Expert Opinion
To diagnose squamous cell carcinoma (SCC) on the scalp, doctors use several steps. They start with a clinical exam, then do a biopsy, and finish with histopathological evaluation. These steps are key to accurately identifying SCC and figuring out the best treatment.
The first step in diagnosing SCC on the scalp is a thorough clinical exam. Doctors look at the lesion’s size, shape, color, and any special features. They also check its texture and if it’s tender. A dermatoscope might be used to get a closer look at the lesion.
Doctors also check for signs of a more aggressive tumor. This includes looking for rapid growth, ulceration, or bleeding. Finding these signs can help decide what to do next and how to treat it.
If the exam suggests SCC, a biopsy is done to confirm it. There are a few ways to do this, like wedge and punch biopsies.
The choice of biopsy method depends on the lesion’s size and location, and the doctor’s preference. Both methods give tissue samples that help confirm SCC.
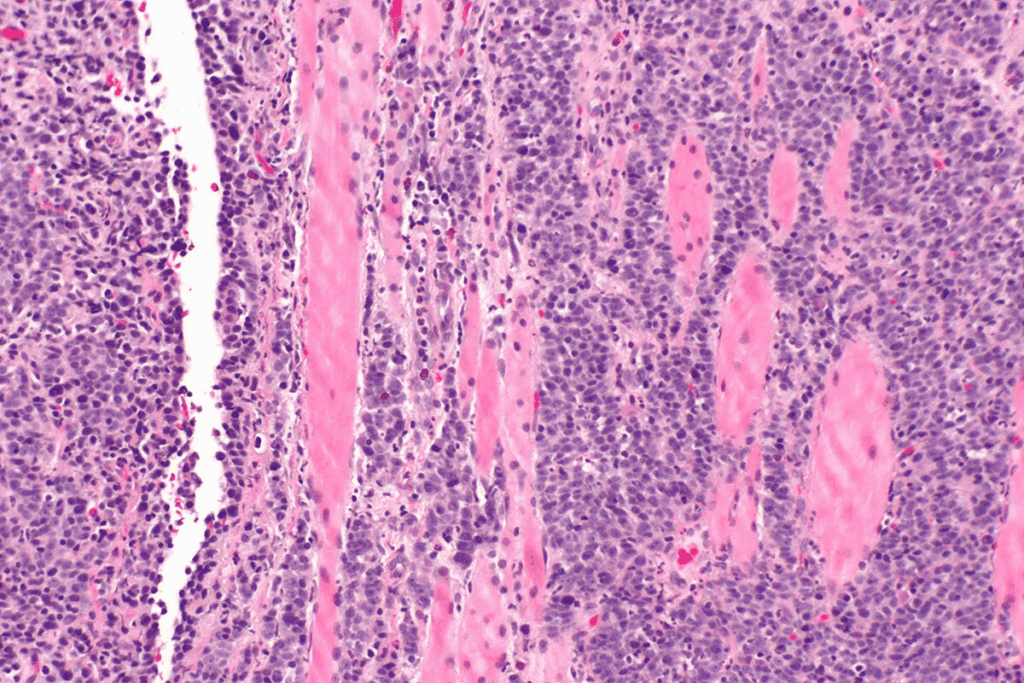
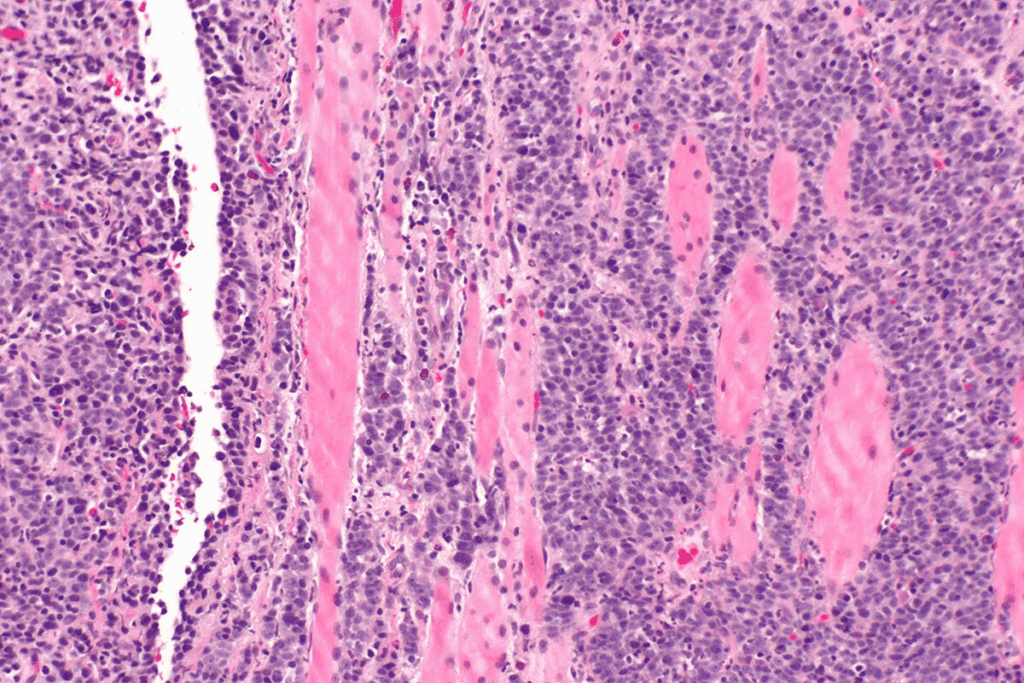
After getting a biopsy sample, it’s examined under a microscope. This helps find signs of SCC, like abnormal cell growth and keratinization.
Doctors also look at the tumor’s thickness, how far it has spread, and if it has high-risk features. These details help stage the cancer and predict its outcome.
| Diagnostic Method | Description | Key Features Assessed |
| Clinical Examination | Visual inspection and dermatoscopy | Lesion size, shape, color, texture, tenderness |
| Wedge Biopsy | Removal of a triangular tissue sample | Tissue architecture, cellular abnormalities |
| Punch Biopsy | Removal of a cylindrical tissue sample | Cellular details, tissue structure |
| Histopathological Evaluation | Microscopic examination of biopsy samples | Tumor thickness, margin status, high-risk features |
Staging SCC on the scalp involves several key steps. These steps help decide the best treatment. Accurate staging and disease assessment are vital for a good prognosis and effective treatment.
The TNM system is used to stage SCC, including scalp SCC. It looks at three main things: the tumor’s size and spread (T), nearby lymph nodes (N), and distant metastasis (M). This helps doctors plan treatment and predict outcomes.
The TNM system helps tailor treatments to each patient. For scalp SCC, the T classification is key. It considers the tumor’s size, depth, and other factors that affect prognosis.
Advanced imaging like MRI and PET scans are vital for SCC staging. MRI shows soft tissue details, helping to see how far the tumor has spread. PET scans find metabolic activity in tumors and check for spread to lymph nodes or distant sites.
These imaging tools add to the TNM system’s insights. They help doctors make better treatment decisions by combining clinical evaluation with advanced imaging.
Lymph node evaluation is key for SCC staging, mainly for scalp tumors. The parotid and cervical regions are common for lymph node metastasis. Clinical exams, imaging, and sometimes biopsies are used to check lymph node involvement.
Knowing about lymph nodes in these areas helps doctors assess recurrence and metastasis risk. This guides the need for treatments like surgery, radiation, or adjuvant therapies.
Scalp squamous cell carcinoma (SCC) is known for its aggressive behavior. This is due to its unique biological traits. It has a high risk of spreading to other parts of the body.
The aggressive nature of scalp SCC comes from several traits. These include:
SCC on the scalp is more likely to spread than SCC in other areas. This is because the scalp has a lot of blood vessels and is close to lymphatic pathways.
Knowing the high-risk features is key to predicting scalp SCC’s behavior. These include:
By understanding these risk factors, doctors can start treatment early. This can lead to better outcomes for patients with scalp SCC.
Scalp SCC treatment uses several key methods. We’ll look at Mohs micrographic surgery, wide local excision, and scalp reconstruction. These are important for treating SCC effectively.
Mohs micrographic surgery is great for scalp SCC. This method checks 100% of the tumor margins. It removes all cancer cells while saving healthy tissue.
A study in the Journal of the American Academy of Dermatology shows Mohs surgery’s high success rate. It’s a top choice for scalp SCC.
“Mohs micrographic surgery has revolutionized the treatment of skin cancers, including SCC on the scalp, by providing a highly effective and tissue-sparing approach.”
– Medical Expert, Journal of Surgical Oncology
Mohs surgery offers many benefits:
Wide local excision (WLE) treats scalp SCC too. It removes the tumor with healthy tissue around it. Margin control is key in WLE to remove all cancer cells.
The margin width depends on the tumor’s size and depth.
| Tumor Size | Recommended Margin |
| <2 cm | 4-6 mm |
| 2-4 cm | 6-10 mm |
| >4 cm | 10-15 mm |
After removing SCC, reconstruction is needed. Scalp-specific reconstruction techniques include primary closure, skin grafting, and local flaps. The right technique depends on the defect size, location, and patient health.
Reconstruction after SCC removal needs a skilled surgeon. The goal is to restore the scalp’s look and function. This helps patients regain confidence and quality of life.
Treating SCC on the scalp needs a team effort. This means using different treatments together to fight the disease well.
Adjuvant radiotherapy is key for those with high-risk SCC. This includes big tumors, deep invasion, or cancer left behind after surgery. Radiotherapy is vital in lowering the chance of SCC coming back, as new guidelines show. Doctors decide on radiotherapy based on the disease’s risk and how far it has spread.
Systemic therapy, like targeted and immunotherapy, is showing great promise for advanced SCC. We’re moving towards treatments that fit each patient’s tumor. Targeted therapies that target specific genetic changes are playing a big role in SCC treatment.
“The integration of systemic therapies into the treatment plan for SCC on the scalp represents a significant advancement in the care of these patients.”
For SCC on the scalp, integrated care is key. It involves a team of experts like dermatologists, surgeons, and oncologists. This team approach ensures patients get all-around care, from start to finish. Together, healthcare teams can create custom treatment plans for each patient’s needs.
Dealing with advanced and metastatic SCC on the scalp needs a detailed plan. This includes complex treatments like regional lymph node dissection and managing intracranial extension. Palliative care is also key.
Removing lymph nodes in the affected area is vital for advanced SCC on the scalp. This surgery stops the disease from spreading further. It’s essential when lymph nodes are involved.
When SCC on the scalp spreads to the brain, it’s a serious issue. A team of experts from neurosurgery, radiation oncology, and medical oncology is needed.
Treatment Options:
Palliative care is essential for patients with advanced and metastatic SCC on the scalp. It focuses on improving life quality by easing symptoms, managing pain, and supporting emotional and social needs.
By using these strategies, we can enhance outcomes and improve life quality for those with advanced and metastatic SCC on the scalp.
Survival rates for SCC on the scalp depend on the disease stage and treatment. Knowing these factors helps doctors and patients plan the best course of action.
Survival rates for SCC on the scalp differ greatly between early and advanced stages. Early-stage SCC, treated quickly, has a much better survival rate. Advanced stages, where cancer may spread, have lower survival rates.
Research shows early-stage SCC has a 5-year survival rate over 80%. But, for advanced stages, this rate drops below 50%. This highlights the need for early detection and treatment.
The treatment chosen greatly affects survival rates for SCC on the scalp. Treatments include surgery, Mohs micrographic surgery, radiotherapy, and systemic therapy.
Choosing the right treatment is key. For example, Mohs surgery is often chosen for its high success rate and ability to save tissue, which is important for the scalp’s appearance.
| Treatment Modality | Early Stage Survival Rate | Advanced Stage Survival Rate |
| Surgical Excision | 85% | 40% |
| Mohs Micrographic Surgery | 90% | 50% |
| Adjuvant Radiotherapy | 88% | 45% |
SCC on the scalp can come back in different ways. Knowing how it recurs helps in managing it better.
Local recurrences are often treated with more surgery or radiotherapy. Regional recurrences might need lymph node removal and more treatments. Distant metastases are treated with systemic therapy to control symptoms and improve life quality.
Regular check-ups are key to catching recurrence early. The timing of these visits depends on the initial stage and treatment.
It’s important to know about squamous cell carcinoma on the scalp early. We’ve talked about how to spot and treat it. Getting medical help quickly is key.
Spotting SCC early and treating it right can help patients live longer. Knowing the signs and how doctors diagnose it helps. This way, patients can get help fast and do better.
Treating SCC on the scalp often needs a team effort. This includes surgery, radiation, and medicine. We stress the need for a full care plan to tackle this serious condition.
In short, squamous cell carcinoma on the scalp needs quick action for better results. Patients and doctors working together can get the best outcomes. Knowing how to diagnose and treat it is vital.
Squamous cell carcinoma (SCC) on the scalp is a type of skin cancer. It starts from the squamous cells, which are thin cells on the skin’s outer layer. The scalp is a common place for SCC because of sun exposure.
Risk factors for SCC on the scalp include UV radiation, genetics, and being immunosuppressed. Other factors are a history of skin cancer, fair skin, and radiation therapy.
Diagnosing SCC on the scalp involves several steps. These include clinical exams, biopsies, and histopathological evaluation. Advanced imaging like MRI and PET scans may also be used.
Treatments for SCC on the scalp include surgery and scalp reconstruction. Mohs micrographic surgery and wide local excision are common. Radiotherapy and systemic therapy may also be needed.
Yes, SCC on the scalp can spread to lymph nodes, like those in the parotid and cervical regions. Checking lymph nodes is important for disease assessment and prognosis.
The prognosis for SCC on the scalp varies. It depends on the disease stage, presence of high-risk features, and treatment success. Early detection and treatment improve survival chances.
Preventing SCC on the scalp involves reducing UV radiation exposure. Wear protective clothing, seek shade, and use sunscreen. Regular skin checks and early detection are also key.
Signs and symptoms of SCC on the scalp include new growths, sores, and firm patches. Watch for rapid growth, bleeding, or pain, which are red flags needing immediate medical attention.
SCC on the scalp can be aggressive, depending on its features and spread to lymph nodes. Understanding SCC’s unique characteristics is vital for effective management.
Multidisciplinary care is essential for SCC on the scalp. It involves a team of healthcare professionals working together. This team may include surgical, radiation, and medical oncologists, among others.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us