Last Updated on December 1, 2025 by Bilal Hasdemir
Stereotactic Radiosurgery (SRS) is a precise way to treat brain tumors and other issues. It uses advanced tech to focus a high dose of radiation on the right spot. This helps avoid harming the healthy tissue around it srs meaning.
This method has changed how we treat some brain problems. It’s a non-surgical option that’s less invasive than traditional surgery. Knowing what SRS means and how it works helps patients choose the best treatment for them.
Key Takeaways
- Stereotactic Radiosurgery is a precise form of radiation therapy.
- It is used to treat tumors and abnormalities of the brain.
- SRS minimizes damage to surrounding healthy tissue.
- This technique offers a non-invasive alternative to traditional surgery.
- Understanding SRS is key for making informed treatment choices.
Understanding Stereotactic Radiosurgery (SRS): Definition and SRS Meaning
Stereotactic Radiosurgery is a non-invasive method that uses precise radiation. It treats tumors and vascular issues in the brain and body. This method has changed how we treat these conditions.
The Science Behind Stereotactic Radiosurgery
SRS targets tumors or lesions with great accuracy. It uses advanced imaging and radiation systems. This precision lets SRS use higher doses of radiation than traditional therapy, making it more effective.
The main parts of SRS are:
- Advanced imaging: MRI, CT, and angiography help find the target.
- Stereotactic frame or mask: Keeps the patient’s head or body steady and in place.
- Radiation delivery: Uses linear accelerators or Gamma Knife technology to send radiation.
How SRS Differs from Conventional Radiation Therapy
SRS is different from traditional radiation therapy in many ways. It gives a higher dose of radiation in fewer sessions, often just one. Traditional therapy takes many sessions over weeks.
SRS also targets tumors more precisely. It uses stereotactic localization for sub-millimeter accuracy. Traditional therapy may affect more tissue.
The advantages of SRS over traditional therapy are:
- Shorter treatment time: SRS usually needs just one session.
- Less invasive: No surgery is needed.
- High accuracy: It targets the tumor well, saving healthy tissue.
Knowing about SRS helps patients and doctors decide if it’s right for certain conditions.
The Evolution and History of Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) has changed a lot over time. It now helps treat brain tumors and vascular malformations in a precise way. This method is non-invasive and is used all over the world. Let’s look at how SRS has evolved.
Development of Gamma Knife Technology
The Gamma Knife technology is key to SRS’s growth. Gamma Knife radiosurgery uses cobalt sources to target specific areas. This reduces harm to nearby tissues.
First introduced in the 1960s, the Gamma Knife has improved over the years. New imaging and radiation delivery tech have made it better. These changes have helped treat more conditions and improve patient results.
Advancements in SRS Technology Over Time
SRS technology has also made big strides. Now, MRI and CT scans help target tumors and malformations more accurately. Better radiation systems have also improved SRS’s precision and effectiveness.
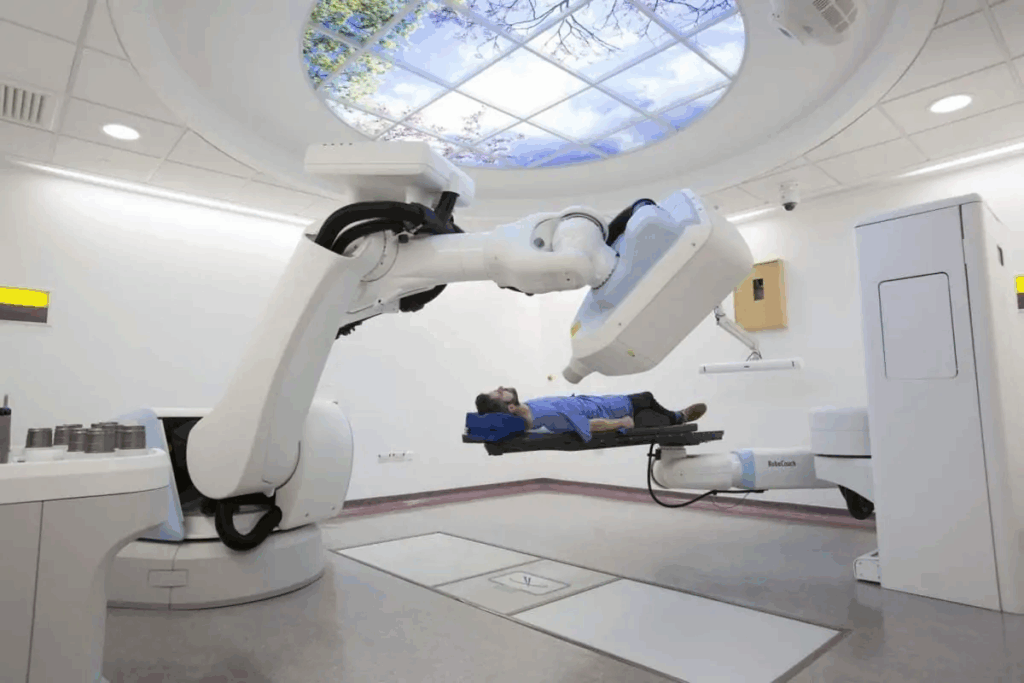
New SRS platforms have come up, using LINACs and robotic systems. These make SRS more accessible and treat more conditions. SRS’s ongoing development shows its value in modern cancer treatment.
How Stereotactic Radiosurgery Works
SRS is a top-notch treatment that uses cutting-edge tech to hit tumors with unmatched precision. This is key for treating conditions that are very sensitive to radiation. It also helps in keeping healthy tissue safe from harm.
The Precision Targeting Mechanism
The heart of SRS’s success is its precise targeting. Advanced imaging like MRI and CT scans pinpoint the tumor’s location. This info helps create a detailed plan for the treatment.
Precision gets even better with the help of special frames or masks. These keep the target area steady, ensuring the radiation hits the right spot every time. This mix of advanced imaging and immobilization lets doctors give high doses of radiation to the tumor while protecting nearby tissues.
Radiation Delivery Systems in SRS
SRS employs different radiation delivery systems for its precision. The Gamma Knife is one, using cobalt sources to focus radiation beams on the target. LINACs are another tool, capable of firing radiation from various angles for precise targeting.
The right system depends on the tumor’s size, location, and other factors. Our team of experts works with patients to pick the best treatment plan. This ensures they get the best care possible.
The SRS Meaning in Modern Oncology and Its Importance
Stereotactic Radiosurgery (SRS) has changed oncology with its exact and non-invasive treatment. It uses high doses of radiation on specific targets, protecting healthy tissues nearby.
SRS is key in modern oncology for treating tumors without surgery. This method is safer and faster than old surgeries, helping patients recover quicker.
Advantages Over Traditional Surgery
SRS beats traditional surgery in many ways. It has less recovery time, lower infection risk, and can treat tumors in hard spots. It can even tackle multiple tumors at once, making it a smart choice for those with many lesions.
Advantages | SRS | Traditional Surgery |
Recovery Time | Minimal to none | Several weeks to months |
Risk of Infection | Low | Moderate to high |
Tumor Accessibility | Can treat hard-to-reach areas | Limited by surgical access |
In summary, SRS is a vital tool in modern oncology. It’s precise, non-invasive, and effective for many tumors. Its benefits over traditional surgery make it a preferred choice for both patients and doctors.
Primary Brain Tumors Ideal for SRS Treatment
Certain primary brain tumors are best treated with Stereotactic Radiosurgery (SRS). We’ll look at meningiomas, acoustic neuromas, and pituitary adenomas as examples.
Meningiomas: Size and Location Considerations
Meningiomas are usually benign and grow from the meninges. The size and location of meningiomas are key in deciding if SRS is right. Small to medium-sized tumors near important areas are often good candidates. SRS is precise, helping to treat the tumor without harming nearby tissues.
Acoustic Neuromas (Vestibular Schwannomas): Treatment Outcomes
Acoustic neuromas are benign tumors on the nerve from the inner ear to the brain. SRS is very effective in treating these tumors, keeping hearing in many cases. The results are usually good, with few side effects.
Pituitary Adenomas: Success Rates and Limitations
Pituitary adenomas grow in the pituitary gland at the brain’s base. SRS is used for tumors not helped by medication or surgery. The success of SRS depends on tumor size and how close it is to important areas. While SRS works well, it has limits, like with large tumors or those near sensitive spots.
In summary, SRS is a great option for certain brain tumors, providing precise and effective treatment. Choosing SRS depends on the tumor’s size, location, and type.
Metastatic Brain Tumors and SRS Efficacy
Stereotactic Radiosurgery (SRS) is a top choice for treating metastatic brain tumors. It offers hope to those with complex cancer cases. These tumors come from cancers that have spread to the brain from other parts of the body. SRS is key because it’s precise and effective in treating these tumors.
Single vs. Multiple Brain Metastases: Treatment Approaches
How SRS treats brain metastases changes based on the number of tumors. For one tumor, SRS can be a final treatment to remove it without harming the brain. But, for many tumors, SRS treats each one separately. The number of tumors SRS can handle is something researchers are studying.
Tumor Size Considerations and Limitations
The size of the tumor is very important for SRS treatment. SRS works best for tumors 3 cm or less. Bigger tumors might risk harming the brain. Yet, SRS can sometimes be used with other treatments for larger tumors.
Primary Cancer Types with Brain Metastases Most Responsive to SRS
Some cancers are more likely to have brain tumors that SRS can treat well. These include breast cancer, non-small cell lung cancer (NSCLC), and melanoma. How well SRS works depends on the cancer type, tumor size and number, and if there’s cancer outside the brain.
The table below shows how well SRS works for different cancers:
Primary Cancer Type | Local Control Rate | Overall Survival Benefit |
Breast Cancer | 80-90% | Yes |
NSCLC | 70-85% | Yes |
Melanoma | 60-80% | Variable |
In summary, SRS is a powerful treatment for brain tumors, with results based on tumor size, number, and cancer type. Knowing these factors helps doctors choose the right patients for SRS. This improves patient outcomes.
Spine Tumors Treatable with Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) is now a key treatment for spine tumors. It’s precise and doesn’t need big cuts. This method is changing how we treat spine tumors, making SRS a great choice instead of old surgeries.
Selection Criteria for Primary Spine Tumors
Doctors pick primary spine tumors for SRS based on size, location, and type. Tumors that can’t be removed or are too risky for surgery are perfect for SRS.
- Tumor size: Smaller tumors are generally more suitable.
- Location: Tumors in sensitive or hard-to-reach areas may benefit from SRS.
- Histology: Certain tumor types respond better to SRS than others.
Managing Metastatic Spine Tumors
Metastatic spine tumors need a team effort to manage. SRS is key for controlling pain and keeping the spine stable. This makes life better for patients.
Tumor Type | Pain Control | Stability Improvement |
Metastatic | Significant reduction in pain | Improved spinal stability |
Primary | Effective pain management | Enhanced structural integrity |
Quality of Life Improvements After Spine SRS
Patients get a big boost in quality of life after SRS for spine tumors. They feel less pain, move better, and don’t have to deal with big surgeries.
Using SRS, we can hit spine tumors right on target without harming nearby important areas. This not only makes treatment better but also improves care for patients.
Vascular Abnormalities and Functional Disorders Treated with SRS
SRS is a precise treatment for complex vascular and functional disorders. It’s changing how we manage these conditions. This is thanks to SRS technology advancements.
Arteriovenous Malformations (AVMs): Size and Location Factors
AVMs are abnormal connections between arteries and veins. The size and location of AVMs affect SRS treatment. Smaller AVMs respond better to SRS, with higher success rates.
The AVM’s location is also key. AVMs in deep or critical brain areas need precise targeting. SRS is effective in treating AVMs, even in hard-to-reach spots.
Trigeminal Neuralgia: Success Rates and Patient Selection
Trigeminal neuralgia causes intense face pain. SRS is a good option for those who haven’t found relief with other treatments. Many patients see long-term pain relief with SRS.
Choosing the right patients for SRS is important. We look at symptom severity, past treatments, and neurovascular compression.
Other Neurological Conditions Amenable to SRS
SRS is also being used for other neurological conditions. This includes some types of epilepsy and other disorders. Its precision and non-invasive nature make it appealing for hard-to-treat conditions.
As SRS technology improves, it will help more patients. It offers new hope for those with complex neurological conditions.
Tumor Characteristics That Determine SRS Suitability
Tumor characteristics are key in deciding if SRS is a good treatment option. The success of SRS depends on the tumor’s size, its location, and how well it responds to radiation.
Size Limitations: Why Smaller Tumors Respond Better
The size of the tumor is a big factor in SRS suitability. Smaller tumors do better with SRS because it’s so precise. “The smaller the tumor, the more effective SRS can be,” says Medical Expert, a top neurosurgeon.
For SRS, tumors under 3 cm are best. Bigger tumors might need other treatments, like fractionated radiation therapy.
Location Considerations: Critical Structures and Safety Margins
The tumor’s location is also very important for SRS. Tumors near important areas, like the brainstem or optic nerves, need careful planning. This ensures the radiation dose to these areas is low.
We use advanced imaging and software to plan the treatment. This creates a safety margin around the tumor. It makes sure the radiation is precise and safe.
Radioresistant vs. Radiosensitive Tumors: Treatment Adaptations
The tumor’s radiosensitivity is also key. How well a tumor responds to radiation affects SRS success. Tumors that are more sensitive to radiation do better with SRS.
For tumors that are less sensitive, we might adjust the treatment. This could mean using higher doses of radiation or combining SRS with other treatments.
By looking at tumor characteristics, we can choose the best treatment for each patient. This makes SRS more effective and reduces side effects.
The SRS Treatment Process: What Patients Can Expect
Learning about the SRS treatment process can ease patient worries. We help our patients through every step, from the first meeting to after the treatment. This ensures they know what to expect and feel comfortable.
Pre-Treatment Planning and Imaging
The first step is detailed pre-treatment planning. We use MRI and CT scans to find the tumor’s exact location. Our team then creates a treatment plan based on the tumor’s size, shape, and location.
Accurate imaging is key for SRS success. It helps us target the radiation precisely, protecting healthy tissues.
The Stereotactic Frame Application
A stereotactic frame is often used to keep the patient’s head steady. It’s applied under local anesthesia and might cause some discomfort. But it’s essential for the treatment.
We make sure the frame is comfortable and secure. We’re here to answer any questions or concerns.
The Treatment Session Experience
On treatment day, the frame is attached to the SRS machine. The session is usually painless and can last from a few minutes to hours. It depends on the case’s complexity.
Our team is with you during the session. We’re here to support and make sure you’re comfortable.
Post-Treatment Care and Follow-up
After treatment, we watch for any immediate side effects. Then, we give detailed care instructions. This includes follow-up appointments and scans to check the treatment’s success.
Follow-up care is vital for SRS success. We work with patients and their doctors to manage side effects and monitor treatment results.
Potential Side Effects and Complications of SRS
Stereotactic Radiosurgery (SRS) is a top choice for treating many tumors and conditions. Yet, it comes with possible side effects and complications. Knowing both short-term and long-term effects is key to giving patients the best care.
Short-Term Side Effects and Management
Right after SRS, patients might feel tired, have headaches, or feel sick to their stomach. These symptoms are usually not too bad and can be helped with medicine. For example, doctors might give corticosteroids to lessen swelling and ease headaches and nausea.
Some people might see their symptoms get worse at first because of swelling from the radiation. This swelling is usually short-lived and can be treated with medicine. It’s very important to watch patients closely right after SRS to catch and treat any side effects quickly.
Long-Term Complications to Monitor
Long-term problems from SRS are not as common but can be serious. These might include damage to nearby tissues, causing different symptoms based on where the treatment was given. Regular check-ups are key to catch any long-term issues early and treat them right away.
- Radiation-induced neuropathy
- Cognitive changes
- Hormonal imbalances, in cases where the pituitary gland is irradiated
We keep a close eye on patients over time. If needed, we adjust their treatment plans to lower these risks.
Radiation Necrosis: Recognition and Treatment
Radiation necrosis is a serious problem that can happen after SRS. It’s when the treated tissue dies because of the radiation. Symptoms can be different but often include seizures, headaches, and changes in thinking. Doctors use imaging studies like MRI to tell if it’s necrosis or if the tumor is coming back.
Dealing with radiation necrosis might mean taking medicine to reduce swelling. Sometimes, surgery is needed to remove the dead tissue. It’s very important to know the difference between necrosis and tumor growth to treat it right.
In summary, SRS is a powerful treatment, but it’s important to know and manage its side effects and complications. By watching patients closely and using the right treatments, we can reduce risks and improve their quality of life.
Comparing SRS with Other Treatment Modalities for Various Tumor Types
Choosing between SRS and other treatments depends on many factors. These include the tumor’s type and size, and the patient’s health. We’ll look at the differences to help patients and doctors make better choices.
SRS vs. Conventional Surgery: Decision Factors
Several factors are important when deciding between SRS and surgery. These include the tumor’s location, size, and type. Also, the patient’s health and risk for surgery matter.
Key considerations:
- Tumor location and accessibility
- Patient’s surgical risk and health status
- Tumor type and responsiveness to SRS
Surgery is often chosen for bigger tumors or those pressing on important areas. But SRS is a good option for smaller, more focused tumors.
SRS vs. Whole Brain Radiation Therapy (WBRT): When Each is Appropriate
The choice between SRS and WBRT depends on the brain metastases. It also depends on the patient’s overall health and outlook.
Treatment Characteristics | SRS | WBRT |
Treatment Area | Localized to tumor site | Entire brain |
Dose Fractionation | Single high dose | Fractionated doses |
Ideal for | Limited number of metastases | Multiple metastases or diffuse disease |
SRS vs. Stereotactic Body Radiation Therapy (SBRT): Applications and Differences
SRS is mainly for brain tumors, while SBRT targets tumors outside the brain. Both use precise, high-dose radiation.
Key differences:
- Anatomical location (intracranial vs. extracranial)
- Tumor characteristics and responsiveness
- Treatment planning and delivery systems
In conclusion, choosing between SRS and other treatments requires a detailed look at the tumor and patient. Understanding each treatment’s strengths and weaknesses helps doctors tailor care plans.
Conclusion: The Future of Stereotactic Radiosurgery in Tumor Treatment
Stereotactic Radiosurgery (SRS) is getting better and being used more in treating tumors. It’s improving and growing in the field of oncology. This is good news for those fighting cancer.
Thanks to new technology, SRS can now target tumors more accurately. This means it can harm less of the healthy tissue around the tumor. It’s becoming a key choice for treating tumors that can’t be removed or are in hard-to-reach places.
New developments in SRS technology are on the horizon. These will likely make SRS even more effective in treating complex tumors. This could bring new hope to patients all over the world.
SRS is a non-invasive method with high success rates. It’s set to stay a big part of cancer treatment. With ongoing research, SRS could lead to better outcomes and quality of life for cancer patients. This shows how important SRS is in the battle against cancer.
FAQ
What is Stereotactic Radiosurgery (SRS) and how does it work?
Stereotactic Radiosurgery (SRS) is a precise radiation therapy. It uses many beams to target tumors with little harm to healthy tissue. A high dose of radiation is given in one session or a few.
What types of tumors are best suited for SRS treatment?
SRS works well for small to medium-sized tumors. These are tumors that are clearly defined and hard to reach surgically. Examples include brain tumors like meningiomas and pituitary adenomas.
How does SRS differ from conventional radiation therapy?
SRS is more precise and delivers a high dose of radiation in a few sessions. Conventional therapy gives lower doses over more sessions.
What is Gamma Knife Radiosurgery?
Gamma Knife Radiosurgery uses a machine to send precise gamma radiation to the brain. It treats brain disorders like tumors and vascular malformations.
What are the possible side effects of SRS?
Side effects can include fatigue, headache, nausea, and radiation necrosis. The risk varies based on the tumor’s location, size, and type, and the radiation dose.
How is SRS used to treat metastatic brain tumors?
SRS targets metastatic brain tumors with high radiation doses. This minimizes damage to the brain. It’s effective for those with a few metastases.
Can SRS be used to treat spine tumors?
Yes, SRS treats spine tumors, including primary and metastatic ones. It helps control pain and stabilize the spine.
What are the advantages of SRS over traditional surgery?
SRS is non-invasive and has fewer complications. It’s also good for tumors in sensitive or hard-to-reach areas.
How is the suitability of a tumor for SRS determined?
Suitability for SRS depends on tumor size, location, and radiosensitivity. Smaller, well-defined tumors away from critical areas are best for SRS.
What is the process of undergoing SRS treatment?
SRS treatment involves planning, applying a stereotactic frame, the treatment session, and post-care. The details vary by SRS type.
References
Nature. Stereotactic Radiosurgery for Brain Tumors A Treatment Option. Retrieved from https://www.nature.com/articles/s41467-024-47998-8