Last Updated on December 2, 2025 by Bilal Hasdemir
A breast cancer diagnosis can be overwhelming, leaving many questions unanswered. One of the critical concerns is understanding the stage of cancer and its implications for treatment. Our simple guide to the stage of breast cancer and mastectomy. Learn when it’s recommended and the critical factors that influence the decision.
Nearly 1 in 8 women will be diagnosed with breast cancer in their lifetime, and for some, a mastectomy may be a necessary treatment option. The decision to undergo a mastectomy depends on various factors, including the stage of cancer.
Recognizing the importance of early intervention is crucial for effectively managing breast cancer. At our institution, we are committed to providing comprehensive care and support throughout your treatment journey.
Key Takeaways
- Understanding the stage of breast cancer is crucial for determining the best course of treatment.
- A mastectomy may be recommended for certain stages of breast cancer.
- Early intervention plays a significant role in effectively managing breast cancer.
- Comprehensive care and support are essential throughout the treatment journey.
- The stage of cancer at diagnosis significantly influences treatment outcomes.
Understanding Breast Cancer Stages
Breast cancer staging is a critical step in understanding the disease’s progression and planning treatment. We believe in empowering our patients with knowledge about their condition, and understanding the stage of breast cancer is crucial for determining the best treatment approach.
Overview of Breast Cancer Staging
Breast cancer staging involves evaluating several key factors to understand the extent of the cancer. These factors include tumor size considerations, whether the cancer has spread to nearby lymph nodes, and whether it has metastasized to distant organs. As noted by the American Cancer Society, “The stage of breast cancer is one of the most important factors in determining the prognosis and treatment options.”
“The staging of breast cancer is a complex process that helps us determine the extent of the cancer — whether it’s localized to breast tissue or has spread beyond it.”
— American Cancer Society
Accurate staging is essential for developing an effective treatment plan. It helps us identify the most appropriate surgical options, such as mastectomy or lumpectomy, and whether additional treatments like chemotherapy or radiation therapy are necessary.
Recognizing the importance of early intervention is crucial for effectively managing breast cancer.
Accurate breast cancer staging is vital for several reasons. Firstly, it helps us understand the cancer’s extent and plan the most effective treatment. Secondly, it provides valuable information about the prognosis, helping patients and their families understand what to expect. As emphasized by a leading oncologist, “Accurate staging is crucial for making informed decisions about treatment and improving patient outcomes.”
- Tumor size and location play a significant role in determining the stage and treatment options.
- The involvement of lymph nodes is a critical factor in staging and prognosis.
- The presence of metastasis to distant organs significantly impacts the treatment plan and prognosis.
By understanding the stage of breast cancer, we can tailor the treatment to the individual’s needs, improving outcomes and quality of life. Our team is committed to providing personalized care and support throughout the treatment journey.
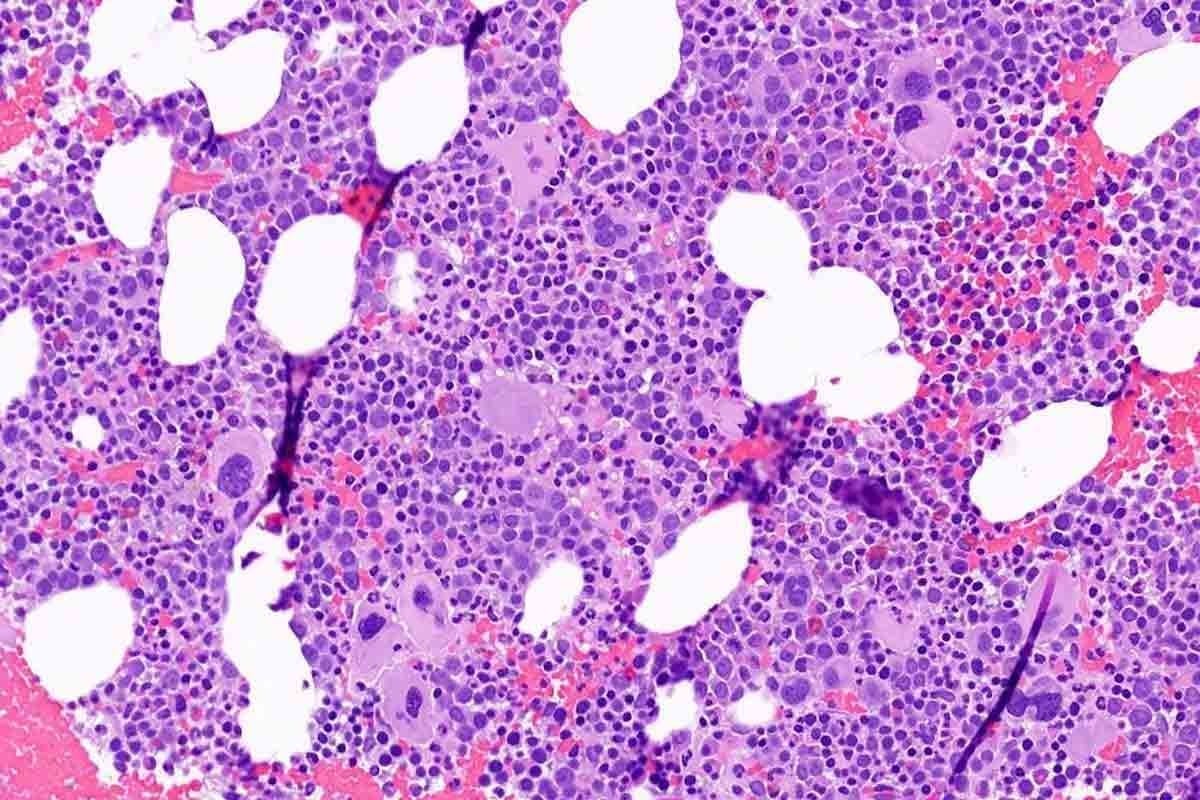
Stage 0: Ductal Carcinoma In Situ (DCIS)
At Stage 0, breast cancer is characterized by the presence of ductal carcinoma in situ (DCIS), a condition that requires careful consideration and management. DCIS is a non-invasive form of breast cancer where cancer cells are contained within the milk ducts, and it is considered the earliest form of breast cancer.
Definition and Characteristics
Ductal carcinoma in situ (DCIS) is a condition where cancer cells are confined to the lining of the milk ducts without invading the surrounding breast tissue. It is often detected during mammography as microcalcifications or densities. The characteristics of DCIS can vary; some cases may progress to invasive cancer if left untreated, while others may remain stable.
Hormone receptor status is an important factor in understanding DCIS. While DCIS cells are not invasive, determining if they are hormone receptor-positive can help in planning treatment and understanding the potential behavior of the cells.
Treatment Options for Stage 0
Treatment for DCIS typically involves surgery, which may be followed by radiation therapy in some cases. The primary goal is to remove the cancerous cells and prevent the development of invasive cancer.
- Radiation Therapy: Often recommended after lumpectomy to eliminate any remaining cancer cells.
At our institution, we work closely with patients to determine the best course of treatment for DCIS, considering factors such as the extent of the disease, hormone receptor status, and patient preferences. Our team of experts is dedicated to providing personalized care and support throughout the treatment process.
Stage I: Early Invasive Breast Cancer
At Stage I, breast cancer is considered early invasive, and patients have various surgical options to consider. This stage is characterized by a small tumor size, typically not larger than 2 centimeters, and the cancer has not spread to the lymph nodes or distant parts of the body.
How Stage I is Defined
Stage I breast cancer is divided into two subcategories: Stage IA and Stage IB. Stage IA involves a tumor that is 2 centimeters or less in diameter and has not spread to the lymph nodes. Stage IB indicates that the cancer has spread to the lymph nodes, but the nodes are not enlarged, or there are small groups of cancer cells in the lymph nodes.
Surgical Options at This Stage
For patients diagnosed with Stage I breast cancer, surgical options are often the first line of treatment. We offer two primary surgical approaches:
- Lumpectomy: This involves removing the tumor and a small margin of surrounding tissue. It’s often followed by radiation therapy to ensure all cancer cells are eliminated.
- Mastectomy: This involves removing the entire breast. In some cases, patients may opt for reconstruction surgery to rebuild the breast.
We understand that making a decision about surgery can be challenging. Our team is committed to providing you with comprehensive support and guidance throughout your treatment journey.
Stage II: Locally Advanced but Still Treatable
Stage II breast cancer represents a critical juncture in the disease’s progression, where the cancer is locally advanced but still potentially treatable with the right approach. At this stage, the tumor is larger than in Stage I, or the cancer has spread to a few nearby lymph nodes.
Characteristics of Stage II Breast Cancer
Stage II breast cancer is divided into two subcategories: IIA and IIB. In Stage IIA, the tumor is between 2 and 5 centimeters, or the cancer has spread to 1-3 lymph nodes under the arm. In Stage IIB, the tumor is larger than 5 centimeters, or the cancer has spread to 1-3 lymph nodes under the arm.
The characteristics of Stage II breast cancer can vary significantly among patients. Key factors influencing treatment decisions include tumor size, lymph node involvement, and hormone receptor status. Understanding these characteristics is crucial for developing an effective treatment plan.
Mastectomy vs. Lumpectomy Options
We work closely with our patients to determine the most appropriate surgical approach. A personalized treatment plan takes into account the unique aspects of each patient’s cancer, ensuring the best possible outcome.
Surgical Option | Description | Considerations |
Mastectomy | Removal of the entire breast | Tumor size, patient preference, genetic factors |
Lumpectomy | Removal of the tumor and surrounding tissue | Tumor size, location, need for radiation therapy |
Ultimately, the decision between mastectomy and lumpectomy should be made after thorough consultation with a healthcare team, considering all relevant factors and potential outcomes.
Stage III: More Advanced Localized Disease
At Stage III, breast cancer is considered locally advanced, necessitating a multifaceted treatment approach. This stage signifies that the cancer has grown larger or has spread to nearby tissues or lymph nodes, but not to distant parts of the body. We understand the complexity and challenges that come with a Stage III diagnosis, and our team is dedicated to providing comprehensive care tailored to each patient’s unique needs.
Understanding Stage III A, B, and C
Stage III breast cancer is further categorized into sub-stages: IIIA, IIIB, and IIIC. Each sub-stage reflects the extent of the cancer’s spread.
- Stage IIIA: The tumor is larger than 5 cm, or it has spread to lymph nodes that are clumped together or to lymph nodes near the breastbone.
- Stage IIIB: The cancer has invaded the chest wall or the skin, causing swelling or ulcers.
- Stage IIIC: The cancer has spread to lymph nodes above or below the collarbone or to lymph nodes near the breastbone.
Understanding these sub-stages is crucial for determining the most effective treatment plan.
Candidates for Mastectomy in Stage III
Mastectomy is often considered for patients with Stage III breast cancer, especially when the tumor is large or has spread significantly. We evaluate each patient to determine if mastectomy is the best option, considering factors such as overall health, tumor characteristics, and personal preferences.
“Mastectomy can be an effective treatment for Stage III breast cancer, offering the potential for removing the cancer entirely,” says one of our surgical oncologists. “However, it’s crucial to discuss all treatment options, including neoadjuvant chemotherapy and radiation therapy, to develop a comprehensive plan.”
Stage IV: Metastatic Breast Cancer
When breast cancer progresses to Stage IV, it means the disease has spread to distant parts of the body, requiring a comprehensive treatment approach. At this stage, the cancer is considered metastatic, meaning it has traveled beyond the breast and nearby lymph nodes to other organs or tissues.
Implications of Stage IV Diagnosis
A diagnosis of Stage IV breast cancer can be challenging, both emotionally and medically. The cancer’s spread to other parts of the body complicates treatment, as it is no longer confined to a single area. We understand the importance of developing a personalized treatment plan that addresses the unique needs and circumstances of each patient.
Stage IV breast cancer can metastasize to various organs, including the bones, liver, lungs, or brain. The symptoms and complications associated with Stage IV disease can vary significantly depending on the location and extent of the metastasis.
Treatment Options and the Role of Mastectomy
In most cases, a mastectomy is not the primary treatment for Stage IV breast cancer, as the disease has already spread beyond the breast. However, we may consider surgical options in certain situations to alleviate symptoms or improve quality of life.
Our team works closely with patients to develop a treatment plan that may include chemotherapy, hormone therapy, targeted therapy, or other treatments tailored to their specific condition. For some patients, particularly those with triple-negative breast cancer, treatment options may be more limited, and we focus on the most effective available therapies.
Treatment Approach | Description | Applicability to Stage IV |
Chemotherapy | Using drugs to kill cancer cells | Commonly used for Stage IV |
Hormone Therapy | Blocking hormones that fuel cancer growth | Used for hormone receptor-positive cancers |
Targeted Therapy | Targeting specific characteristics of cancer cells | Used based on cancer’s genetic characteristics |
Mastectomy | Surgical removal of the breast | Generally not primary treatment for Stage IV |
We are committed to providing comprehensive care and support throughout the treatment journey, ensuring that patients receive the best possible outcomes and quality of life.
Factors Influencing Mastectomy Decisions
Several important factors come into play when determining if a mastectomy is necessary. The decision-making process involves a comprehensive evaluation of the patient’s condition, including the characteristics of the tumor and the patient’s overall health.
Tumor Size and Location
The size and location of the tumor are critical factors in deciding whether a mastectomy is required. Larger tumors or those located in certain areas of the breast may necessitate a mastectomy.
- Tumor Size: Tumors that are large in relation to the size of the breast may require mastectomy.
- Tumor Location: Tumors located in the center of the breast or those that are close to the nipple may be more challenging to remove with a lumpectomy.
- Lymph Node Involvement: The involvement of lymph nodes can also influence the decision, as it may indicate a more advanced stage of cancer.
Hormone Receptor Status
The hormone receptor status of the tumor is another crucial factor. Tumors that are hormone receptor-positive may have different treatment options compared to those that are hormone receptor-negative.
Hormone Receptor-Positive Tumors: These tumors may respond to hormone therapy, which can be used in conjunction with or instead of mastectomy in some cases.
Hormone Receptor-Negative Tumors: Tumors that are hormone receptor-negative may require more aggressive treatment, potentially including mastectomy.
We work closely with patients to evaluate these factors and determine the best course of treatment. Our team considers the potential benefits and risks of mastectomy and other treatment options to provide personalized care.
Mastectomy Types Explained
Understanding the different types of mastectomy procedures is crucial for patients facing breast cancer surgery. A mastectomy is a surgical procedure that involves the removal of breast tissue, and it’s performed for various reasons, including treating breast cancer or reducing the risk of cancer in high-risk individuals.
” “Each patient’s situation is unique, and what works for one patient may not be suitable for another.”
Benefits and Risks of Each Type
Both total and partial mastectomies have their benefits and risks. A total mastectomy may be recommended for patients with larger tumors or those who have a high risk of recurrence. The benefits include removing all potentially cancerous tissue, which can be reassuring for some patients. However, it also involves more extensive surgery and potentially longer recovery times.
- Benefits of Total Mastectomy:
- Removal of all potentially cancerous tissue
- May be necessary for larger tumors
- Risks of Total Mastectomy:
- More extensive surgery
- Potential for longer recovery times
A partial mastectomy, while less invasive, requires careful consideration to ensure that all cancerous tissue is removed. The benefits include preserving more of the breast tissue and potentially lessening the impact on the patient’s body image. However, it may require additional treatments, such as radiation therapy, to ensure all cancer cells are eliminated.
- Benefits of Partial Mastectomy:
- Preserves more breast tissue
- Less invasive than total mastectomy
- Risks of Partial Mastectomy:
- May require additional treatments like radiation therapy
- Risk of cancer recurrence if not all cancerous tissue is removed
Reconstruction options are available post-mastectomy, offering patients the possibility of rebuilding their breast(s) using implants or their own tissue. The decision to undergo reconstruction is highly personal and depends on various factors, including the patient’s overall health and personal preferences.
In conclusion, understanding the different types of mastectomy and their implications is vital for making informed decisions about breast cancer treatment. Patients should discuss their options thoroughly with their healthcare provider to determine the best course of action for their specific situation.
The Role of Genetic Testing in Decision-Making
The role of genetic testing in breast cancer treatment is multifaceted, influencing both risk assessment and treatment choices. As we continue to advance in our understanding of genetics and its impact on cancer, genetic testing has become an indispensable tool for patients and healthcare providers alike.
Genetic testing can identify specific mutations that may increase the risk of developing breast cancer. This information is crucial for making informed decisions about treatment options, including the consideration of mastectomy.
BRCA Gene and Mastectomy Considerations
The BRCA1 and BRCA2 genes are among the most well-known genetic mutations associated with an increased risk of breast cancer. Individuals with a family history of breast cancer may be tested for these mutations to assess their risk.
- If a BRCA1 or BRCA2 mutation is identified, the risk of developing breast cancer can be significantly higher.
- Knowing the mutation status can help guide decisions about preventive measures, including mastectomy.
- Prophylactic mastectomy is sometimes considered for individuals with a BRCA1 or BRCA2 mutation to reduce the risk of developing breast cancer.
Family History and Risk Assessment
A detailed family history is a critical component of assessing the risk of breast cancer. Healthcare providers use this information to determine if genetic testing is appropriate.
- A family history of breast cancer, especially in first-degree relatives (parents, siblings, or children), can indicate a higher risk.
- The age at which relatives were diagnosed with breast cancer is also an important factor in risk assessment.
- Genetic counseling can provide individuals with a comprehensive understanding of their risk and the implications of genetic testing.
By understanding genetic predisposition and assessing individual risk factors, patients and their healthcare providers can make more informed decisions about the most appropriate treatment options.
Recovery and Aftercare Post-Mastectomy
Recognizing the importance of early intervention is crucial for effectively managing breast cancer.
Physical Recovery and Expectations
During the recovery period, patients can expect a range of physical sensations and challenges. Pain management is a critical aspect, and our healthcare team will work closely with you to develop an effective pain management plan. It’s also important to be aware of potential complications such as infection, swelling, or numbness, and to report any concerns to your healthcare provider promptly.
Some key aspects to focus on during physical recovery include:
- Following post-operative instructions carefully to minimize the risk of complications
- Engaging in gentle exercises as recommended by your healthcare team to promote healing and maintain range of motion
- Monitoring your body’s response to the surgery and reporting any unusual symptoms
Recognizing the importance of early intervention is crucial for effectively managing breast cancer.
Recovery from mastectomy is not just about physical healing; it’s also a time of significant emotional adjustment. Emotional support from family, friends, and healthcare professionals plays a vital role in helping patients cope with the psychological impact of their surgery.
“The emotional journey after a mastectomy can be just as challenging as the physical recovery. Having a strong support system makes all the difference.”
Support systems can include:
- Counseling or therapy to address emotional and psychological concerns
- Support groups where patients can share their experiences and connect with others who have undergone similar treatments
- Family and friends who can provide practical assistance and emotional comfort
By understanding what to expect during recovery and leveraging the support available, patients can navigate this challenging period more effectively. Our multidisciplinary care approach is designed to provide comprehensive support, addressing both the physical and emotional aspects of recovery.
Emotional Support for Patients
Emotional support plays a vital role in helping patients cope with the stress and uncertainty of breast cancer diagnosis and treatment. At our institution, we understand that a breast cancer diagnosis can be emotionally challenging, and we are committed to providing comprehensive emotional support and resources to help you navigate this journey.
Coping Mechanisms and Resources
Coping with breast cancer involves more than just medical treatment; it requires emotional resilience and support. We offer various resources to help you manage the emotional aspects of your diagnosis and treatment.
- Support Groups: Joining a support group can connect you with others who are going through similar experiences, providing a sense of community and understanding.
- Counseling Services: Professional counseling can help you address anxiety, depression, and other emotional challenges associated with breast cancer.
- Educational Resources: Understanding your diagnosis and treatment options can empower you to make informed decisions about your care.
Counseling Options Available
Our counseling services are designed to provide emotional support tailored to your needs. We offer individual and group counseling sessions, led by experienced professionals who specialize in supporting cancer patients.
Counseling Type | Description | Benefits |
Individual Counseling | One-on-one sessions with a licensed therapist | Personalized support, addressing specific concerns and needs |
Group Counseling | Group sessions with other breast cancer patients | Community support, shared experiences, and coping strategies |
We are dedicated to providing you with the emotional support and resources necessary to navigate your breast cancer journey with confidence and resilience.
Conclusion: Navigating Your Treatment Journey
Navigating your treatment journey requires careful planning and support. We provide the necessary information and support to make informed decisions about your care. Our team of experts, including oncologists, work closely with you to develop a personalized treatment plan.
Personalized Care and Support
We encourage you to ask questions and seek support from our team and other resources. Oncologist recommendations play a crucial role in determining the best course of treatment. In some cases, clinical trial participation may be a viable option, offering access to innovative treatments and contributing to the advancement of breast cancer research.
Empowering Informed Decisions
By understanding your diagnosis and treatment options, you can make informed decisions about your care. We are committed to delivering exceptional international healthcare with personalized VIP service and comprehensive medical support. Our goal is to empower you with the knowledge and resources needed to navigate your treatment journey confidently.
FAQ
What are the different stages of breast cancer and how are they determined?
Breast cancer staging involves evaluating the size of the tumor, whether the cancer has spread to nearby lymph nodes, and whether it has metastasized to distant organs. Accurate staging is crucial for developing an effective treatment plan.
At what stage is a mastectomy typically recommended?
A mastectomy may be recommended for various stages of breast cancer, depending on factors such as tumor size, location, and whether the cancer has spread. For stage I breast cancer, surgical options may include lumpectomy or mastectomy. For stage II and III breast cancer, treatment options may include mastectomy, chemotherapy, and radiation therapy.
What are the treatment options for stage 0 breast cancer, also known as ductal carcinoma in situ (DCIS)?
Treatment options for DCIS may include surgery, radiation therapy, or a combination of both. Our team of experts will work closely with you to determine the best course of treatment.
How does hormone receptor status affect treatment decisions for breast cancer?
Hormone receptor status is an important factor in determining the best course of treatment for breast cancer. Our team will evaluate hormone receptor status and other factors to develop a personalized treatment plan.
What are the benefits and risks of different types of mastectomy?
We will explain the different types of mastectomy, including total mastectomy and partial mastectomy, and their benefits and risks. We will also discuss reconstruction options post-mastectomy.
How does genetic testing, such as BRCA gene testing, impact mastectomy decisions?
Genetic testing can help identify individuals at higher risk for breast cancer. Our team will discuss the role of genetic testing in decision-making and help you understand your risk factors.
What can I expect during recovery from a mastectomy?
We will provide you with comprehensive guidance on what to expect during recovery from a mastectomy, including the importance of support systems and emotional support resources.
Are there any clinical trials or new treatments available for breast cancer?
Our team will discuss the latest treatment options, including clinical trials, and help you determine if they are right for you.
How can I cope with a breast cancer diagnosis and treatment?
We are committed to providing emotional support and resources to help you cope with your diagnosis and treatment. We offer counseling options and other support services to help you navigate your treatment journey.
What kind of follow-up care can I expect after treatment for breast cancer?
Our team will provide you with comprehensive guidance on long-term follow-up care, including regular check-ups and monitoring for any signs of recurrence.
References
https://www.mayoclinic.org/tests-procedures/mastectomy/about/pac-20394670