Last Updated on December 1, 2025 by Bilal Hasdemir

Did you know over 100,000 patients worldwide have had stereotactic radiosurgery (SRS)? This is for brain conditions like tumors and vascular malformations. It’s a precise radiation therapy that has changed how we treat complex brain disorders. What is the life expectancy after SRT radiation? We explore the prognosis and critical survival rates. Discover the definitive facts now.
We focus on giving top-notch care to patients from around the world. Stereotactic radiosurgery is a key treatment that has made a big difference. By understanding SRS’s role in treating brain conditions, we see its big impact on life expectancy.
Key Takeaways
- Stereotactic radiosurgery is a precise form of radiation therapy.
- SRS is used to treat brain tumors and vascular malformations.
- The treatment has improved patient outcomes and life expectancy.
- We provide complete care for international patients.
- SRS is a highly effective treatment option for complex brain disorders.
Understanding Stereotactic Radiosurgery (SRS)
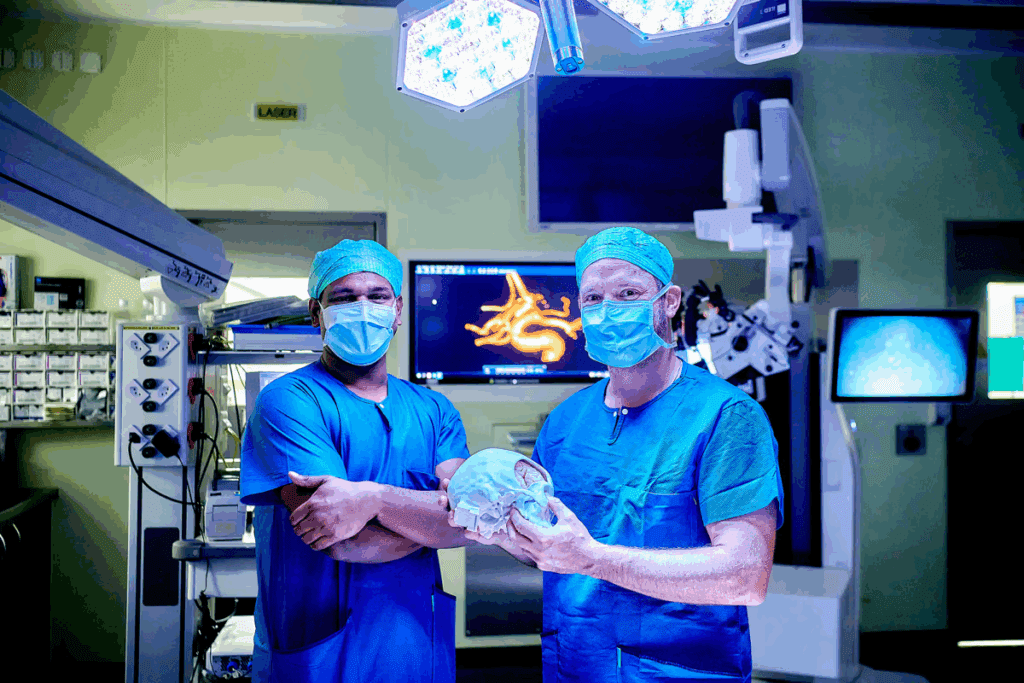
Stereotactic radiosurgery (SRS) has changed the way we treat cancer. It’s precise and effective. We’ll look into what SRS is, how it started, and what makes it different from regular radiation therapy.
Definition and Basic Principles
SRS is a method that uses focused radiation to treat tumors and lesions. It doesn’t cut into the body like surgery does. Instead, it sends high doses of radiation to exact spots, protecting healthy tissues nearby. The basic principle of SRS is its ability to target lesions with great accuracy using advanced imaging and radiation systems.
The process starts with imaging, like MRI and CT scans, to find the target area. Then, software plans the best radiation dose. Last, machines like the Gamma Knife or linear accelerators deliver the radiation.
Historical Development of SRS
Lars Leksell, a Swedish neurosurgeon, first thought of SRS in the 1950s. It was first used for conditions like trigeminal neuralgia and arteriovenous malformations. Over time, SRS has grown, treating more conditions like brain tumors and metastases.
Studies show SRS has come a long way. It’s now a key part of radiation oncology thanks to technology and technique improvements.
How SRS Differs from Conventional Radiation
SRS is different from regular radiation therapy in several ways. It uses higher doses in fewer fractions, making it more effective for some tumors. It also uses advanced systems for precise radiation delivery, protecting healthy tissues.
| Characteristics | SRS | Conventional Radiation |
| Dose per Fraction | High | Lower |
| Number of Fractions | Fewer (often single) | Multiple |
| Targeting Precision | High | Variable |
SRS’s precision and effectiveness make it a valuable treatment option. As technology improves, SRS will become even more important in cancer treatment and radiation oncology.
SRT Radiation: The Technical Approach to Precision Treatment
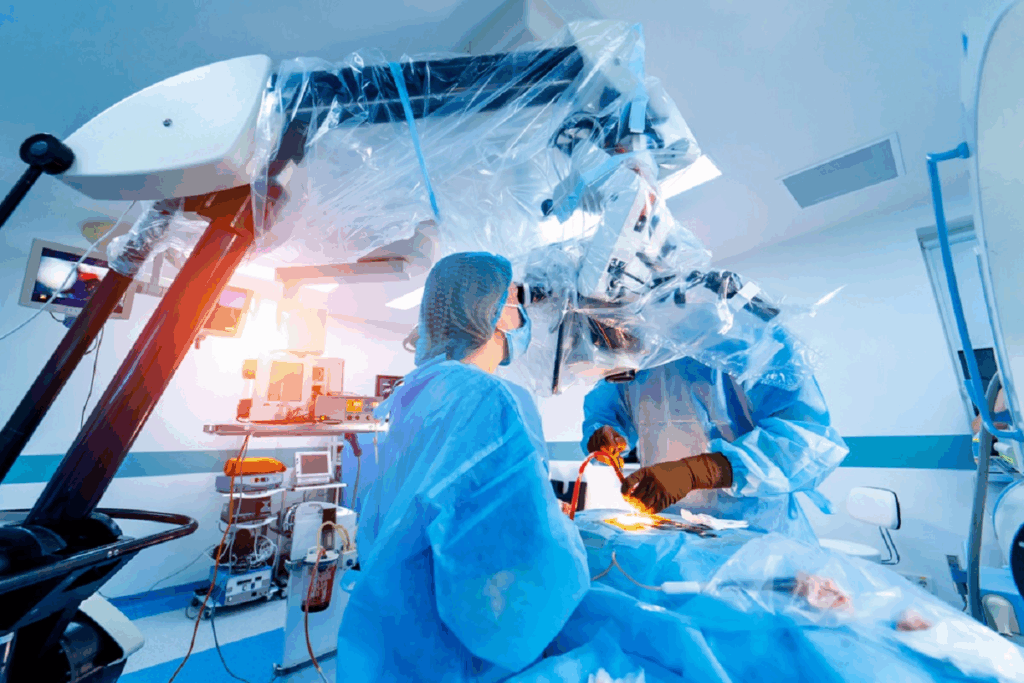
SRT radiation has changed the game in radiation therapy. It allows for precise treatment with little harm to nearby tissues. This is thanks to advanced imaging and delivery systems that pinpoint tumors accurately.
What Makes SRT Radiation Unique
SRT radiation stands out because it can focus high doses of radiation on specific areas. It does this while protecting healthy tissue. This is thanks to cutting-edge imaging like image-guided radiation therapy (IGRT), which tracks the tumor in real-time.
Key Features of SRT Radiation:
- High precision in tumor targeting
- Advanced imaging technologies for real-time monitoring
- Ability to deliver high doses of radiation
- Minimized damage to surrounding healthy tissues
Equipment and Technology Used
The tools and tech behind SRT radiation are key to its success. Linear accelerators create the radiation beams. Advanced software and algorithms help target the tumor precisely.
| Technology | Description | Benefit |
| Linear Accelerators | Generate radiation beams | Precise delivery of radiation |
| Image-Guided Radiation Therapy (IGRT) | Real-time imaging during treatment | Accurate tumor targeting |
| Advanced Software and Algorithms | Enable precise targeting and dose calculation | Optimized treatment outcomes |
Delivery Methods and Protocols
The way SRT radiation is delivered is all about precision and safety. Treatment plans are tailored to each patient’s needs. Quality checks ensure the treatment is accurate.
By using the latest tech and strict protocols, SRT radiation is a top choice for cancer treatment. It leads to better outcomes and a better life for patients.
Common Conditions Treated with Stereotactic Radiosurgery
SRS is a non-invasive method that treats serious health issues with high accuracy. It’s a sophisticated treatment for complex and life-threatening conditions.
Brain Tumors and Metastases
SRS is great for treating brain tumors and metastases. It delivers precise radiation doses directly to the tumor site, protecting healthy tissue. This is helpful for tumors that are hard to reach surgically or are in sensitive brain areas.
- Primary brain tumors: SRS treats various primary brain tumors, like meningiomas and acoustic neuromas.
- Brain metastases: For brain metastases, SRS is a top choice, boosting survival and quality of life.
Arteriovenous Malformations
AVMs are abnormal connections between arteries and veins, posing serious health risks. SRS is a preferred treatment for many AVMs due to its precision and non-invasive nature.
The goal of SRS in treating AVMs is to close off the abnormal vessels, lowering the risk of bleeding and complications.
Trigeminal Neuralgia
Trigeminal neuralgia is a chronic pain condition affecting the trigeminal nerve. SRS is used when other treatments fail. It delivers a precise dose of radiation to the nerve root, providing significant pain relief.
Other Neurological Conditions
SRS is also explored for treating other neurological disorders. Research is ongoing to see if SRS works for conditions like certain types of epilepsy and other functional disorders.
SRS’s versatility and precision make it a valuable treatment for many serious medical conditions. As technology advances, SRS’s uses are likely to grow, bringing new hope to patients with complex health challenges.
Life Expectancy for Brain Tumor Patients After SRS
The life expectancy of brain tumor patients after Stereotactic Radiosurgery (SRS) is complex. SRS is a key treatment for brain tumors, known for its precision. But, it’s hard to predict life expectancy without looking at many factors.
These factors include the tumor type, size, and location, and the patient’s health. Each one plays a role in how well a patient might do after SRS.
Primary Brain Tumors: Survival Rates
Primary brain tumors like glioblastoma, meningioma, and acoustic neuroma have different survival rates after SRS. Glioblastoma is very aggressive and has a poor prognosis. On the other hand, meningiomas are usually benign and have better survival rates after SRS.
We will dive into these differences. This will give us a better understanding of what to expect for patients with different types of primary brain tumors.
Brain Metastases: Impact on Prognosis
Brain metastases, which come from cancers elsewhere, greatly affect a patient’s prognosis after SRS. Having many metastases makes treatment harder and usually means a worse outlook. We will look at how the number, size, and location of metastases affect life expectancy.
We will also see how SRS helps manage these complex cases.
Factors Affecting Outcomes
Many things can change how well a patient does after SRS. These include the tumor’s type, size, and location, and the patient’s age and health. Younger patients with smaller, easier-to-reach tumors usually do better.
Also, new technology in SRS and imaging has made treatments more precise and effective. We will explore these factors in more detail to understand their impact on life expectancy.
By knowing these variables, doctors can give more accurate predictions. They can also tailor treatments to meet each patient’s needs. This can improve the quality of care and possibly increase life expectancy for brain tumor patients treated with SRS.
SRS for Lung Cancer: Survival Statistics and Outcomes
Stereotactic radiosurgery (SRS) is a new hope for lung cancer patients. It’s important to look at its survival stats and outcomes. This helps us understand its role in treating lung cancer.
Early-Stage Lung Cancer Treatment
In early-stage lung cancer, SRS is very effective. It’s great for patients who can’t have surgery. SRS delivers precise radiation to the tumor, protecting healthy tissue.
A study showed that SRS can help patients live up to 3 years. This is a big deal for those with few treatment options.
Metastatic Lung Cancer Management
SRS helps manage symptoms in metastatic lung cancer. It targets multiple lesions at once. This improves quality of life and can extend life.
Studies show SRS can control metastatic lesions for over a year. It’s part of a bigger plan to manage the disease, often with other treatments.
Comparative Survival Rates
Comparing SRS to other treatments, it often matches or beats them. For early-stage lung cancer, SRS survival rates are similar to surgery. For metastatic disease, SRS can improve survival.
Choosing the right treatment depends on many factors. It’s all about the cancer stage, patient health, and tumor details.
Liver and Pancreatic Cancer: Life Expectancy After Stereotactic Treatment
Stereotactic body radiation therapy (SBRT) is a new hope for liver and pancreatic cancer patients. It gives precise, high doses of radiation to tumors. This helps avoid harming healthy tissue nearby.
Primary Liver Tumors
SBRT is a good choice for primary liver tumors. It’s better than surgery for some patients. Studies show SBRT can control tumors well, improving life and quality of life.
SBRT targets tumors accurately, even in hard-to-reach spots. This is key to protecting the liver and keeping it working right.
Pancreatic Cancer Outcomes
Pancreatic cancer is tough to treat because it’s often found late. But, SBRT has shown promise in controlling tumors and possibly increasing survival. It works alone or with other treatments.
Researchers are looking into how SBRT fits into pancreatic cancer treatment. They’re testing it before surgery or to ease symptoms.
Combination Therapy Approaches
SBRT is being studied with other treatments like chemotherapy and immunotherapy. Combining therapies aims to make SBRT more effective. It targets both local and systemic disease.
For example, adding immunotherapy to SBRT might boost the immune system’s fight against cancer. Studies are checking if these combos are safe and work well.
Factors That Influence Life Expectancy After SRS
Many important factors affect how well SRS works in increasing life expectancy. Knowing these factors is key for planning treatment and predicting outcomes.
Patient Age and Overall Health
Age and health are big factors in life expectancy after SRS. Younger patients with fewer health issues usually do better. Age impacts how well the body recovers from treatment.
We look at health metrics and other medical conditions to see if SRS is right for a patient. This helps us make the treatment fit the patient’s needs.
Tumor Type, Size, and Location
The tumor’s characteristics are vital for SRS success. Different tumors react differently to radiation. The tumor’s size and location also matter for treatment success.
| Tumor Characteristic | Impact on SRS Outcome |
| Tumor Type | Certain tumor types are more responsive to SRS, such as some brain metastases. |
| Tumor Size | Smaller tumors are generally more treatable with SRS. |
| Tumor Location | Tumors in sensitive or hard-to-reach areas can be challenging to treat. |
Previous Treatments and Response
A patient’s past treatments and how they responded matter a lot for SRS. We look at how well previous treatments worked. Then, we adjust the SRS plan.
“The effectiveness of SRS can be enhanced by understanding a patient’s previous treatment history and response, allowing for a more personalized treatment approach.”
Expert Opinion
Genetic and Molecular Factors
Genetic and molecular tumor traits also affect SRS success. Some genetic markers suggest better or worse outcomes. We consider these when planning treatment.
By looking at all these factors, we create a detailed treatment plan. This plan aims to get the most out of SRS for each patient.
Comparing SRS Outcomes to Other Treatment Modalities
Looking at how SRS compares to other cancer treatments helps us understand its strengths and weaknesses. It’s important to know how SRS stacks up against surgery, radiation therapy, and chemotherapy. This knowledge helps us make better choices for cancer treatment.
SRS vs. Conventional Surgery
SRS is a non-invasive option compared to surgery. It’s great for tumors in hard-to-reach places. SRS delivers precise radiation to the tumor, protecting nearby tissue.
Surgery needs direct access to the tumor, leading to longer recovery times. But, SRS can match or beat surgery in some cases. It’s better for local control and survival rates for certain tumors.
SRS vs. Traditional Radiation Therapy
Traditional radiation therapy is spread out over many sessions. SRS gives a high dose in just one or a few sessions. This method might be more convenient and effective for some tumors.
SRS can control tumors better than traditional radiation for some conditions. But, the choice between them depends on the tumor’s size, location, and the patient’s health.
SRS vs. Chemotherapy
Chemotherapy treats cancer cells all over the body. SRS focuses on a specific area. For localized tumors, SRS offers effective control without chemotherapy’s side effects.
SRS can also work with chemotherapy in a combined treatment. This combination can improve outcomes by tackling both local and systemic disease.
Multimodal Treatment Approaches
Using SRS with other treatments like surgery, chemotherapy, and immunotherapy is becoming more common. This approach can lead to better results by combining different therapies’ strengths.
For example, SRS can treat remaining tumors after surgery or metastatic sites. Chemotherapy or immunotherapy can target cancer cells throughout the body. SRS’s flexibility makes it a key part of a complete treatment plan.
As cancer treatment advances, studying SRS and other modalities is vital. It helps improve patient outcomes and quality of life.
Quality of Life Considerations After Stereotactic Radiosurgery
After SRS, patients face many quality of life issues. These include health and daily function. As medical tech advances, knowing how SRS affects patients is key.
Neurological Function Preservation
Keeping neurological function after SRS is a big concern. SRS aims to be precise, avoiding damage to healthy tissue. But, results can differ based on the area and size treated.
Preserving neurological function helps patients stay independent. We use top-notch imaging to target accurately and reduce side effects.
Cognitive Effects and Management
Cognitive changes are a big issue after SRS. Patients might see memory, concentration, or other cognitive changes. It’s important to manage these well.
We do comprehensive cognitive assessments to track changes. Then, we use cognitive rehab, meds, or other support to help.
Pain Control and Symptom Management
Managing pain and symptoms is key after SRS. Patients might feel pain, fatigue, or nausea. We need to manage these to keep their quality of life up.
| Symptom | Management Strategy |
| Pain | Medication, physical therapy |
| Fatigue | Rest, exercise, nutritional support |
| Nausea | Anti-nausea medication, dietary adjustments |
Return to Daily Activities
Being able to do daily activities is a big part of quality of life after SRS. This depends on the patient’s health, their condition, and treatment success.
We help patients create personalized rehabilitation plans for returning to normal life. This might include physical or occupational therapy.
By focusing on these areas, we can greatly improve patients’ lives after SRS. This lets them live fulfilling lives.
Potential Complications and Their Impact on Survival
SRS is a powerful tool for treating many conditions. But, it’s important to know about the possible complications. These complications can affect how long a patient lives and their quality of life.
Radiation Necrosis
Radiation necrosis is a serious issue with SRS. It happens when the treated tissue dies from radiation damage. This can cause swelling and high pressure in the brain, leading to brain problems. Managing radiation necrosis well is key to avoiding long-term harm.
“Radiation necrosis is a serious complication that needs quick and effective treatment,” say doctors. This is to protect the patient’s quality of life.
Edema and Inflammation
SRS can also cause swelling and inflammation. This swelling can cause headaches, seizures, and brain problems, depending on where the treatment is. Corticosteroids are often used to manage swelling and reduce inflammation.
Secondary Malignancies
Another risk of SRS is getting secondary malignancies. Though rare, radiation can sometimes cause new cancers. It’s important to weigh the risks and benefits before choosing SRS treatment.
Management of Complications
Managing SRS complications involves several steps. For radiation necrosis, doctors might use medications like corticosteroids and bevacizumab. Swelling and inflammation are usually treated with corticosteroids. Regular check-ups and monitoring are key to catching and treating problems early.
As we improve SRS technology and methods, focusing on complications is vital. This way, we can make sure patients get the best care and quality of life.
Recent Advances in SRS Technology and Their Effect on Outcomes
In recent years, SRS technology has seen big improvements. These changes have made treatments better for many medical conditions, like cancer.
Improved Imaging and Targeting
One big step forward is better imaging and targeting. Today’s SRS systems use high-resolution images from MRI and CT scans. This lets doctors see tumors and healthy tissues more clearly.
Enhanced imaging means doctors can give more radiation to tumors. This helps avoid harming nearby healthy tissues. It’s key to reducing side effects and improving life quality for patients.
Dose Escalation Strategies
Dose escalation is a big focus in SRS treatment now. Giving higher doses of radiation directly to tumors can improve control and survival rates.
- Increased precision in dose delivery
- Better tumor control
- Reduced risk of radiation-induced side effects
Combination with Immunotherapy
Using SRS with immunotherapy is a new and exciting area. It aims to boost the body’s fight against cancer cells.
| Treatment Modality | Benefits | Outcomes |
| SRS Alone | High precision, effective for localized tumors | Local tumor control |
| SRS + Immunotherapy | Potential for enhanced immune response, synergistic effects | Improved survival, possible systemic control |
Adaptive Planning Techniques
Adaptive planning lets doctors adjust treatments as needed. This is important for keeping treatments effective and safe.
Adaptive SRS helps doctors adapt to changes in tumors. This ensures the best dose delivery throughout treatment.
These recent SRS technology advancements have greatly improved treatment results. They offer new hope for patients with complex conditions. As technology keeps improving, we can look forward to even better care and outcomes.
Real Patient Experiences and Outcomes
Real patient stories show how SRS changes lives for the better. By looking at how SRS works, we learn a lot. We see how it can make patients feel better and live longer.
Case Studies: Long-Term Survivors
Studies have shown SRS helps people live longer with various diseases. For example, a study on brain metastases found SRS led to better survival rates. Long-term survivors often say they feel better and can do more things without feeling sick.
Quality of Life Reports
SRS makes life better for many patients. It helps keep their brains working well and reduces side effects. This means patients can stay independent and enjoy their daily lives.
Patient Testimonials and Insights
Patient stories share their SRS experiences. Many say they feel less pain and better overall after SRS. These stories show how important SRS is for better patient care.
Lessons from Clinical Practice
Doctors have learned a lot from using SRS. They know how to pick the right patients and plan treatments carefully. Using SRS as part of a bigger treatment plan is key to better care.
Conclusion: The Future of Life Expectancy with Stereotactic Radiosurgery
Stereotactic Radiosurgery (SRS) is getting better, giving hope to cancer patients. New research and tech are making SRS more precise and effective. This could mean longer lives for those with different cancers.
Our talk showed how important SRS is for treating brain and other cancers. It delivers precise radiation, boosting survival chances and improving life quality. This is good news for many patients.
As SRS tech gets better, treatments will get even more precise. We’ll see better results as SRS works with other treatments like immunotherapy. This could lead to even better outcomes for patients.
The outlook for SRS in cancer treatment is bright. It could lead to longer, better lives for people all over the world. With ongoing advancements, patients can expect more tailored and effective treatments.
FAQ
What is Stereotactic Radiosurgery (SRS) and how does it work?
Stereotactic Radiosurgery (SRS) is a precise radiation therapy. It targets a specific area of the body. This is often for tumors and other issues.
We use advanced imaging and technology. This helps us aim at the right spot, protecting healthy tissue.
What conditions are treated with SRS?
SRS treats many conditions. These include brain tumors, metastases, and arteriovenous malformations. It also helps with trigeminal neuralgia and other neurological problems.It’s used for certain cancers too, like lung, liver, and pancreatic cancer.
How does SRS differ from conventional radiation therapy?
SRS is more precise and delivers a high dose in a few sessions. This makes it better for hard-to-reach tumors.
What are the benefits of SRT radiation?
SRT radiation is precise. This means it treats tumors well while protecting healthy tissue. This leads to fewer side effects and better results for patients.
What factors influence life expectancy after SRS?
Life expectancy after SRS depends on several things. These include the patient’s age and health, the tumor’s type, size, and location. Also, previous treatments and genetic factors play a role.We consider these when planning treatment.
How does SRS compare to other treatment modalities?
SRS is compared to surgery, traditional radiation, and chemotherapy. Each has its own benefits and drawbacks. SRS is a non-invasive, precise way to treat some conditions.We might use different treatments together for the best results.
What are the possible complications of SRS?
Complications of SRS include radiation necrosis and edema. There’s also a small chance of secondary malignancies. We work to avoid these and manage any issues that come up.
How has SRS technology advanced in recent years?
SRS technology has improved a lot. Advances include better imaging and targeting, higher doses, and combining with immunotherapy. These changes make SRS more precise and effective.
What can patients expect after SRS treatment?
After SRS, patients can usually go back to their normal activities. We aim to keep neurological function and manage symptoms. We also watch for complications and adjust treatment as needed.
What is the role of image-guided radiation therapy in SRS?
Image-guided radiation therapy is key in SRS. It helps us target tumors accurately. This technology lets us make adjustments in real-time during treatment.
How does tumor targeting impact SRS outcomes?
Targeting tumors is vital in SRS. It allows us to focus radiation on the tumor while protecting healthy tissue. This improves results and reduces risks.
References
National Center for Biotechnology Information. Stereotactic radiosurgery for brain conditions life expectancy. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5866122/